Benjamin Chin-Yee
Toronto, Ontario, Canada
In the spring of 1953 at the Verdun Protestant Hospital in Montreal, the psychiatrist Heinz Lehmann initiated the first trial of chlorpromazine in North America, treating “psychomotor excitement” in patients with diagnoses ranging from manic depression to schizophrenia.1,2 Within weeks, the drug proved a remarkable success: patients’ delusions, hallucinations and thought disorders disappeared.3,4 For one patient with mania, the drug alleviated the feeling that she “had to live [her] whole life in one day”; another patient with long-standing anxiety reported, “[i]t was like a chairman taking control of a meeting where everybody previously had been shouting at once.”5The drug’s effects were striking and unprecedented; as Lehmann later recalled, “nobody knew why it would work and we hardly believed it the first time. I saw the first patients better after two or three weeks and I thought, it must be a fluke.”6
Historians have called the discovery of chlorpromazine, “the critical event in the foundation of psychopharmacology,”7 which “initiated a revolution in psychiatry, comparable to the introduction of penicillin in general medicine.”8 Chlorpromazine quickly spread to asylums throughout North America where it dramatically changed inpatient management and made it possible for many chronically ill patients to return to their homes in the community. The early success of chlorpromazine gave the hope that, one day, medications may offer a cure for severe mental illness. In 1955, the Canadian news magazine Maclean’s declared that chlorpromazine was “leading a revolution that’s taking the word ‘hopeless’ from more forms of mental illness.”9 Other psychoactive drugs, such as opium and barbiturates, had previously been used in psychiatry, and new twentieth-century treatments—notably electroconvulsive therapy and insulin coma therapy—offered some source of therapeutic optimism; however, it is difficult to overstate the impact of chlorpromazine, which for the first time provided effective relief of symptoms of psychosis with relatively minimal side effects.10,11
In addition to its direct clinical impact, the introduction of chlorpromazine also contributed to broader changes in psychiatry and medicine. Antipsychotic drugs were an important factor in the de-institutionalization movement, which resulted in the decline of the asylum and an increasing focus on outpatient psychiatric care. The Verdun Hospital, which housed nearly 1,500 inpatients in 1942, was reduced to 908 beds by 1981, a trend reflected at mental hospitals throughout North America.12
Chlorpromazine directly impacted new biological theories of mental illness, which sought to ground psychiatry in the neurosciences and explain psychiatric symptoms as the result of chemical imbalances in the brain. When Lehmann and other clinicians initially administered chlorpromazine, little was known of its mechanism of action. Different theories had been proposed, which included psychoanalytic explanations of the drug’s effects through its ability to decrease “psychic energy” upholding “ego defenses.”13 A decade later, however, chlorpromazine’s effectiveness in treating psychosis became understood in terms of neurotransmitter systems, in particular the dopaminergic theory of psychosis. This neurotransmitter model would establish a biological paradigm in psychiatry that forms the basis of our current medical understanding of mental illness and pharmacotherapy.
The history of psychiatry is often represented as a swinging pendulum, oscillating between biological and psychological theories of mental illness, with therapies targeted at the soma or the psyche.14 Despite this metaphor’s crude and simplistic dichotomy, there is indeed a tension apparent in psychiatry today.15 In this age—the “age of psychopharmacology”—there nonetheless remains a strong demand for psychotherapy and, in general, a desire for a more humanistically-oriented practice.16 The introduction of chlorpromazine into the asylum was a definitive moment in psychiatry’s swing towards the biological paradigm. The rise of biological psychiatry—equipped with new and powerful drugs—would underwrite the decline of psychoanalysis, which was already underway by the 1950s. Further developments in psychopharmacology would widen the chasm between humanistic and pharmacologic approaches, leading to the problematic “split” that exists in psychiatry today.17
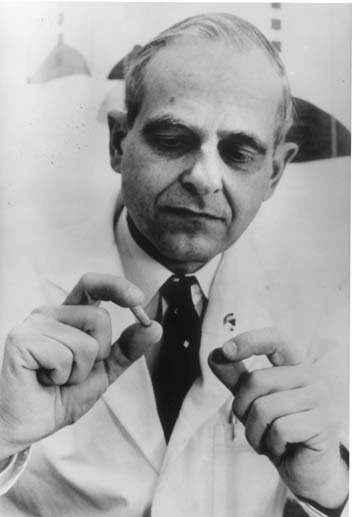
Of course, Lehmann could not have predicted how his actions would influence the history of psychiatry when he first administered chlorpromazine at the Verdun Hospital in 1953. Lehmann, a German refugee who fled to Canada in 1937, was not concerned with advancing a certain research program or promoting a particular theory of psychiatric disease. He was not a researcher or a neuroscientist, but rather a consummate clinician first and foremost. As Lehmann later reflected, “I never had postgraduate training—it was during the war and there was no way of getting away because they didn’t have enough staff to let me go anywhere.”18 Nonetheless, he recalled, “I got the best training just by the fact that from 8.30 in the morning, until midnight I was making my rounds and seeing hundreds of patients for many, many hours every day over many years.” From this clinical experience, he learned “the kind of idiosyncratic, individualized flexibility, […] empathy, and the expertise you get through the experience of being able to relate to individuals rather than to a statistical number of biological facts.”
Lehmann’s trial of chlorpromazine was guided by his attention to patient care and hope of treating the debilitating psychiatric symptoms that he encountered on a daily basis in his capacity as asylum physician. He came across research reports on chlorpromazine left for him by a passing salesman from Rhône-Poulenc, the French manufacturer of the drug. Aided by his ability to read French—Lehmann’s wife was French Canadian, and they spoke French at home—he examined the article reprints in his bathtub one Sunday evening and was intrigued by the findings. These were the reports by Parisian psychiatrists Jean Delay and Pierre Deniker who described the sedative effects of chlorpromazine as producing a sort-of “chemical lobotomy.”19 Although slightly skeptical of these claims, Lehmann decided to test the drug and enlisted the help of his resident Gorman Hanrahan to administer chlorpromazine to a total of seventy-one inpatients at the Verdun Hospital. They carefully monitored the drug’s effects, reporting their results in an article that would shape the history of the field and introduce chlorpromazine to the mental hospitals of North America.
Lehmann seems an unlikely hero in the narrative of biological psychiatry, and it is ironic that he became known as a main protagonist in the development of psychopharmacology. In fact, Lehmann’s decision to pursue a career in psychiatry stemmed from his fascination with Freud during his adolescence, whose ideas he found helpful in resolving his own emotional struggles, which he later identified as an episode of depression.20 Despite becoming a pioneering figure in psychopharmacology, he maintained the importance of humanistic approaches in psychiatry throughout his career. Lehmann’s role in the story of psychopharmacology is best understood as a genuine effort to alleviate symptoms of severe mental illness at a time when few therapeutic alternatives existed. He was encouraged by a therapeutic optimism that he shared with his patients and their families—families that hoped to one day receive their loved ones back home from hospital.
Upon reflection, Lehmann was somewhat ambivalent about his role in this history: “I have often wondered whether it was a good thing that I was instrumental in getting the drugs into psychiatry.”21 He expressed his dismay that psychopharmacology spawned what he called “cook book” psychiatry, which loses the important therapeutic relationship between physician and patient in its focus on diagnosing and prescribing. He acknowledged the major advances in the neurosciences that occurred in his lifetime; however, he cautioned, “the fact that we can explain more is not understanding,” and believed that “the understanding part is the personal part, the interpersonal part.” Lehmann advocated transcending the biological/psychological divide that had emerged in psychiatry, and emphasized the need to integrate these approaches to help patients suffering with mental illnesses.
Despite the far-reaching impact of chlorpromazine—its role in emptying asylums, spurring drug discovery, and bolstering a biological paradigm of mental illness—this moment in history, and the part played by Heinz Lehmann, reveals that the important driving force behind this movement was, above all, a concern for the wellbeing of patients. For Lehmann, the healing role of the physician was always primary, and therapeutic innovation should always be motivated by the goal of improving patient care, an ethic too often forgotten in an age when competing interests increasingly influence drug development and marketing. As Lehmann reminds us, “a psychiatrist ought to be somebody who can use whatever is available to help his patients,” a fact that remains true amidst shifting theoretical frameworks and therapeutic approaches in psychiatry and medicine.22
Notes
- The Verdun Protestant Hospital was renamed the Douglas Hospital in 1965.
- H. E. Lehmann and G. E. Hanrahan, “Chlorpromazine: New Inhibiting Agent for Psychomotor Excitement and Manic States,” Archives of Neurology and Psychiatry 71 (1954): 227.
- H. Lehmann, interview by D. Healy, “Heinz Lehmann: Psychopharmacotherapy,” in The Psychopharmacologists, ed. D. Healy (London: Chapman & Hall, 1996), 160.
- H. Lehmann, “The Introduction of Chlorpromazine to North America,” Psychiatric Journal of the University of Ottawa 14, no. 1 (1989): 263-265.
- Lehmann, “Chlorpromazine,” 231.
- Untangling the Mind: The Legacy of Dr. Heinz Lehmann, produced by C. Mullins, (New York, NY: Filmakers Library, 2000), DVD.
- D. Healy, The Antidepressant Era (Cambridge: Harvard University Press, 2002), 43.
- E. Shorter, A History of Psychiatry: From the Era of the Asylum to the Age of Prozac (New York: John Wiley & Sons, 1997), 255.
- S. Katz, “The New Wonder Drugs that Fight Insanity,” Maclean’s Magazine, November 12, 1955, 11.
- For a discussion of the continuities and discontinuities between earlier and later treatments in psychiatry, see D. Healy, “Some continuities and discontinuities in the pharmacotherapy of nervous conditions before and after chlorpromazine and imipramine,” History of Psychiatry 11 (2000): 393-412.
- Lehmann’s initial 1953 trial examined closely for potential side effects of chlorpromazine. They noted some side effects, including the now-familiar extrapyramidal symptoms; however, they concluded that these side effects were minimal compared to the other available treatments, namely electroconvulsive therapy and insulin coma therapy. See Lehmann, “Chlorpromazine,” 233-236.
- C.H. Cahn, Hôpital Douglas: 100 ans d’histoire et de progrès / Douglas Hospital: 100 years of history and progress (Montreal: J. Emile Roys & Fils, 1981), 55, 191. Today, the Douglas Hospital has 241 beds, Institut universitaire en santé mentale, “Rapport annuel 2013-2014,” 2014, 42. (http://www.douglas.qc.ca/publications/251/file_fr/rapport_annuel_2013-2014_final.pdf).
- M. A. Ramos, “Drugs in context: a historical perspective on theories of psychopharmaceutical efficacy,” The Journal of Nervous and Mental Disease 201, no. 11 (2013): 926-933.
- Despite this metaphor’s extensive use by historians, some highlight inaccuracies and limitations arising from the application of this metaphor in the history of psychiatry. See J. Sadowsky, “Beyond the Metaphor of the Pendulum: Electroconvulsive Therapy, Psychoanalysis, and the Styles of American Psychiatry,” Journal of the History of Medicine and Allied Sciences 61, no. 1 (2005): 1-25.
- For an anthropological study of the tension between psychopharmacology and psychotherapy, and the problems arising from this “split” in modern psychiatry, see T.M. Luhrmann, Of Two Minds: The Growing Disorder in American Psychiatry (New York: Alfred A. Knopf, 2000).
- G. Schomerus, C. Schwahn, A. Holzinger, P. W. Corrigan, H. J. Grabe, M. G. Carta, and M. C. Angermeyer, “Evolution of public attitudes about mental illness: a systematic review and meta-analysis” Acta Psychiatrica Scandinavica 125 (2012): 440-452.
- Luhrmann, Of Two Minds, 203.
- This series of quotes is from an interview with Lehmann in 1996. Lehmann, interview by D. Healy, “Heinz Lehmann: Psychopharmacotherapy,” 171.
- Ibid., 159.
- Untangling the Mind: The Legacy of Dr. Heinz Lehmann, produced by C. Mullins.
- Lehmann, interview by D. Healy, “Heinz Lehmann: Psychopharmacotherapy,” 171.
- Ibid.
Bibliography
Cahn, C.H. Hôpital Douglas: 100 ans d’histoire et de progrès / Douglas Hospital: 100 years of history and progress. Montreal: J. Emile Roys & Fils, 1981.
Healy, D. The Antidepressant Era. Cambridge: Harvard University Press, 2002.
Institut universitaire en santé mentale. “Rapport annuel 2013-2014.” 2014. (http://www.douglas.qc.ca/publications/251/file_fr/rapport_annuel_2013-2014_final.pdf).
Katz, S. “The New Wonder Drugs that Fight Insanity.” Maclean’s Magazine, November 12, 1955.
Lehmann, H. E. and G. E. Hanrahan. “Chlorpromazine: New Inhibiting Agent for Psychomotor Excitement and Manic States.” Archives of Neurology and Psychiatry 71 (1954): 227-237.
Lehmann, H. Interview by D. Healy. “Heinz Lehmann: Psychopharmacotherapy.” In The Psychopharmacologists, edited by D. Healy, 159-186. London: Chapman & Hall.
Lehmann, H. “The Introduction of Chlorpromazine to North America.” Psychiatric Journal of the University of Ottawa 14, no. 1 (1989): 263-5.
Luhrmann, T. M. Of Two Minds: The Growing Disorder in American Psychiatry. New York: Alfred A. Knopf, 2000.
Ramos, M. A.“Drugs in context: a historical perspective on theories of psychopharmaceutical efficacy.” The Journal of Nervous and Mental Disease 201, no. 11 (2013): 926-933.
Sadowsky, J. “Beyond the Metaphor of the Pendulum: Electroconvulsive Therapy, Psychoanalysis, and the Styles of American Psychiatry,” Journal of the History of Medicine and Allied Sciences 61, no. 1 (2005): 1-25.
Schomerus, G, C. Schwahn, A. Holzinger, P. W. Corrigan, H. J. Grabe, M. G. Carta, and
M. C. Angermeyer. “Evolution of public attitudes about mental illness: a systematic review and meta-analysis.” Acta Psychiatrica Scandinavica 125 (2012): 440-452.
Shorter, E. A History of Psychiatry: From the Era of the Asylum to the Age of Prozac. New York: John Wiley & Sons, 1997.
Untangling the Mind: The Legacy of Dr. Heinz Lehmann. Produced by C. Mullins. New York, NY: Filmakers Library, 2000. DVD.
, BSc, MA, MD (2017) is a medical student at the University of Toronto. He received his BSc in Biology from McGill University and studied History and Philosophy of Science as a visiting student at the University of Cambridge. He recently received his MA from the Institute for the History and Philosophy of Science and Technology at the University of Toronto. His research interests include the history of clinical medicine and the patient-physician relationship. He hopes to pursue a career in medicine that combines clinical practice with academic research in the medical humanities.
Highlighted in Frontispiece Summer 2016 – Volume 8, Special Issue, and Winter 2016 – Volume 8, Issue 1

Leave a Reply