Jack Coulehan
Stony Brook, New York, United States
 |
| Clinicians in Intensive Care Unit. 2011. Photo by Calleamanecer. Via Wikimedia. CC BY-SA 3.0 |
I want to reflect on the role of emotions, or “sensibility of heart,” in medical judgment. I take the term “judgment,” in general, to refer to the human capacity of assessing, analyzing, and reaching a conclusion with regard to any point or course of action. Any specific conclusion reached by this process may also be termed a “judgment.” We make judgments every day when we form opinions about politics, decide what groceries to buy, and give advice to our grandchildren. In every case there is an element of uncertainty involved. We might feel certain about our judgments, but they are usually based on incomplete knowledge. In medical practice it is useful to consider two broad categories: clinical judgment, which is the capacity to make decisions about diagnosis, prognosis, and treatment of illness, as well as the personal characteristics and life experience of patients; and moral judgment, which involves making decisions based on the physician’s moral values.
At bottom, these two categories of judgment largely overlap. My concern here is the role of the physician’s own emotions (or, as we like to say in medicine, in order to sanitize them, affects) in judgments of either category. Do the physician’s own emotional responses contaminate her judgment when making clinical or moral decisions in patient care? Or, rather, do her emotional states constitute essential components of medical judgment?
Clinical judgment
Medicine has a long tradition that attributes a special quality to the diagnostic and therapeutic thought processes of good clinicians, an attribute independent of intelligence or medical knowledge. Traditional views of clinical judgment included personal experience, received knowledge in the profession, and evidence from empirical studies. Emphasis was put on developing the “clinical eye” or clinical intuition as a result of personal experience, perhaps guided by role model physicians. In 1967 the Yale clinician and epidemiologist Alvan Feinstein published his book, Clinical Judgment, which was the first (as far as I am aware) systematic and scholarly analysis of judgment in medicine.1 What Feinstein added to the mix was a firm grounding in epidemiological methodology; notions like prevalence, sensitivity, specificity, and predictive value. What constituted evidence became more scientific and less subject to bias. However, Feinstein acknowledged the important influence of a personal relationship with the patient in good clinical judgment.
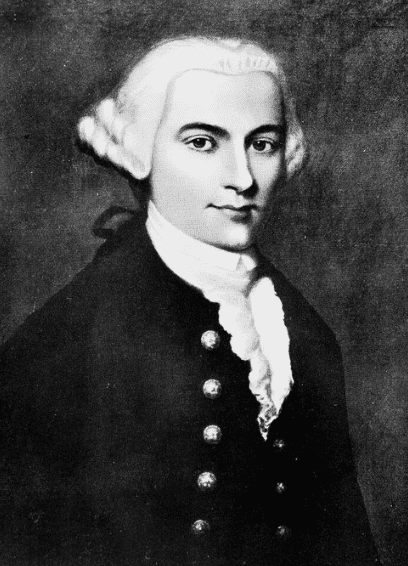 |
| Thomas Percival from Sketches of the lives and work of the honorary medical staff of the Manchester Infirmary: from its foundation in 1752 to 1830 when it became the Royal Infirmary / [Edward Mansfield Brockbank]. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0) |
In this sense he was following a tradition that has been prominent among physician writers for over 250 years and was often expressed metaphorically by reference to the heart. For example, John Gregory, professor of medicine at the University of Edinburgh wrote in 1772: “Of the physician’s character, the chief quality is humanity, the sensibility of heart that makes us feel for the distress of our fellow-creatures, and which, in consequence, incites us . . . to relieve them.” Physicians “by being daily conversant with scenes of distress, acquire that firmness of mind so necessary in the practice of physic.”2 Yet he warned his readers to maintain “a gentle and humane temper” because “rough and blustering manners generally accompany a weak understanding and a mean soul.”2 In 1803 Gregory’s student, Thomas Percival, instructed physicians to, “Unite tenderness with steadiness in your care of patients and cultivate the tender charity that the moral practice of medicine requires.” He warned his readers that medical practice makes the practitioner vulnerable to “coldness of heart,” and he concluded: “This coldness of heart, this moral insensibility, should be sedulously counteracted before it has gained an invisible ascendancy.”3
Physicians reiterated this dynamic throughout the nineteenth century. Morril wrote that “the study of medicine has a peculiar tendency to harden the disposition,” which makes it incumbent on students to cultivate “an affectionate sympathizing spirit,” while Jones reflected on medicine’s “manifest tendency to harden and corrupt the heart.”4 And famously, in his 1889 graduation address at the University of Pennsylvania, William Osler encouraged the graduates to cultivate the virtue of “aequanimitas,” which would assist them in meeting “the exigencies of practice with firmness and courage without, at the same time, hardening the human heart by which we live.”5
In the early twentieth century, Francis W. Peabody, chief of the Harvard medical service at Boston City Hospital, published an influential description of this tension between the “intensely personal” values needed in caring for patients and the “entirely impersonal” aspects of treating disease. Peabody recognized that the hospital setting creates a hostile environment for humanism, but urged students to commit “time, sympathy, and understanding” to creating a “personal bond” with their patients, which will make them more effective healers, as well as give them personal satisfaction.6 This tradition was most recently and eloquently summarized in A Flag in the Wind, Thomas Inui’s now-famous report to the American Association of Medical Colleges (2003).7 Each of these writers emphasized the importance of tenderness or sensibility of heart, while warning students and practitioners against the tendency of medical practice to chill, harden, or corrupt the heart.
A second tradition, almost diametrically opposed to the first, experienced a growth spurt in the mid-twentieth century and has become the most prominent model for medical education and practice in recent decades. In terms of diagnosis and therapy, the ascendency of randomized clinical trials, statistical techniques for the metanalysis of multiple studies, evidence-based medicine, algorithms, and clinical decision rules has progressively reduced the role of judgment in medicine because decisions are presumably to be based on complete, rather than incomplete, knowledge. Judgment is to be replaced by decision rules that can be applied without the adverse influence of spooky elements like intuition, biases, experience, emotion, or idiosyncratic beliefs.
In tandem with this, the doctor’s proper stance toward her patient became detachment rather than personal engagement, and the doctor’s emotions became stumbling blocks rather than beneficial to care. This tradition holds that emotional experience decreases objectivity, which harms the patient because it compromises clear thinking and harms the physician because it makes her vulnerable to emotional stress, depression, and burnout. In summary, what was once a pernicious tendency to harden the heart is no longer considered pernicious, but rather a positive development that should be fostered by medical education.8-11 Clinical judgment, according to this tradition, should ignore the heart and focus exclusively on the mind.
Moral judgment
Medical morality originated in ancient writings from Greece, India, and China that specify the personal traits and moral duties of medical practitioners. These documents include such duties as honoring their teachers, acting in their patient’s best interests, and keeping “whatever I shall see or hear in the course of my profession” confidential. These admonitions were later incorporated into a Judeo-Christian-Islamic framework that added a theological dimension (e.g. respect for human life, compassion, fidelity, and vocation) to medical morality—for example, in the Oath of Maimonides: “May I never see in the patient anything but a fellow creature in pain.” Or, in the Islamic oath, “I swear by God to be . . . an instrument of God’s mercy.” This work was secularized in the eighteenth and nineteenth centuries by writers who adapted Aristotelian virtue theory to the profession. The basic idea, then, was that learning to be a physician involved a process of character formation in which certain defining virtues were incorporated as personal traits or qualities, thus enabling physicians to make correct moral judgments in their professional lives.
This work was brought up to date in recent decades by philosophically-minded physicians like Edmund Pellegrino12 and Eric Cassell,13, 14 who argue that judgment in medicine should be an instantiation of the Aristotelian intellectual virtue called phronesis, or practical wisdom.9 They remind their readers of the moral goals intrinsic to the profession, and that certain physician character traits or virtues further those goals, e.g. compassion, fidelity, integrity, courage, humility, and self-improvement. They argue that, in fact, all clinical judgment is informed by moral judgment.
Although moral judgment was thought essential in deciding what to do for patients, it was proscribed in making decisions about the intrinsic value of patients. The ethos of medicine strongly warns against judging the patient’s personal worthiness or value, even if the physician considers his beliefs or actions hateful. Thus, professional ethics dictates that you remain detached from any behavior that would compromise treatment of enemy soldiers, criminals, terrorists, or patients that you find personally hateful or disgusting.
Beginning in the 1960s and 1970s, the professional virtue tradition was supplemented by (or challenged by, depending on your perspective) a new moral framework that generally goes by the name biomedical ethics. This development became necessary for a variety of reasons, most notably (a) technological advances in medicine that enhanced the ability to prolong life and especially to harm, as well as to help, patients; (b) new societal emphasis on individual and civil rights; (c) increasing opportunities for conflicts of interest in medical practice; (d) revelations about medical research conducted without the subjects’ knowledge or adequate consent; and (e) concerns about the lack of equity in the provision of health care services.
The biomedical ethics movement involved a concerted response to these issues by a great number of moral philosophers, theologians, legal theorists, and physicians. In the United States the movement acquired its canonical form as a result of the publications of two bodies, the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1974-78) and the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research (1978-1983). The former developed the ethical framework (i.e., Common Rule) that has since guided all research involving human subjects. The latter delineated and elaborated four basic ethical principles: respect for autonomy, beneficence, nonmaleficence, and justice.
In biomedical ethics the focus is entirely on explicit justification of individual decisions (i.e. who should make them, what principles should be invoked), rather than on the qualities or character of the decision maker. Importantly, the model is one of shared decision making between patient and clinician, with adult patients having the determining voice, unless they lack decision making capacity.
The notable aspect, for my purposes here, is that principles, like respect for autonomy, are intellectual constructs rather than personal traits, like virtues. There is no explicit role for such traits in biomedical ethics. I take it that virtues like compassion, empathy, humility, or courage cannot be actualized without an emotional component. You cannot act compassionately without experiencing some feeling. Thus, while traditional medical morality highlights sensibility of heart, biomedical ethics (at least in theory) exclusively involves intellectual considerations. Principle-based biomedical ethics is often labeled “thin” because, theoretically at least, it leaves out particularistic features of the patient’s community, culture, beliefs, and personal story. Advocates of care, feminist, and/or narrative ethics maintain that such features have great moral relevance to health care decisions. They argue for a “thick” form of health care ethics that takes particularities into account.
“Thickness” in decision making applies to physicians in decisions about the best (or most virtuous) way to allocate their time and effort. Part of this thickness relates to the physician’s feelings, emotions, or “tenderness,” to use Thomas Percival’s term. Consider the following case example.
Case example
The case is an excerpt taken from “Narrative Medicine and Negative Capability,” an essay by the cardiologist Terrence Holt.10 Holt illustrates his discussion of the complexities of moral judgment in medicine by describing a situation he once experienced when he was a resident in the cardiac ICU:
“It is about eleven in the morning and I have been up since six in the morning the day before. The patient has been under my care eleven days. . . . . About fifteen minutes earlier, in response to her request and after several days of discussion, I had asked the nurse to turn off the pump that had been keeping her alive. The family members are around the bedside. The patient is awake . . . She will probably be dead within the hour.
Tears are coursing down my face. I am being very quiet about it, but in a very quiet way I am sobbing as freely as I know how. I’m determined to stay with the patient during this ordeal. But meanwhile I am thinking: This is crazy. I’ve got several unstable patients who need attention. And there’s that arterial line in twenty-four that needs changing . . . At the same time I am utterly sad, haunted by memories of my father’s . . . death ten years ago.
But somewhere a voice is also thinking: I’ll never get to lunch at this rate. I’m so backed up I’ll never get out of here on time.”15
Reflections
I want to reflect on several aspects of Dr. Holt’s judgment in light of the clinical and moral traditions that I have outlined. First, the writer appears to combine deep emotional experience with a sense of detachment. He experiences (a) feelings of sadness and compassion, (b) awareness that at least in part those feelings arise from grief over his father’s death, and (c) detached reflection about his own needs and the work he has to do that afternoon. This combination appears consistent with older admonitions that physicians should maintain “sensibility of heart,” but to be at variance with the contemporary belief that emotional connection with patients is incompatible with good judgment—assuming, of course, that his current choices constitute good judgment. Do they?
Second, from the perspective of contemporary biomedical ethics, Dr. Holt had already fulfilled his ethical duty when he respected the patient’s right to refuse treatment, and consequently withdrew mechanical ventilation. In addition, he may have consciously employed the principle of nonmaleficence if he believed that the respirator was only prolonging the patient’s suffering. He has no moral duty to maintain a compassionate vigil. In contemporary terms, his actions would be considered supererogatory—commendable, but not a moral duty.
Third, but how commendable is his behavior? It is clear that Dr. Holt’s course of action could have arisen, at least in part, from unresolved emotions related to his father’s death ten years earlier. He admits to strong feelings of sadness, loss, and grief, even to the extent of crying. Is this a case of countertransference, a psychological defense mechanism, rather than a true expression of moral virtue? We need to consider the extent to which the emotions about his father’s death are nurturing appropriate compassionate behavior, or, alternatively, contributing to a form of hyper-compassion that is preventing him from attending to other duties.
Fourth, this brings us to the question of harm. Given the level of criticality among his ICU patients, Dr. Holt’s compassionate vigil has a reasonably high risk of negatively impacting the others’ care. He does, after all, have an established duty to provide the best medical care he can to each of his other patients in the ICU. They all have identified and pressing needs. To what extent, if any, does his behavior represent an abrogation of his duty to others? In bioethical terms, he may well be discounting the ethical principles of beneficence and justice in his desire to demonstrate compassion.
To demonstrate this, we can take the narrative a step further. Suppose the man whose arterial line needed to be changed (e.g. nurses have noticed local redness and swelling) develops septic shock shortly after the first patient dies. Dr. Holt has spent more than an hour in the room with the dying patient and his family. Did his delay in removing the infected arterial line precipitate the septic shock? Perhaps it could have been averted had he changed the line earlier that morning? Has his compassion for one patient and his family caused a life-threatening complication in another?
This leads to a fifth consideration. Let’s return to the concept of clinical judgment as being informed by phronesis, a type of wisdom relevant to practical things, requiring an ability to discern the right or virtuous action in a given situation. Thomas Aquinas considered phronesis to be equivalent to prudence, and medical writers like Pellegrino tend to use the terms interchangeably. Pellegrino and Thomasma, in The Virtues of Medical Practice, describe prudence as the virtue that fosters the ability to choose the right way of acting.11 From this perspective, was Dr. Holt’s decision a prudent decision? Would it have been more prudent to excuse himself and go tend to his other duties?
Sixth, let’s look briefly at Dr. Holt’s situation through the lens of narrative ethics, which is a relatively new perspective that highlights medicine’s traditional focus on particular cases or stories as providing the context for individual judgments.12 In this framework, Dr. Holt’s actions make for an engaging story. There is little doubt that his response to what is going on with the patient and his family suggests a more affirmative and inspirational narrative than had he chosen to continue with his ordinary duties. This version is more comforting for the patient and his family, it is more personally fulfilling for the doctor himself, and more compelling for the reader than the more prudent alternative. For better or worse, heroic or passionate behavior is generally far more interesting than prudent behavior. Does that make it right?
Conclusion
Judgment in medical practice is complex and omnipresent, involving decisions that range from diagnosis and treatment of illness to the assessment of relevant patient characteristics and choice of appropriate words. A great deal of this judgment has an important moral dimension. In this paper, I have argued that medical judgment also frequently integrates emotional content into the decision-making process; and the role of emotion can be important and beneficial, rather than damaging. In fact, traditional medical virtues—e.g., compassion, fidelity, courage, and humility—are habits of the heart that are intrinsically associated with emotion, as well as rational cognition.
The case I have presented illustrates this complexity. It also illustrates the role of incomplete knowledge in medical judgment. For example, if we knew more about the benefits and risks of Dr. Holt’s actions, we might come to a more definitive judgment about whether, under the given circumstances, his clinical/moral judgment was right or wrong, correct or incorrect. Surely, respecting the patient’s decision to discontinue the ventilator was morally right, but what about his subsequent decision to spend considerable time with the patient and his family, while postponing other duties? Well, that is a question of judgment.
References
- Feinstein A. Clinical Judgment. Baltimore, Williams & Wilkins, 1967.
- Gregory J. Lectures on the duties and qualifications of a physician. London, W. Strahan and T. Cadell, 1772. [Reprinted in McCullough LB (Ed.) John Gregory’s Writings on Medical Ethics and Philosophy of Medicine. Dordrecht, Kluwer Academic, 1998.]
- Percival, Thomas. Percival’s Medical Ethics. Ed. C. D. Leake. Huntington, NY: Robert E. Krieger, 1975.
- Warner JH, Rizzolo LJ. Anatomical instruction and training for professionalism from the 19th to the 21st centuries. Clinical Anatomy. 2006; 19: 403-414.
- Osler W. “Aequanimitas,” in Hinohara S, Niki H (Eds). Osler’s ‘A Way of Life” & Other Addresses With Commentary & Annotations. Durham, Duke University Press, 2001., pp. 21-29.
- Peabody FW. The care of the patient. JAMA. 1927; 88: 877-882.
- Inui TS. A Flag in the Wind: Educating for Professionalism in Medicine. Washington, DC: Association of American Medical Colleges, 2003.
- Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994; 69: 861-871.
- Coulehan J, Williams PC. Vanquishing virtue: The impact of medical education. Acad Med. 2001; 76: 598-605.
- Coulehan J. Williams PC. Conflicting professional values in medical education. Cambridge Quarterly of Healthcare Ethics, 2003; 12: 7-20.
- Coulehan J. Today’s Professionalism: Engaging the Mind, but Not the Heart. Acad Med. 2005; 80: 892-898.
- Pellegrino ED, Thomasma DC. The Virtues in Medical Practice, Oxford University Press, 1993.
- Cassell EJ. The Nature of Suffering and the Goals of Medicine, 2nd edition, Oxford University Press, 2004.
- Cassell EJ. Doctoring. The Nature of Primary Care Medicine. Oxford University Press, 1997.
- Holt TW. Narrative medicine and negative capability. Lit. Med. 2004; 23(2): 318-333.
- Jones AH. Narrative in medical ethics. Brit Med J. 1999; 318: 253-256.
- Lothe J, Hawthorne J. Narrative Ethics, Value Inquiry Book Series, Rodopi, 2013.
JACK COULEHAN is an Emeritus Professor of Medicine and former Director of the Center for Medical Humanities, Compassionate Care, and Bioethics at Stony Brook University. Jack’s essays, poems, and stories appear frequently in health care journals and literary magazines, and his work is widely anthologized. He is the author of seven collections of poetry, including The Talking Cure: New and Selected Poems (Plain View Press, 2020).

Leave a Reply