Richard Zhang
Philadelphia, Pennsylvania, United States
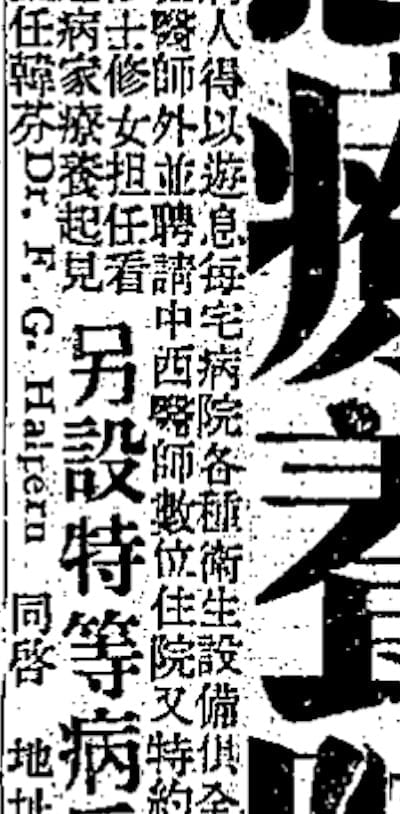
On September 20, 1935, a lengthy advertisement in one of Shanghai’s most popular newspapers, the Shen Bao, celebrated the recent opening of the Shanghai Puci Sanatorium (上海普濨療養院).1 The sanatorium would later be known in Western histories as The Mercy Hospital for Nervous Diseases. The advertisement lauded the Puci Sanatorium, headed by director Lu Bohong, for treating psychiatric patients at a time when very few local institutions cared for them. It noted the restful environment, with many flowers and trees, and its high-quality modern utilities such as telephones and electricity. Admissions occurred by walk-in or appointment, and family members could visit patients or even stay on-site.
The advertisement also portrayed therapies and personnel at the sanatorium as modern and international.2 For conditions such as neurasthenia, which was associated with insomnia and fatigue, treatments included the “latest medications” and targeted the root cause of patients’ symptoms. Roman Catholic monks and nuns from France, Germany, and the United States were included among the caregivers. The advertisement also mentioned a “Dr. F.G. Halpern” as director of medical affairs. Dr. Halpern was a famous Austrian Jewish psychiatrist who helped translate and adapt the notion of mental hygiene in Shanghai.
Fanny-Gisela Halpern was born to military surgeon Simon Halpern and Rosalie Halpern in Krakow, then part of the Austro-Hungarian Empire, on August 1, 1899.3 She studied medicine at the University of Vienna, graduating in 1924. After working with Nobel laureate psychiatrist Julius Wagner-Jauregg and several other notable researchers in Vienna, in 1933 Fanny Halpern was invited by the president of the National Medical College of Shanghai, Yan Fuqing, to work as a professor of psychiatry and neurology. She collaborated with local medical and business elites to teach trainees and expand access of care to Shanghainese with mental health conditions. Very few institutions existed in the first half of the 1930s to care for the city’s psychiatrically ill.4,5
The 1935 founding of the Puci Sanatorium was a collaborative effort between Dr. Halpern and local elites. This project epitomized Shanghai’s international diversity and the selective incorporation of biomedical ideas during the Republican period. The two most crucial figures behind the institution’s founding and shaping, Dr. Halpern and Lu Bohong, had dramatically different but complementary backgrounds.6 Neuropsychiatrist Dr. Halpern envisioned a vast “mental hygiene” network of mental hospitals, psychotherapy clinics, and special schools that would “correct social maladjustments” early on and treat “members of all nations and of all classes of society” suffering from psychiatric conditions. Chinese businessman, local philanthropist, and staunch Roman Catholic Lu Bohong (alternatively transliterated as Lo Pa-Hong) collaborated with local government in Shanghai to fund a psychiatric institution that would be medically charitable, beneficial for public security, and partly evangelical in mission. Dr. Halpern inspired the businessman to fund the creation of a hospital that could offer preventative and longitudinal psychiatry services, as well as treat those with advanced mental health conditions. This was in contrast to Lu Bohong’s initial vision of an asylum that primarily admitted the severely mentally ill.
Mental hygiene (xinli weisheng: 心理衛生) was originally a Western biomedical concept.7 It had originated in the United States in the early 1900s and promoted early, preventative, and systematic measures among Euro-Americans to address risk factors for mental health conditions. In the West it embodied two impulses: humanitarian concern for the wellbeing of people with mental health conditions, and an authoritarian desire for public order and control. Similarly in Republican China, mental hygiene was supported by physicians and caregivers largely out of interest in humane treatment of the mentally ill, and by educators and social scientists as a means of advancing Chinese self-strengthening, political unity, and nationhood as a whole. Elites’ interest in this concept was similar to their interest in using public sanitation to boost national image. The latter had largely arisen from decades of Europeans’ condescending justification of military intervention in Qing China due to a perceived lack of sanitation and thus backwardness.8
Yet, the incorporation of mental hygiene as envisioned by Dr. Halpern in Shanghai was not an uncontested, unmodified, cross-cultural diffusion of biomedical knowledge. Her vision for a mental hospital system relied on the intersection of powerful Chinese social reform and evangelical interests to be realized. This was also evident in the fact that later mental hygiene-promoting “child guidance clinics” targeted poorly-behaving street and refugee children, who were popularly associated with criminal behavior in the city.9 Furthermore, not all forms of psychotherapeutic knowledge practiced by Dr. Halpern’s Shanghai Mental Hygiene Association were received equally well by Chinese patients; for instance, medical missionary Charles Hart Westbrook’s form of experimental psychology appealed more than abstract Adlerian psychology.10 Biomedical knowledge was filtered through selective Chinese interests in psychology and therapeutic concerns, making its translation locally contingent. Nonetheless, this shared vision of mental hygiene was pivotal, especially in the creation of the Puci Sanatorium.
Halpern was cognizant of both local circumstances modifying the translation of mental hygiene and the risks of Orientalism among Western observers. For example, in November 1935 she described Freudian psychoanalysis at a Chinese medical conference as a lower-priority component of mental hygiene in Shanghai, based on the poor quality of general psychiatric facilities.11 Dr. Halpern’s exchanges were also bidirectional, as during the opening ceremonies of the Puci Sanatorium when she spoke to a Eurocentric audience, “It seems evident that there is no difference between the European and Oriental minds. The causes of nervous breakdown here and in Europe are similar [and] our treatment here is the same as it was in Vienna.”12 Although she was not a native Shanghainese elite, and would not work in European psychiatry for most of the 1930s, she was a key linkage between the two groups.
Halpern was a twentieth-century example of an epistemic “go-between.” In The Brokered World, historian Simon Schaffer and others describe such go-betweens: historical intermediaries who were situated “between worlds” and articulated “relationships between disparate worlds or cultures by being able to translate between them.”13 Eroding notions of center and periphery, these go-betweens interacted with their connected actors to facilitate new knowledge production rather than passively diffuse it. Although the book focuses on interpreter-translators, knowledge brokers, and other go-betweens in settings between 1770 and 1820, a time of increasing cross-cultural interactions worldwide, the framework may also be connected to the medical marketplace of Republican China. Cosmopolitan cities like Shanghai and Beijing saw substantial interactions between Euro-American and Chinese medical practitioners, especially in medical schools and hospitals like the Puci Sanatorium.14,15
As the world continues to become more interconnected, and biomedical care becomes more accessible worldwide, it is crucial to understand the intermediaries who make such expansion possible. Such agents, often healthcare professionals or entrepreneurs limited in capital and visibility, can benefit from the public’s awareness about them.16 How do these go-betweens help adapt biomedical ideas to new cultural and economic circumstances? Who are the moneyed and influential agents with whom they can collaborate? By examining remarkable go-betweens like Dr. Fanny Halpern, historians of science and medicine can better imagine and articulate how cross-cultural translation of medical knowledge in the future should take place.
References
- “Shanghai puci liaoyangyuan zhuanzhi jingshen shenjingbing kaizhen qishi”上海普濨療養院專治精神神經病開診啟事 [Opening of the Puci Sanatorium for Nervous Diseases]. Shen Bao 申報. September 20, 1935.
- Ibid.
- Triarhou, Lazaros C. “Women Neuropsychiatrists on Wagner-Jauregg’s Staff in Vienna at the Time of the Nobel Award: Ordeal and Fortitude.” History of Psychiatry 30, no. 4 (December 1, 2019): 393–408.
- “Shanghai fengrenyuan” 上海瘋人院 [Shanghai Insane Asylum]. Shen Bao. April 17, 1934.
- Wang, Wen-Ji. “An International Teamwork: Mental Hygiene in Shanghai During The1930s and 1940s.” History of Psychology 22, no. 4 (2019): 289–308.
- Ibid.
- Baum, Emily. “Healthy Minds, Compliant Citizens: The Politics of ‘Mental Hygiene’ in Republican China, 1928–1937.” Twentieth-Century China 42, no. 3 (2017): 215–33.
- Rogaski, Ruth. “Health and Disease in Heaven’s Ford.” In Hygienic Modernity: Meanings of Health and Disease in Treaty-Port China, 1:48–75. Berkeley, CA: University of California Press, 2004.
- Wang, “An International Teamwork,” 289-308.
- Ibid.
- “Women Neuropsychiatrists.” 393-408.
- Baum, Emily. “Spit, Chains, and Hospital Beds: A History of Madness in Republican Beijing, 1912-1938.” Ph.D. dissertation, UC San Diego, 2013.
- Schaffer, Simon, Lissa Roberts, Kapil Raj, and James Delbourgo. “Introduction.” In The Brokered World: Go-Betweens and Global Intelligence, 1770-1820, 1:ix-xxxviii. Sagamore Beach, MA: Watson Publishing International LLC, 2009.
- Rose, Anne C. “Racial Experiments in Psychiatry’s Provinces: Richard S Lyman and His Colleagues in China and the American South, 1932–51.” History of Psychiatry 23, no. 4 (2012): 419–36.
- “An International Teamwork,” 289-308.
- Lim, Yee Wei, and Audrey Chia. “Social Entrepreneurship: Improving Global Health.” JAMA 315, no. 22 (June 14, 2016): 2393–94.
Image Citation
- Beijing Airusheng shuzihua jishu yanjiu zhongxin 北京爱如生数字化技术研究中心. Shenbao shujuku 申報數據庫 [Shen Bao Database]. Beijing: Beijing Airusheng shuzihua jishu yanjiu zhongxin, 2011.
RICHARD ZHANG is an MD/MA student completing his medical studies at Sidney Kimmel Medical College at Thomas Jefferson University, and his MA in History of Science and Medicine at Yale University.

Leave a Reply