Julius Bonello
Michael Neff
Zoe Demko
Peoria, Illinois, United States
One of the greatest medical achievements of the twenty-first century was the creation of penicillin. The road to this great achievement began almost 300 years ago when Antonie van Leeuwenhoek (1632–1723), a draper by trade who had no science background, wished to assess the quality of his threads.
Around 1676, van Leeuwenhoek started to create lenses stronger than his magnifying glass. As he ground and polished them more and more, he began to see objects smaller than the fibers he had intended to study. He then began to look at other things such as well water, rainwater, and his own saliva. When he studied the tartar from his own teeth (and samples from his wife and child), he observed tiny moving objects: “there were many very little living animalcules, [from Latin animalculum = “tiny animal”] very prettily a-moving.” He continued, “Moreover, the animalcules were in such enormous numbers, that all the water . . . seemed to be alive.” Today, we call these tiny animals bacteria.
In 1998, scientists at the University of Georgia estimated that there are five nonillion bacteria on earth. That is five with thirty zeros behind it. Compare that with eight billion people living today: eight with nine zeros. We are vastly outnumbered.
Fortunately, most of these are commensal bacteria. They live and work in harmony with us, but there are others that wreak havoc in our lives: the pathogenic bacteria. From pimples to pus, from plague to an infected tooth to flesh-eating infections, all of these are caused by pathogens.
Since the first physician hung his shingle, doctors have searched for means to prevent infection by these pathogens. Early Egyptians used honey and willow branches. Greeks and Romans poured vinegar or wine on wounds. Joseph Lister, in 1856, soaked bandages with carbolic acid (phenol) on a fresh open fracture to prevent infection of the bone. In the early 1900s, surgeons began washing their hands and instruments with phenol before an operation. Alas, despite these interventions, if the wound became infected, physicians were powerless until 1942, when my adopted city, Peoria, Illinois, pitched in to produce penicillin.
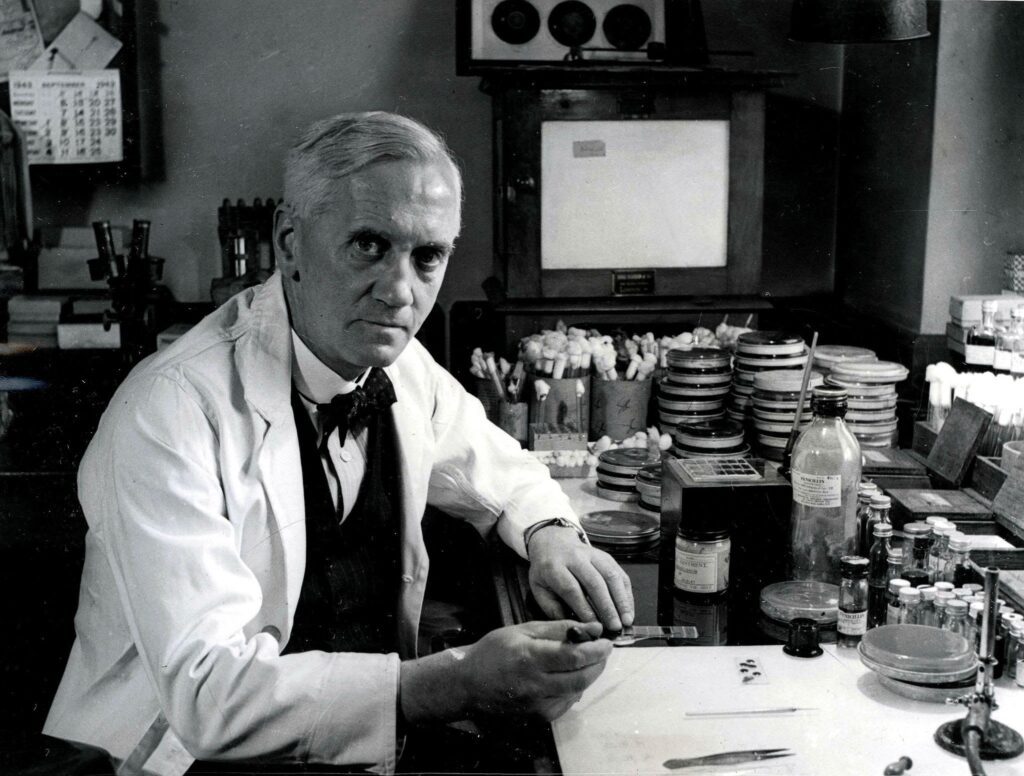
In 1928, Alexander Fleming, a Scottish physician working in London, discovered by accident a mold with bacteria-killing powers. Having spent time with convalescing soldiers during World War I, he was familiar with the pathogenic bacteria Staphylococcus and Streptococcus, which caused most wound infections. After an extended vacation, he returned to his lab and while cleaning out his old petri dishes filled with these pathogens, noticed a mold growing on one of the dishes. Looking more closely, he was surprised to see that the mold was surrounded by an area of dead bacteria. He surmised that either the mold had killed the bacteria or prevented it from growing. He consulted another scientist in the lab and found that the mold was Penicillium. Over the next year, he worked with the mold and published his findings in a paper in 1929. He even presented his findings at a scientific meeting but was largely ignored because of the similarities to already used antiseptics. Years later, it was concluded that if Fleming had performed animal studies, he would have seen his “mold juice” as a great discovery.
Ten years later, two researchers at Oxford University were looking to discover new antibacterials. Howard Florey, an Australian physiologist and Ernst Chain, a German chemist, began their work in 1935. Needing a competent microbiologist, Florey added Dr. Norman Heatley to the team. Scouring the literature, Chain discovered Fleming’s 1929 paper on penicillin. Having a mold sample already in the lab from Fleming, they started experimenting immediately. After four years of chemical analysis and isolating a purer form, they began to perform animal studies. In 1940, they injected eight mice with a pathogen. Four mice were given penicillin and four were used as controls. After six hours, the control mice were showing signs of sickness. Heatley was so impressed that he slept that night in the lab and checked on the mice at 3:45 am. All the control mice were dead, and the treated ones were alive. They immediately started human studies and found that penicillin was therapeutic. They published their results in the Lancet on August 24, 1940. Within two weeks of the publication, a team of US scientists asked the Oxford team for cultures of Penicillium. After receiving them, the first doses of penicillin were given in New York City on October 15, 1940.
It was clear to the team at Oxford that large volumes of fermentation liquor would be needed if sufficient quantities of the drug were to be available for clinical use. Penicillium only survives on the surface of this liquid and their lab had no containers larger than a half-gallon flask. Searching for larger containers, they settled on hospital bed pans, which could hold larger quantities of liquid. However, this was still not enough surface area. Adding to this predicament was that England was now involved in World War II. Money was scarce and companies did not have the resources to provide the Oxford team with ways of mass producing the mold. Because the United States was not involved in the war at that time, the Oxford team decided to bring the cultures to the United States in hopes that US pharmaceutical companies would see the need for this drug. To make sure that the cultures arrived in the United States and were not intercepted by German spies, the Oxford team (Florey and Heatley) had the spores spread in their coat pockets during their flight to the United States.
They arrived in New York City and were directed to the office of Dr. Charles Thom, a mycologist in Washington DC. Thom was one of the world’s foremost experts on molds and fungi. Florey detailed the difficulties encountered in their effort to produce large quantities of penicillin, and Thom directed them to the US Agricultural Department. There, the Oxford team was directed to Peoria, Illinois, where the Northern Regional Research Laboratory was located. The Peoria staff was telegraphed that day and told to arrange shallow pan set-ups for production. The Oxford team arrived July 14, 1941, and met Dr. Robert Coghill, the head of the fermentation division. He was not familiar with the work done at Oxford, but by the end of the afternoon, Coghill promised full cooperation.
The Peoria scientists would use corn steep liquor, a viscous byproduct of cornstarch, in large 300-gallon tanks. It is rich in nitrogen, which promotes excellent growth. These tanks would be agitated and air blown in from the bottom so that the mold could be produced submerged in the liquor and not only on the surface. After one month of experimenting with different additives, the production of penicillin was progressing. Wanting to increase the potency of the drug, the Peoria team asked for other strains of the mold. Samples were sent in from all over the world, but the strongest strain actually came from in town. A woman, searching behind a Peoria grocery store, found a rotting cantaloupe with what turned out to be the strongest strain.
With the United States entering World War II, the production of penicillin became a priority. In 1942, Merck, Squibb, and Pfizer signed an agreement to share research and production information. By the end of 1943, the production of penicillin was the second highest priority at the war department. Only the Manhattan Project (development of the atom bomb) was considered more important. Together with the Peoria team, by using X-rays and adding additives to the medium that grew the penicillin, the US pharmaceutical companies were able to change the drug to make it more effective. By June 1943, 400 million units of penicillin had been produced in America. By January 1944, 20.5 billion units were manufactured and by D-Day, production was approximately 100 billion units per month, enough to care for 40,000 patients. By 1951, 30 trillion units of penicillin were produced each month in the United States.
Today penicillin is produced throughout the world in 50,000-gallon tanks. Each tank contains more than a trillion units of penicillin.
Epilogue
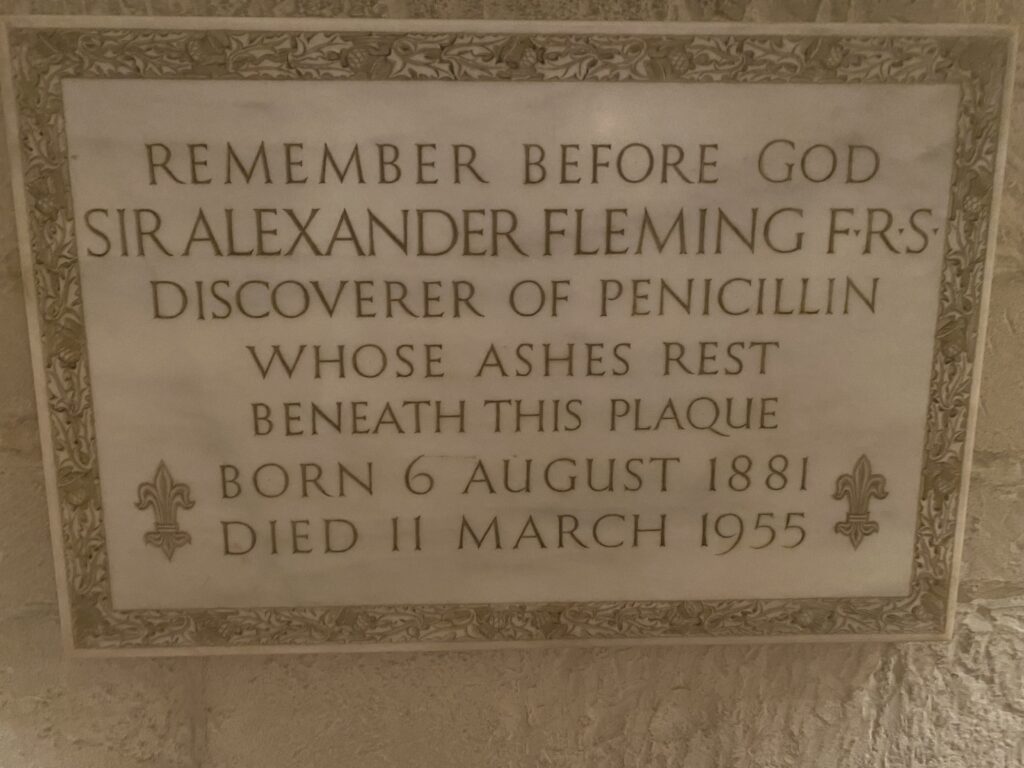
In 1945, Fleming, Chain, and Florey were awarded the Nobel Prize in Medicine. Dr. R. Coghill was awarded the Presidential Medal of Merit for his work on penicillin. He died in 1997 at the age of ninety-three. On March 11, 1955, Fleming died in London at the age of seventy-three. He was cremated and his ashes were interred in a crypt of Saint Paul’s Cathedral in London. Chain died in Ireland during a summer holiday in 1979 at the age of seventy-three. Florey was made president of Queens College in 1963. He died on February 21, 1968 of a heart attack at the age of sixty-nine. In 1982, a commemorative plaque was placed in his honor in the floor of Westminster Abbey near the one for Charles Darwin. Historians today regard Fleming’s 1929 largely ignored article as one of the most important medical papers ever written.
References
- Hobby, Gladys L. Penicillin, Meeting the Challenge. Yale University Press, 1985.
- Lax, Eric. The Mold in Dr. Florey’s Coat. Henry Holt & Company, 2005.
JULIUS P. BONELLO, MD, is a Professor Emeritus of Clinical Surgery at the University of Illinois College of Medicine Peoria. Dr. Bonello has given 43 years of service to UICOMP, continuing to take an active role in medical students’ educations there. Although clinically retired since 2018, he continues his passion of writing and publishing articles on the history of medicine.
MICHAEL J. NEFF and ZOE O. DEMKO are medical students at the University of Illinois College of Medicine Peoria.

Leave a Reply