Jayant Radhakrishnan
Chicago, Illinois, United States
Almost 5,000 years ago, the Chinese described a disease that presented with intermittent fevers, enlarged spleens, and a predilection to epidemics. Those malarial infections were possibly caused by Plasmodium vivax (P. vivax) since P. malariae is unlikely to cause epidemics. The Chinese did not mention mortality following these symptoms; therefore, P. falciparum was probably still confined to Africa.1 Hippocrates (460–377 BC) described benign tertian (P. vivax), quartan (P. malariae), and malignant subtertian (P. falciparum) forms of the disease in Greece.
In the early days, malaria was believed to be the work of demons, deities, and the devil.2 Malaria has afflicted important people and altered history around the world. Some believe that Alexander the Great may have succumbed to it since he suffered from an eleven-day illness with high fevers. If that is the case, P. falciparum had emerged from Africa by 323 BC. Abraham Lincoln had malaria in 1830 when he relocated to Illinois and again in 1835 while living in New Salem, Illinois.3 The story of how the natives of South America knew the curative properties of the bark of the cinchona tree are well known. Thus, malaria has long been present around the world and is believed to have played a role in the fates of many empires and countries, including the independence of the United States.4 It is also hypothesized that it played a role in Pemberton’s surrender to Grant at Vicksburg during the American Civil War.5
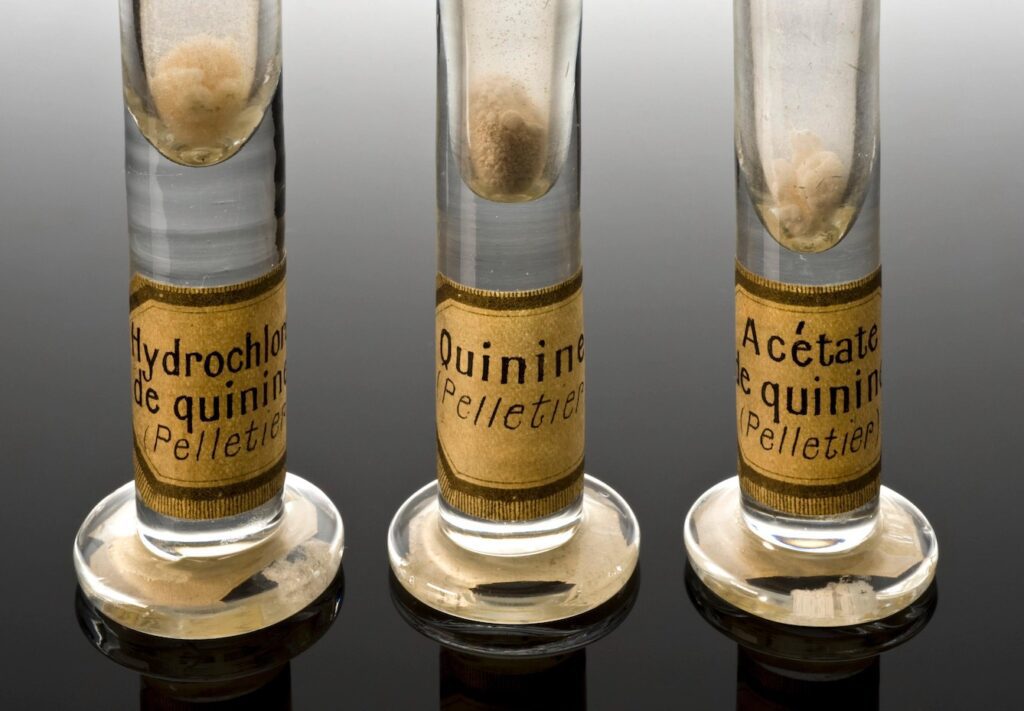
Currently, malaria is only active in the tropics and subtropics because it has been controlled in other parts of the world. If conditions become suitable, say with warming of temperate regions, it will surge immediately in other parts of the world. Madagascar is an example. Malaria had been eradicated there but it caused havoc when conditions were conducive to its resurgence in 1986.1 Malaria affects society by rendering people unable to work and decimating the economies of these parts. Hence, once quinine was extracted from the bark of the cinchona tree in 1820, British colonial officers posted in India were asked to mix the powder in water and to drink it to guard against malaria. However, the therapeutic concentration was too bitter to swallow. Some enterprising officer decided to dissolve the powder in gin and add sugar and lime, and the gin and tonic cocktail was born.6
By the nineteenth century, Hippocrates’ miasma (Greek: “stain” or “pollution”) hypothesis7 to explain the disease mal aria (“bad air” in medieval Italian) was no longer believed, and in 1880 Charles Louis Alphonse Laveran identified the malaria parasite within erythrocytes. He also observed that use of quinine removed it from the cells.8 The ancient Greeks had named one type of mosquito “anopheles,” which means “useless,” as they believed it did not bite and was not a threat to humans.9 In August 1897, Ronald Ross demonstrated the malaria parasite in the stomach tissues of a female anopheles mosquito and charted the entire life cycle of the malaria parasite.10 Therefore, by the end of the nineteenth century, the parasite, vector, and treatment for malaria were all known, yet malaria continued to ravage populations. Younger children and pregnant women were particularly vulnerable.
There are many reasons why humans continue to be so vulnerable to malaria. People develop partial immunity to malaria but only after repeated exposures.11 Children under five years of age do not have enough exposures to be immune. Also, for immunity to last more than six months, repeated and continuing exposures are required. If malaria is eliminated from an area and then recurs after six months to a year, the population is no longer immune, as was the case in Madagascar in 1986.1 Protective human genetic polymorphisms in the population at risk take centuries to develop, and while they increase resistance to malaria, they cause problems of their own. The following changes fall into this category: sickle cell disease, hemoglobin C, hemoglobin E, ovalocytosis, eliptocytosis, loss of the Gerbich antigen (glycophorin C), RBD Duffy negativity, thalassemias, and glucose-6-phosphate dehydrogenase (G6PD) deficiencies.1
From the mid-nineteenth century onwards, malaria declined spontaneously in Europe because contact between mosquitos and humans was reduced as living conditions improved. Furthermore, once the role of the female anopheles mosquito was established, attempts at vector control were instituted. By the 1950s, malaria had been largely eliminated in North America and most of Europe, but it was still running rampant in Asia and Africa. In 1954, the World Health Organization (WHO) instituted a massive and extremely expensive malaria eradication campaign that attacked the problem from various angles. The first was vector control. Standing water was drained whenever possible and sanitation was improved. When that could not be done, oils were sprayed on the pooled water to suffocate larvae. In addition, indoor residual spraying (IRS) with an approved insecticide was employed to kill mosquitos taking their usual postprandial nap on the walls of homes. Attempts were also made to introduce sterile male mosquitos in affected areas and to use gain-of-function techniques to suppress P. falciparum in the anopheles mosquito.12
Simultaneous attempts at avoiding human contact with mosquitos consisted of building better houses, using light colored clothing to cover most of the skin, particularly after sunset, and the use of insecticide-treated nets (ITN) for sleeping. ITNs treated with pyrethroids derived from the chrysanthemum flower reduce infections to almost half of that seen with untreated nets and offer 70% better protection than if nets are not used at all.13 Pyrethrum attacks the nervous system of mosquitos and renders them unable to move. Cleopatra (69–30 BC) used mosquito nets. Whether it was only to avoid pesky mosquito bites and to get a good night’s sleep, or whether ancient Egyptians had identified the role of the mosquito in spreading malaria is not known. From 400 BC, the Persians knew that chrysanthemum was an insecticide, but it is not known whether anyone used it against mosquitos.
The third step was using prophylactic chemotherapies. Travelers to malaria-prone areas were advised to take a drug appropriate for the area for two to three weeks before travel and for four weeks afterwards to cover any parasites that emerged later from the liver. People living in endemic areas were advised to self-medicate in seasons when the risk of malaria was the highest, regardless of whether they were infected or not. Finally, patients with malaria were treated with highly effective medicines. Over the years, resistance to many drugs and insecticides has resulted in the need for more expensive chemotherapies. The current standard is artemisinin-based combination therapy (ACT). Quinghaosu, now known as artemisinin, was first mentioned in Ge Hong’s (283–343 AD) Zhou hou bei ji fang (A Handbook of Prescriptions for Emergencies). It was extracted from the dried leaves of artemisia annua (sweet wormwood) by Tu Youyou in 1971.14
Despite these all-out efforts, malaria has not been eradicated. In 2021, according to the WHO, nearly half the world’s population was at risk for malaria, resulting in 247 million cases and 619,000 deaths.15 Much greater progress would have been made if an effective vaccine were available. The sporozoite that is injected into the bloodstream by the female anopheles mosquito immediately enters hepatocytes, where it multiplies profusely and forms merozoites. When the hepatocyte ruptures, the merozoites escape, enveloped in the host cell’s membrane that protects it from the human host’s immune system.16 Merozoites immediately make their way into erythrocytes where they replicate profusely. Depending on the nature of the parasite. the overfilled erythrocytes disintegrate every three or four days, giving rise to the typical intermittent fevers while also infecting more erythrocytes. The parasite is safe from the host’s immune system while replicating in the liver and in the erythrocytes; therefore, to prevent the disease, any vaccine must attack the parasite in the pre-erythrocyte stage. Of course, the ideal vaccine would attack the parasite in all its stages.
SPf66 is a multistage vaccine. It had an extensive randomized trial in endemic areas. Unfortunately, it did not protect against P. falciparum in Africa, and it protected only modestly in South America.17 Subsequently, pre-erythrocytic vaccines were studied. In this group, the RTS,S/AS01 vaccine was the best of all. RTS,S/A01 is a circumsporozoite protein (CSP)-based vaccine. CSP is secreted in the sporozoite phase of the parasite and has a critical role in invasion of hepatocytes by the plasmodium. RTS,S/A01 reduced clinical episodes of malaria by 26% and severe malaria by 58% for eighteen months. Parasitemia was reduced by 26% for six months after immunization.18 This modest protection is not good enough to make a major dent in the incidence of malaria. The latest vaccine developed is named the R21/Matrix-MTM. It is also a CSP-based vaccine. Phase I trials were completed in Kenya and Phase II in Burkina Faso. Phase III results published ahead of peer review are impressive. They demonstrate a vaccine efficiency (VE) of 75% where malaria is seasonal and of 68% where it is endemic. Furthermore, five to seventeen-month-old children had higher titers than eighteen to thirty-six-month-old youngsters. Finally, the younger age group showed the highest twelve-month VE to clinical malaria episodes in both situations, being 79% in the seasonal and 75% in the endemic areas.19
On October 2, 2023, the WHO gave the go ahead for its clinical use. If R21 lives up to its promise, the world could finally be rid of this scourge after more than 5,000 years of recorded history. If so, Oxford University researchers who developed this vaccine would be contenders for the Nobel Prize.20 They would be following Ronald Ross (1902),10 Alphonse Laveran (1907),8 and Tu Youyou (2015),14 all of whom received the Nobel Prize for their contributions to understanding and managing the disease. Paul Hermann Muller (1948)21 helped indirectly by discovering that dichlorodiphenyltrichloroethane (DDT) is a contact poison against mosquitos, and Julius Wagner-Jauregg (1927)22 recognized that using malariotherapy treated dementia paralytica. The Poonawallas of the Serum Institute of India (SSI) also deserve a vote of thanks for funding the study at personal financial risk and then supplying an affordable vaccine at a time when vaccines are a major source of profit for the pharmaceutical industry.
Bibliography
- Carter R, Mendis KN (2002). Evolutionary and historical aspects of the burden of malaria. Clin Microbiol Reviews 15(4):564-594. doi: 10.1128/CMR.15.4.564–594.2002.
- Neghina R, Neghina AM, Marincu I, Iacobiciu I (2010). Malaria, a journey in time: In search of the lost myths and forgotten stories. Am J Med Sci 340(6):492-498. doi: 10.1097/MAJ.0b013e3181e7fe6c.
- Sotos JG. (2008). The Physical Lincoln Sourcebook. Mt. Vernon Book Systems. ISBN 978-0-9818193-3-4 Pp. 385-386.
- McNeill JR (2016). How the lowly mosquito helped America win independence. The Smithsonian Magazine June 15, 2016. https://www.smithsonianmag.com/science-nature/how.
- Klein L, Wittenberg E (2023). The decisive influence of malaria on the outcome of Grant’s Vicksburg campaign of 1863. Hektoen International Winter 2023. https://hekint.org/2023/01/19/the-decisive-influence-of-malaria-on-the-outcome-of-grants-vicksburg-campaign-of-1863/.
- Roser M, Ritchie H (2015) revised February 2022. Malaria. Published online at OurWorldinData.org Accessed from https://ourworldindata.org/malaria.
- Capanna E (2006). Grassi versus Ross: Who solved the riddle of malaria? Int Microbiol 9(1):69-74.
- Alphonse Laveran – Biographical. NobelPrize.org. Nobel Prize Outreach AB 2023. Sat. 18 Nov 2023. https://www.nobelprize.org/prizes/medicine/1907/laveran/biographical/.
- Anopheles. Merriam-Webster.com Dictionary, Merriam-Webster, https://www.merriam-webster.com/dictionary/anopheles. Accessed 21 Nov. 2023.
- Ronald Ross – Facts. NobelPrize.org. Nobel Prize Outreach AB 2023. Thu. 16 Nov 2023. https://www.nobelprize.org/prizes/medicine/1902/ross/facts/.
- Tran TM, Samal B, Kirkness E (2012). Systems immunology of human malaria. Trends Parasitol 28(6):248-257. doi:10.1016/j.pt.2012.03.006.
- Dong Y, Simões M, Dimopoulos G (2020). Versatile transgenic multistage effector-gene combinations of Plasmodium falciparum suppression in Anopheles. Sci Adv 6(20) 13;6(20):eaay5898. doi: 10.1126/sciadv.aay5898. eCollection 2020 May.
- Raghavendra K, Barik TK, Reddy BPN, Sharma P, Dash AP (2011). Malaria vector control: from past to future. Parasitol Res 108(4):757-779. doi: 10.1007/s00436-010-2232-0. Epub 2011 Jan 13.
- Tu Youyou – Biographical. NobelPrize.org. Nobel Prize Outreach AB 2023. Sat. 18 Nov 2023. https://www.nobelprize.org/prizes/medicine/2015/tu/biographical/.
- World Health Organization. World malaria report 2022. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO.
- Vaughan AM, Aly ASI, Kappe SHI (2008). Malaria parasite pre-erythrocytic stage infection: Gliding and hiding. Cell Host Microbe 4(3):209-218. doi:10.1016/j.chom.2008.08.010.
- Graves PM, Gelband H. Vaccines for preventing malaria (SPf66) (Review). Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No.: CD005966. doi: 10.1002/14651858.CD005966.
- Graves PM, Gelband H. Vaccines for preventing malaria (pre-erythrocytic) (Review). Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD006198. DOI: 10.1002/14651858.CD006198.
- Datoo MS, Dicko A, Tinto H, Ouédraogo J-B, Hamaluba M, Olotu A et al (2023). A phase III randomised controlled trial evaluating the malaria vaccine candidate R21/Matrix-M™ in African children. Available at SSRN: https://ssrn.com/abstract=4584076 or http://dx.doi.org/10.2139/ssrn.4584076.
- Johnson S (2023). Cheaper more effective malaria vaccine wins WHO approval. The Guardian October 2, 2023 1235 EDT. https://www.theguardian.com/global-development/
- Paul Müller – Biographical. NobelPrize.org. Nobel Prize Outreach AB 2023. Sat. 18 Nov 2023. https://www.nobelprize.org/prizes/medicine/1948/muller/biographical/.
- Julius Wagner-Jauregg – Biographical. NobelPrize.org. Nobel Prize Outreach AB 2023. Sat. 18 Nov 2023. https://www.nobelprize.org/prizes/medicine/1927/wagner-jauregg/biographical/.
JAYANT RADHAKRISHNAN, MB, BS, MS (Surg), FACS, FAAP, completed a Pediatric Urology Fellowship at the Massachusetts General Hospital, Boston, following a Surgery Residency and Fellowship in Pediatric Surgery at the Cook County Hospital. He returned to the County Hospital and worked as an attending pediatric surgeon and served as the Chief of Pediatric Urology. Later he worked at the University of Illinois, Chicago, from where he retired as Professor of Surgery & Urology, and the Chief of Pediatric Surgery & Pediatric Urology. He has been an Emeritus Professor of Surgery and Urology at the University of Illinois since 2000.

Leave a Reply