Shelley Grach
Chicago, Illinois, United States
In the Middle Ages, fear and superstition often stood in the path of helping the sick, as maladies were believed to result from the sins of the afflicted. These roadblocks were compounded by inherited hostility towards Jews, impeding Jewish participation in scientific education at educational institutions. The University of Montpellier in southeast France, established in 1220, seems to have been one exception. It was one of the few universities that allowed a small number of Jews to teach or study there, including Abraham Avigdor of Arles, “the first Provencal Jew to state expressly that he was in Montpellier and studied at its university.”1 After 1394 when the Jews were expelled from France, Padua provided some opportunity for Jews to obtain medical knowledge. The majority, however, learned their skills through private study and the development of a full library in Hebrew.
Jews translated medical documents, often from Arabic, into Hebrew and Latin, earning payment for their efforts and picking up deep medical knowledge. In the 13th century, Shem Tov of Tortosa translated the encyclopedia of medicine of Al-Zahrawi, known known in the West as Abulcasis and as the “father of surgery.” Another Jewish scholar and translator who advanced medical knowledge was Kalonymus ben Kalonymus (1286–1328). He translated several works from Arabic, including works of Galen, scientific and metaphysical treatises, and Avicenna’s Canon of Medicine, “the most important medical book in the High Middle Ages and certainly the most influential. . . . Arabic scientific works seem to have furnished the essential Jewish medical arsenal.”2 Jewish scholars could also study with mentors and obtain skills from father-physicians or knowledgeable family members. This legacy of handing medical knowledge down from generation to generation resulted in medical “dynasties” such as the Abenardut family.
The combination of a trusted physician and a powerful family medical heritage resulted in medieval Jewish physicians going beyond their medical role in their communities. They were what we would call “influencers” today: well compensated for their skills, they acted as judges and negotiators in local disputes, enjoyed tax exemptions, and served princes and popes.
The relationship between Jewish physicians and Christian patients was complicated and inconsistent. Despite legislation to prevent Jews from being licensed as physicians or treating non-Jewish patients (), much of this legislation was ignored. At times, Jews could only treat patients in conjunction with, or under the supervision of a Christian physician. Church leaders hesitated to have a Jewish healer seen as more important or powerful than a Christian and often barred Jews from treating the uneducated common folk, yet relied on Jewish physicians for themselves. Ultimately, “justifications like ‘public utility’, ‘urgent necessity’, ‘scarcity of Christian doctors’ were brought forward. . . simply put, society was not ready to reject the Jewish doctor.”3 Many Jewish doctors became court physicians (and advisors). Their presence was often included in formal court documents and papal dispensations, thereby justifying and supporting their expertise.
Societal views
“A society’s treatment of its ill, handicapped, and both mentally and physically disabled members informs us about far more than just the lives of these individuals; it offers insight into the society’s social values.”4
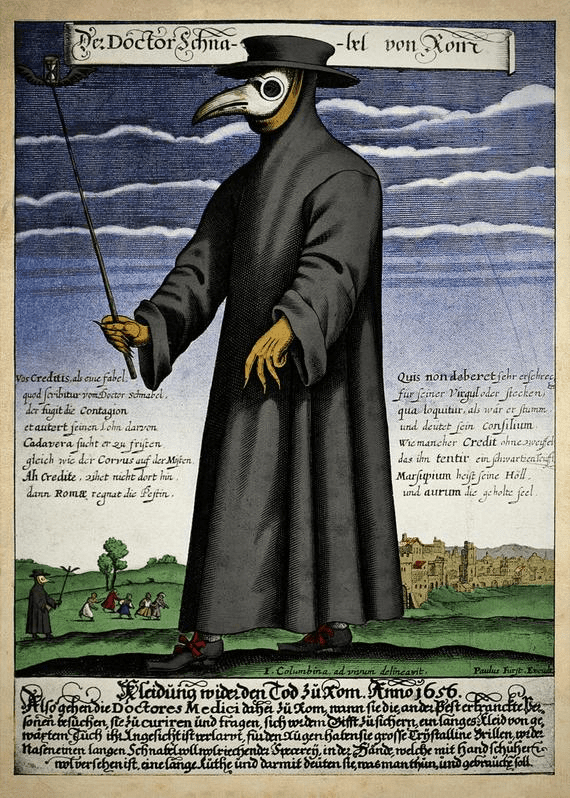
It is therefore not surprising to see “rabbi-physicians” develop during the Middle Ages. It was a powerful combination: the inherited focus on education and studying, the ability to read and translate complex medical sources in multiple languages, an emphasis on solutions through scientific evaluation, and the religious tradition of healing and serving the sick. One example is Jacob Zahalon (1630–1693), a physician and rabbi who oversaw a section of the Rome Ghetto during the bubonic plague. He worked closely with the Gentile physicians and documented his observations of the plague—“throughout his account, Zahalon reminds the reader that it was God who saved him.”5 Jewish medicine reflected Jewish values: intellectualism, kindness, and the doctor as a “partner to God.” As respect for Jewish physicians increased, so did their involvement in local civic decisions, especially when they also held rabbinic appointments.
Most female Jewish practitioners in the 14th and 15th centuries were accepted as midwives or “healers.” They typically learned through apprenticeships, rarely were able to attend the universities, and therefore followed the family learning model of Jewish male physicians. Often, they were “paid a full salary…. [and] sometimes accorded special honors such as exemption from certain sumptuary laws.”6 While Jewish male physicians often had restrictions on treating non-Jewish patients, there seemed to be fewer restrictions for women. This difference may have been due to the simpler, more routine procedures they carried out or simply that people felt more comfortable with a woman. It is also documented that they were considered “better suited” to treat women than male physicians. Yet the number of female healers and midwives was still very small: “In France between the twelfth and fifteenth centuries, women constituted only about 1.5 percent of physicians. . . . It is certain many more women practiced medicine than the meager historical record reflects.”7
Impact of the Black Death
When the Black Death began its march in 1346, it brought new opportunities for Jewish physicians to share innovative perspectives on public health measures; it also re-surfaced antisemitic accusations such as well poisoning, which resulted in anti-Jewish violence. From biblical times, plagues were viewed as the work of God and represented God’s ability to destroy or save according to mankind’s goodness or sinfulness. Yet there was minimal mention of plague (and how to counter its impact) in early Middle Ages’ Jewish laws or writings. The only advice given was to stay in the home, essentially early self-isolation. By the time of the Sefer Hasidim (The Book of the Pious, 1487), physicians were now urging people to “flee.” Over the next century or so, various rabbis gave incorrect medical advice, not understanding the true cause of plagues and instead citing “vapors” and planet alignment as their causes. As the Black Death progressed, Jewish physicians began to observe its causes and effects and documented their findings, providing more scientific facts than superstitions. Abraham Caslari practiced in Spain, and in 1349, he wrote “a treatise in eight chapters about the origins, treatment and prevention of the plague. . . . It was among the first works of its kind in any language, Hebrew or otherwise.”8 Caslari is an important example of an early step towards early modern scientific thinking. While not specifically Jewish in his perspective, he did include biblical references while deliberately omitting references to the demonic or to spirits. He also identified certain people as infection prone, although the underlying reasons for their ill health were firmly rooted in superstitious thinking.
Notably, other rabbis, Jewish physicians, and rabbi-physicians used the Black Death as a catalyst for research, observation, and documentation. Rabbi Narboni linked the plague to planetary alignment; Abraham Yagel focused on both the “theological and medical” in his writings and identified transmission through personal contact; Hyyam Vital, a student of Rabbi Isaac Luria in Safed, suggested a three-pronged approach of prayer, medicine, and intervention—a precursor to holistic medicine.
In addition to violent antisemitic accusations that accelerated during the Black Death, the underlying antisemitic policies that isolated Jews to ghettos or Jewish areas brought a heightened focus by Jewish physicians on better public health measures. We have examples of Jewish physicians appointed to positions as “city physician” or “ghetto physician.” Before, during, and after the Black Death, Jewish physicians worked with local governing bodies to improve health care, extend health care services such as apothecaries, and support embryonic social services. German Jews especially had “an expansive network of social service institutions that included hospices, hospitals, and sick care societies. . . . The community councils in Europe devised elaborate quarantine and treatment procedures to be implemented in times of plague and epidemic.”9 Jewish physicians did provide a measure of health care and consolation to the sick and provided documentation of what Jewish life was like during the Black Death.
Legacies
Although the medieval Jewish physician was often denied education in the formal sense, the inheritance of studiousness and documentation, assisted by the surge of translations of medical treatises into Hebrew and Arabic, helped overcome university quotas and outright denial of admission. Coupled with family legacy and training, the Jewish physician had both book-learning and practice from on-the-job experience in diagnosing, recommending remedies, and treating patients. The sheer lack of trained physicians generally opened the doors to Jewish doctors.
Jewish women also learned through apprenticeship, often with their own family members. Few had official licenses, but women healers were sought for their skills as well as their (perceived) non-threatening approach to treatment. They crossed religious and gender boundaries and were well compensated for their skills, as in the case of “Sara, who was granted a license by municipal authorities to practice medicine in 1419, for which she was paid an annual tax of 10 florins, was so successful that she was able to accumulate a considerable fortune—enough to buy a manor house.”10
Less quantifiable are anecdotes of Jewish physicians developing strong relationships with their patients. This may have evolved from the commandment to help and support the sick or from the importance of community and prayer as tools to sustain people. This skill was developed in the ghettos and in palaces. In the ghetto, the communities were small, families were familiar, and the survival and continuity of the Jewish people was a high priority. In the palace, the stakes for success were high, so the Jewish court physician was always on call, available to the prince, and was both a healer and a personal advisor.
Summary
Ironically, the rise of the medieval Jewish physician tells a story in which being the “other” contributed to being seen as possibly better than a non-Jewish physician: “That which Christians feared most about Jews, their otherness and exoticness, provided a source of comfort and hope to Gentile patients.”11 While antisemitism raged during the bubonic plague, and innocent Jews were accused of well poisoning and were burned alive, Jewish physicians were seen as possible saviors with their rational approaches to health. Today, our society places emphasis on collective healing via social justice, but in the Middle Ages, healing was focused on the individual, the family, and the stranger. This ability to blend the best scientific knowledge of the time with trust and two-way respect established the groundwork for how physicians practice medicine today. It is the story of a minority representing less than one percent of the population rising to a position of trust and knowledge that has spanned centuries.
End notes
- Joseph Shatzmiller, Jews, Medicine, and Medieval Society (Berkley: University of California Press, 1994), 29.
- Shatzmiller, 48, 51.
- Shatzmiller, 93-94.
- Ephraim Shoham-Steiner, On the Margins of a Minority (Detroit: Wayne State University Press, 2014), 184.
- Jeremy Brown, The Eleventh Plague (Oxford: Oxford University Press, 2023), 92.
- John Efron, Medicine and the German Jews (New Haven: Yale University Press, 2001), 85.
- Efron, 19.
- Brown, 72.
- Efron, 37.
- Efron, 20.
- Efron, 21.
Bibliography
- Brown, Jeremy. The Eleventh Plague: Jews and Pandemics from the Bible to Covid-19. Oxford: Oxford University Press, 2023.
- Efron, John M. Medicine and the German Jews. New Haven: Yale University Press, 2001.
- Shatzmiller, Joseph. Jews, Medicine, and Medieval Society. Berkley: University of California Press, 1994.
- Shoham-Steiner, Ephraim. On the Margins of a Minority: Leprosy, Madness and Disability Among the Jews of Medieval Europe. Detroit: Wayne State University Press, 2014.
SHELLEY STERN GRACH is a former director of civic engagement at Microsoft Corporation. Prior to Microsoft, Grach was vice president of sales at AT&T. Shelley has served on numerous nonprofit boards supporting increasing technology skills and employment opportunities for underserved individuals. She has also served on councils for both Chicago mayors and the state of Illinois. Stern earned a double B.A. at Oakland University and an M.A. in business from Central Michigan University. She is currently completing her masters in Jewish studies at the Spertus Institute for Jewish Learning and Leadership, where she is also a trustee.
Highlighted in Frontispiece Volume 16, Issue 1 – Winter 2024

Leave a Reply