William Kingston
Dublin, Ireland
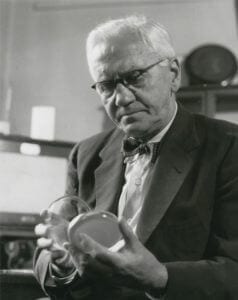
Alexander Fleming Laboratory Museum (Imperial College Healthcare NHS Trust)
The discovery of antibiotics has been described as the “domestication of microorganisms” and ranks in importance with the domestication of animals as part of settled agriculture about 10,000 years ago. It depends upon antagonism between bacteria, which had been noticed as early as 1874, and Pasteur commented then that if we could learn how to intervene in this antagonism, it would offer “perhaps the greatest hopes for therapeutics.”1
Penicillin
These hopes began to be realized when an experiment went wrong for Alexander Fleming of St. Mary’s Hospital, Paddington, London, in 1928, and the story is one of near-incredible coincidences and chances. After being away on holiday, he noticed that the growth of bacteria he had left to culture had been stopped by accidental contamination by a mold. He was about to discard the culture, when a colleague pressed him to investigate it further.2 The offending mold proved to be penicillin, which he studied as best he could, but found to be highly unstable. Consequently, after publishing a paper in which he called attention to its possible therapeutic potential, he abandoned work on it.3
Nothing more happened until 1935, when an Australian, Howard Florey, became Professor of Pathology in Oxford. With backing from the Rockefeller Foundation, he was able to recruit Ernst Chain to introduce the new discipline of biochemistry to the University. (Chain had been a Professor in Berlin, but had to flee from Nazi persecution of Jews). They agreed that the research would begin by studying an earlier discovery of Fleming’s, lysosyme. Florey obtained a grant of £250 (about $1,000 at the time) from the Rockefeller Foundation for this, and as Foundation officials later observed, “seldom has so small a contribution led to results so momentous.”4
In searching the scientific literature with Fleming’s name in mind, it was inevitable that Chain would come across his 1929 paper. As there was a sample of the mold in Oxford, with resources that had not been available to Fleming, he was able to demonstrate and publish the extraordinary power of penicillin to deal with a wide range of bacterial infections.5 Some progress was also made towards getting the substance under control.
Even though it was clear that World War II would generate a great need for penicillin, the resources required for its production were just not available in Britain. Florey therefore obtained permission from the authorities to seek help in the United States, where he succeeded beyond anything that could have been hoped for. The steps taken there led to there being enough penicillin to treat all the Allied wounded in the D-day landings and afterwards. The US authorities said later that “this saved as many lives, and mitigated as much suffering, as the war cost us.”6
Streptomycin
Unfortunately, one disease on which penicillin had little effect was tuberculosis. Nevertheless, it was directly due to its innovation that the second founding drug of the antibiotic revolution, streptomycin, which could treat it, was discovered. The process whereby this came about could not have been more different from that of penicillin, and the key individual, Selman Waksman, was not even in the medical field. He was a microbiologist in Rutgers University, New Jersey, and since his arrival in the United States from Russia as a student, he had specialized in the study of actinomycetes, bacteria that live in the soil.
Merck had already funded research by Waksman, and they were also involved in the American production effort for penicillin. As well as this, they knew about remarkable clinical successes with this drug that Drs. Dawson and Hobby were having in New York (and which eventually led these two to another big advance, which was the ability to administer penicillin orally).
Merck consequently funded investigation of Waksman’s collection of actinomycetes for antibacterial qualities, and within a few months, streptomycin had been discovered.7 Soon afterwards, researchers from the Mayo Clinic found it was amazingly powerful against tuberculosis. In the nine years from 1950, for example, the death rate of children from this disease in Western countries was reduced by no less than 90%.
Fleming’s Crucial Experiment

Fleming had been commissioned to write the chapter on staphylococci in a British Medical Research Council’s nine-volume compendium on bacteriology, which made him alert to scientific papers with this word in their title. In 1927, such a paper appeared from researchers in Trinity College, Dublin.8 Having read it, Fleming, as a good scientist, replicated the experiment to confirm the authors’ findings. Reverting to Fleming, why was he doing that particular experiment, and how did it go wrong for him?
But how did it go wrong? Charles la Touche, a mycologist, was researching a theory that asthma was caused by proximity to cobwebs, and had filled a laboratory in St. Mary’s with a collection of these. Later research showed that this was the only possible source of the contaminating penicillin.9 Interestingly, in the days before scientific medicine, a common treatment for an infected wound was to place a cobweb on it, and it is plausible that those who did this were treating the wound with penicillin without knowing it.
The crucial element in the Bigger, Boland, and O’Meara paper was an instruction to culture the bacteria at room temperature instead of incubating them. The importance of this for Fleming’s experiment is that penicillin does not kill bacteria, but acts on their cell walls as they are dividing, and so prevents their growth. This was why Fleming and his small team found it so difficult to handle, and in fact they were never able to repeat the original experiment, because they kept trying to use penicillin against fully-grown bacteria. If the staphylococci in Fleming’s experiment had been cultured by incubation instead of at room temperature, they would have grown so rapidly that la Touche’s penicillin mold would have been overwhelmed by them. A final twist to the story is that neither Bigger nor La Touche ever learned of the parts they had played in the discovery of penicillin, even though Bigger later did important work on resistance of bacteria to it.
Chance
Did the antibiotic revolution have to happen in the way just described? Indeed, did it have to happen at all?
Perhaps the best known of Pasteur’s obiter is that “in matters of observation, fortune favours only the prepared mind.” Fleming’s mind was prepared because he had earlier discovered lysosyme in mucus in his nose when he had a cold. He had hopes that this would have antibacterial quality, but was disappointed by its weakness. Nevertheless, without his experience of it, he might not have been sensitive to what was on his petri dish in 1928. It was also because Florey and Chain set out to study lysosyme that Chain was led to Fleming’s paper on penicillin. How low must be the chances of such a sequence of events?
Coincidences

Even more improbable must be the coincidence in time of Fleming’s commission from the Medical Research Council for a chapter on staphylococci and the appearance of the Bigger, Boland, and O’Meara paper with a similar topic in its title. Then add to the odds against this, the proximity of la Touche’s cobwebs, and that within his collection the one which escaped and contaminated Fleming’s experiment was unique: “Fleming’s strain had the ability to produce penicillin at a level that put it in a class of its own, and it was one so rare that it would have been most unlikely to be rediscovered.”6 To all of these unlikely elements in what happened must also be added that Fleming felt that without Merlin Pryce’s suggestion, he would not have given the crucial petri dish a second look. Also, his holiday period was exceptionally cold for the time of year. Had it not been, even though the bacteria in his experiment were not being incubated, they might still have grown too fast for the accidental penicillin contamination from la Touche’s cobweb collection to cope with them.
And what about the chances of the right individuals coming at the right time, in the right place? In the Oxford work, the contribution of Norman Heatley in designing and building the equipment needed at a time of wartime shortages was crucial. It was he who developed the system of dosage measurement for penicillin that remains the worldwide standard. But Florey was the real hero of the story. He wore himself out traveling all over the United States trying to get the major drug firms to take up the production of penicillin — “made to feel like a carpet-bag salesman trying to promote a crazy idea for some ulterior motive,” as he put it.10 When enough of the drug had become available for the campaign in North Africa, the army doctors refused to use it, so Florey himself went to the battlefields to persuade them.
Missed chances
The chances that were missed also need to be taken into account. Not long after Fleming’s paper was published, Roger Reid, a student in Penn State University, approached him and obtained a sample of the mold. Although he wrote two papers on it, his Professor dissuaded him from doing his doctorate on penicillin.11 Waksman later noted that several times in his own research, an instance of bacteriological antagonism was on the laboratory bench in front of him, but he had failed to recognize it. One such case was in 1923, five years earlier than Fleming. There can be no doubt that Professor Gratia of Liege also anticipated Fleming, although he did not take his experiment forward. And then, tellingly, there was izoniazid (INH), which was so powerful that it could even substitute for streptomycin against tuberculosis. This had been synthesized as long ago as 1912, but its effectiveness was not demonstrated until the firms of Bayer, Hoffmann-la-Roche, and Squibb all did this independently in 1951.12 Without the previous penicillin-streptomycin history and stimulus, would its importance and value ever have been recognized?
To the professionals who calculate chances, the probability of independent events occurring simultaneously is the product of their individual probabilities. Thus, if each of two separate events has a chance of happening of 1 in 5, the chance of their both happening together is 1 in 25. When the odds against each of the components discussed above are put together in this way, their product quickly goes beyond even the most vivid imagination’s ability to capture. We are, quite literally, incredibly lucky to be the beneficiaries of the antibiotic revolution.
References
- Waksman S.A., The Antibiotic Era, citing a Royal Society Note by William Roberts. (Tokyo, The Waksman Foundation of Japan, 1975).
- Brown K, Penicillin man: Alexander Fleming and the Antibiotic Revolution. Citing personal communication from Merlin Pryce. (2004, Sutton Publishing, Stroud).
- Fleming A, ‘On the antibacterial action of cultures of Penicillium, with special reference to their use in the Isolation of B. influenzae.’ Br J Exp Pathol 10: (1929) 226–236.
- Rockefeller Foundation. Extract from Trustees’ Bulletin (1943) October.
- Chain E, Florey H et al. ‘Penicillin as a chemotherapeutic agent.’ Lancet 24: (1940) 226–228.
- MacFarlane G, Howard Florey: the Making of a Great Scientist. (1979, Oxford, Oxford University Press).
- Schatz, A, Bugie, E,. Waksman, S, ‘Streptomycin, a substance exhibiting antibiotic activity against Gram-positive and Gram-negative bacteria.’ Proc Soc Exp Biol Med 55:(1944) 65–69.
- Bigger, JW., Boland, C, O’Meara, R A Q., ‘Variant colonies of Staphlococcus aureus’. J Pathol Bacteriol 30 (1927) 261–268.
- Hare, R, The Birth of Penicillin, Chaps 3 and 4. (1970, London, George Allen and Unwin);
- Williams T I. Howard Florey: Penicillin and After. (1984, Oxford, Oxford University Press).
- Hobby, GL., Penicillin: Meeting the Challenge. (1985, New Haven, Yale University Press).
- Waksman, S.A., The Conquest of Tuberculosis. (1964, Berkeley, University of California Press).
WILLIAM KINGSTON, LittD is a retired associate professor (Innovation) from Dublin University, author of six books and numerous articles on this subject, and director of several major research projects funded by the European Union, the US National Science Foundation, European Patent Office, etc. His interest in the subject of this essay was sparked by finding out that the discovery of penicillin was a direct result of research in his own university, of which his medical colleagues were unaware. Author’s original research was published in Research Policy 29 (2000) pp. 679-710 and Journal of the History of Medicine and Allied Sciences 59 (2004) pp. 441-462.
Highlighted in Frontispiece Summer 2014 – Volume 6, Issue 3

Leave a Reply