Daniel Gelfman
Indianapolis, Indiana, United States
Sir Thomas Lewis (1881–1945) has been called one of the “fathers of modern cardiology” due to his many significant contributions to that discipline. In 1930 he wrote a landmark paper clarifying the disease “congestive (heart) failure,” revealing clues that are present in the jugular veins, for making the diagnosis and judging the severity of this disease.1 His contribution to the understanding of heart failure is now still remembered.
Our current understanding of congestive heart failure developed over centuries. Patients with heart failure generally start with shortness of breath on exertion, sometimes associated with chest discomfort, progress to symptoms with minimal exertion, and then finally have symptoms at rest. There is often cough and sometimes blood-tinged sputum. There is also a gradual development of edema, following the effect of gravity, which starts in the legs and progresses higher in the body. Before treatment was available, patients would essentially drown internally as their lungs filled with fluid. Treatments in the early 1900s included therapies with limited effectiveness such as digitalis and bloodletting. Later in the twentieth century, treatments improved and progressed to include heart transplantation.
In order to develop and gauge the effectiveness of treatment, it was important to diagnose congestive heart failure early in the course of the disease. Recognizing findings on examination required advances in understanding the pathophysiology of heart failure.
Lewis was an exceptional scientist, clinician, and medical educator who had studied the pathophysiology of heart failure. He was aware that the pressure inside the heart, called the central venous pressure, normally increased some when needed to improve the ability of the heart to pump; however, this compensatory mechanism had limitations. When the heart fails, the central venous pressure becomes too high. The pressure in the peripheral veins is excessive as well, as all veins drain into the heart. Lewis and others recognized that the buildup of edema throughout the body was due to the high pressure in the venous system resulting in fluid leaking into the tissues from the thin-walled capillaries that drain into the veins. The fluid would accumulate in the lungs (pulmonary edema) or in the rest of the body (peripheral edema). Congestive heart failure is excessive fluid in these tissues due to inadequate function of the heart.
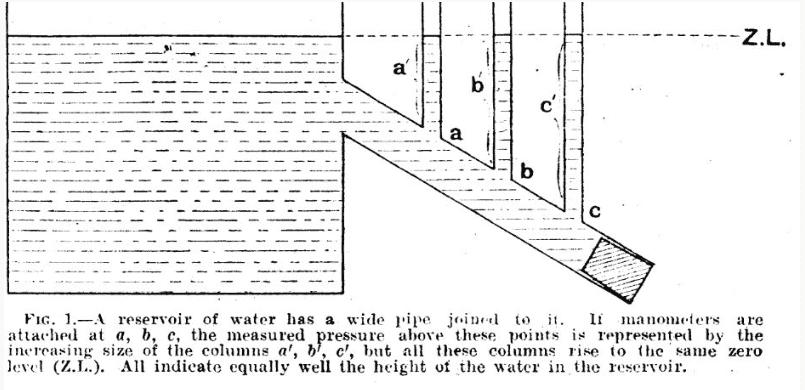
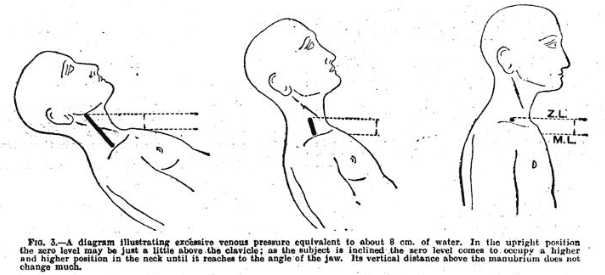
Dr. Lewis studied the treatment of patients with congestive heart failure by measuring the pressure in the peripheral venous system, as the central venous pressure could not be directly measured at that time. He then measured the pressure in the veins of the arm at the level of the heart to closely estimate the pressure inside the heart. He found indeed that lowering the venous pressure with treatment would result in patients breathing easier and having less edema.1 Being an analytical thinker and astute observer, he recognized that the height of the visible bulging jugular veins in the neck, being above the heart, was dependent on the central venous pressure inside the heart.1 He compared the heart and the whole venous system to that of a reservoir of water: as it fills and its internal pressure goes up, any tube connected to the reservoir would have the same pressure and the same level of filling as the reservoir itself (figure 1). The jugular veins behaved like those tubes connected to the reservoir. So, as the central venous pressure in the heart increased, the visible vertical height of the jugular veins rose. He realized that if the jugular veins were distended above the clavicle in the upright position, the central venous pressure in the heart itself was excessive and patients were developing “congestive failure,” a term he proposed. And he found that distended jugular veins above the clavicle (figure 2) on physical examination was the earliest sign of heart failure.
Over the next several decades, the treatment of congestive heart failure advanced, and there became a need to know the central venous pressure accurately. This ability became clinically available in the 1940s, although it took decades to be commonly available. Physicians needed a way to closely estimate this central pressure on physical exam.
Dr. Lewis stated, (but never published),1,2 that the anatomic region called the sternal angle (figure 2) was about five centimeters above the right atrium, the area where central venous pressure originated in any patient position. Thus, one could measure the vertical height of the jugular veins above this anatomical point and add five centimeters to this to roughly estimate the central venous pressure in the heart. This was called, by others, the “Lewis Method” and it was useful for the treatments available during Lewis’ life, but it was not precise enough for what physicians needed in the future, varying much between different positions and patients.3,4
Although Lewis didn’t write about it, we know that he made the statement about the relationship of the sternal angle to the right atrium from several sources. The “Lewis Method” appears in an article published by Paul Allen in 1948 describing “an instrument for venous pressure estimations” that added “the 5-centimeter constant of Lewis.”5 In 1957, the famous British cardiologist and student of Lewis, Paul Wood, made an instructional video available in the Wellcome Collection. He said Lewis had made the statement concerning the sternal angle as a good reference point “because this was about 5 cm above the center of the right atrium.” But Wood did not say anything about Lewis using this to precisely measure central venous pressure. Lewis did write about estimating central venous pressure qualitatively using words such as “normal,” “raised a little,” and “Where pressure is higher still, the veins remain throughout the neck when the head and shoulders are lifted off the bed.”1
Given Lewis’ accomplishments in teaching medicine, it is appropriate to remember him by renaming this technique to possibly, “the Lewis method for recognizing an elevation in the central venous pressure.” This was his message in 1930. It was invaluable for recognizing heart disease and the limited treatments available at the time, and it is still valuable for recognizing heart disease today.
Bibliography
- Lewis T. Remarks on Early Signs of Cardiac Failure of the Congestive Type. Br Med J. 1930;1(3618):849-852. doi:10.1136/bmj.1.3618.849
- Lewis T. Diseases of the Heart. 4th ed. The Macmillan Company; 1946.
- McGee SR. Physical examination of venous pressure: A critical review. Am Heart J. 1998;136(1):10-18. doi:10.1016/S0002-8703(98)70175-9
- Seth R, Magner P, Matzinger F, van Walraven C. How Far Is the Sternal Angle from the Mid-right Atrium? J Gen Intern Med. 2002;17(11):861-865. doi:10.1046/j.1525-1497.2002.20101.x
- Allen P. A Standardization of the Lewis Method of Venous Pressure Estimation. Can Med Assoc J. 1948;59(6):560-565.
DANIEL GELFMAN, MD, FACC, FACP, is a Clinical Professor Emeritus of Medicine (Cardiology) at The Marian University College of Osteopathic Medicine. He remains active teaching clinical medicine, working as a volunteer physician, and pursuing scholarly activities at Marian University. His research interests currently include developing effective teaching methods and combining the humanities with medicine. Recent publications include, The David Sign, published in JAMA Cardiology, and The importance of “The David Sign”, published in Hektoen International, which reveal and discuss previously unrecognized illustrations of cardiovascular physiology in Michelangelo’s sculptures.

Leave a Reply