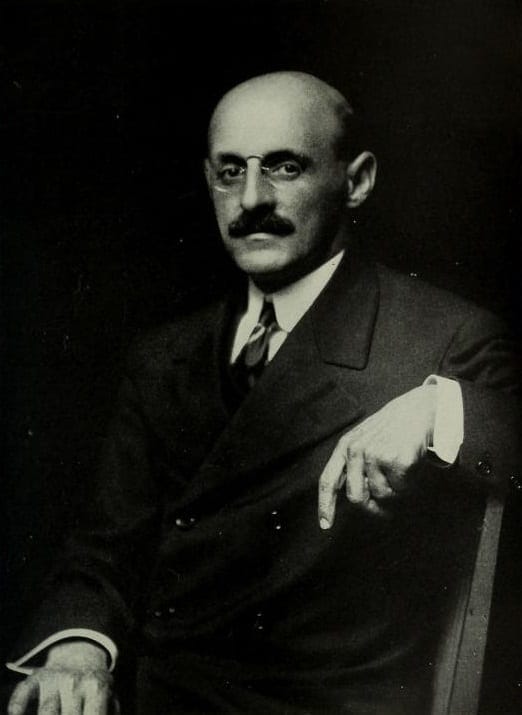
Unlike his brother Simon, who became a celebrated infectious diseases specialist and director of the Rockefeller Institute, Abraham Flexner was mainly interested in culture and education. He also grew up in Louisville, Kentucky, where his father had ended up after an odyssey that had taken him from Bohemia to Strasbourg, to New York, to New Orleans, and then up the river to Louisville. While going to high school, Abraham worked six days a week in a library, checking out books, cataloging them, and educating himself by reading the classics and also by listening to conversations on politics, literature, religion, music, and art. His elder brother Jacob, having become the head of the family after the death of their father, had heard that Johns Hopkins University had a high reputation and gave him $1,000 to go to college there.1
Returning to Louisville, Abraham taught school, but after four years set up a private school, tutoring young people whose parents anxiously wanted them to get into Ivy League colleges. He used unconventional teaching strategies to stimulate and encourage them to study, giving no grades, having no standard curriculum, and teaching in small groups. He lavished personal attention on each student and had many accepted to Harvard, Yale, and Princeton.
Among his students was a girl called Anne Crawford, whom he helped get into Vassar, where she edited the college literary magazine. When she came back to Louisville, she taught in “Mr. Flexner’s School” for two years and published several stories. The two fell in love and became engaged in 1896. They married in 1898, and in 1904 sailed for England and the Continent. Armed with letters of introduction, Abraham attended lectures at Oxford and Cambridge, visited Rugby and Eton, and studied at Berlin and Heidelberg. He was particularly impressed with the German educational system. Back in America, he wrote The American College, a book critical of free electives that allowed students to take only easy courses, too large classes that limited student interaction, and ineffective teaching by unprepared assistants.2
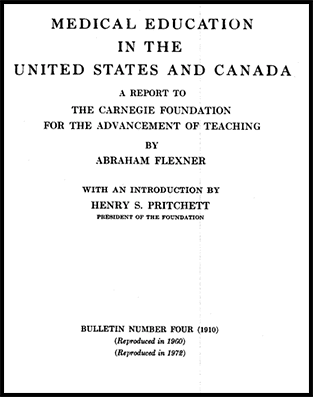
Among those who read his book was Henry Pritchett, president of the newly founded Carnegie Foundation for the Advancement of Teaching. Pritchett was impressed, and after several conversations asked Flexner to make a study of U.S. medical schools, arguing that this should be done by an outsider because medical doctors could not or would not criticize their colleagues.
Flexner and Pritchett went from state to state and visited some 155 medical schools. In a detailed report they concluded that in the previous twenty-five years there had been an enormous overproduction of doctors, five times as many per population as in Germany, but many uneducated and ill-trained. This they attributed to the proliferation of for-profit private schools, all designed mainly to make money. Many of them accepted any applicant who could pay regardless of his education. Often they had no laboratories, no connection with hospitals, no dissecting rooms to teach anatomy, and no libraries. Medical students were little more than apprentices, poorly taught and poorly supervised.
Chicago they regarded as the plague-spot of the nation. There were three university linked medical schools but there were many others, much smaller, their buildings in “wretched condition,” and dirty, with one badly kept room devoted to anatomy and containing a few cadavers “as dry as leather.” Rooms were often inadequate for anything but simple demonstrations, with no teaching accessories worth mentioning, and only very slight provisions for pathology or bacteriology. Some schools provided instructions for three hours at night, allowing students to have full-time jobs. Some of the schools were owned by the deans, often violating state and local board rules.
Flexner regarded Johns Hopkins as the best medical school in the United States, distinguished by its faculty members including William Henry Welch, Howard Atwood Kelly, William Stewart Halsted, and William Osler. Entrance requirements for students were high, the medical faculty well trained, and students thoroughly educated in hospitals. Flexner and Pritchett concluded that about 120 of the 155 extant schools should be closed or consolidated to a few. In their investigations they had to deal with subterfuge, threats of lawsuits, and threatening letters. But when their report was published the consequences were profound. Many medical schools collapsed, some pooled their resources and were consolidated, admission criteria and curricula were reorganized, and standards of clinical instruction in the hospital were emphasized, as well education in science using properly equipped laboratories.
The Flexner Report3,4 created a revolution and remade medical education in the United States. It exposed medical quackery, and made scientific and supervised clinical training central in the education of physicians. It helped make medical doctors esteemed, valued, and well-paid professionals. Medical research became a priority in universities, especially after the Second World War, when the government lavished huge amounts of money on universities and their ever-growing staff.
But the great advances in medicine made by adopting the German educational system were not made without cost. Already at the time of the original report, concerns were expressed about its overall unsparing critical tone and its overemphasis on education and science rather than on medical practice by an academician with no medical training and no understanding of its practice and the needs of providing medical care. Quite early on people like Willian Osler and Harvey Cushing worried about the deleterious effects of the university full-time system, which in the opinion of Osler would result in a generation of clinical prigs.5 William Castle argued that the Flexner Report decreased the supply of doctors and drove up medical costs. More recent critics have commented on a perceived decline in medical caring and an erosion of the doctor-patient relationship.6 This trend has clearly been exacerbated by the large quantities of money available both in universities and in private practice, the growth of medical corporations, and the adoption of a market-place philosophy, compounded by the increasing cost of providing medical care. In recent decades, there have been significant attempts to reverse this trend and put more emphasis on the service component of medical care and on the reaffirmation of the doctor-patient relationship.6
In fact, however, the situation is even more complex. Since 1910 the population of the United States has tripled, jobs in farms and agriculture are fewer, and women have entered the workforce in large numbers. Many jobs now come from healthcare, nursing, clerical and assistant duties, administration, regulation, bureaucracy, legal medicine, social work, education, journalism, and ever more complex and expensive technology. The public has become more educated and more demanding. The authority of the doctor has diminished, and so has confidence in the medical profession. At one time a doctor might have listened to a patient’s chest with a stethoscope and reassured him that he could save him money by not ordering a chest x-ray. Now many patients might question him and the doctor, fearful of being sued, would order an MRI.
References
- Seyal, MS. Abraham Flexner: his life and legacy. Hektoen International. Summer 2013.
- Abraham Flexner: An Autobiography, Simon & Schuster, 1960.
- Flexner A. Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching. Boston, Mass, 1910.
- Ludmerer, K. Understanding the Flexner Report. Academic Medicine 2010;85:193 (issue2, February).
- Osler, Sir William. On full-time clinical teaching medical schools. Canad Medl Ass J 1962; 87:762.
- Duffy TP: The Flexner report – 100 years later. Yale J Biol Medicine 2011; 84:269 (Sept).