Hans Erik Heier
Oslo, Norway
“While we have now begun to understand the cost of everything, we are in danger of losing track of the value of anything”
—Ann Oakley and John Ashton, 1993
Voluntary, non-remunerated blood donation in catastrophe
September 11, 2001: Two passenger airplanes are crashed into the World Trade Towers in New York, and one into the Pentagon in Washington, D.C. Three thousand people are killed; many are wounded.
Shortly afterward people across the US line up to donate blood; many of them have never donated before. During the next several days 500,000 extra units of blood are donated.1 The donors are not remunerated.
July 22, 2011: A terror attack occurs in the center of Oslo, Norway, and in an island outside the city. Seventy-seven people are killed; many are wounded. Immediately more than 1,000 people line up outside the Blood Bank of Oslo, demanding to donate blood. The majority have never donated before. Outside Oslo people also offer themselves as blood donors.2 The donors are not remunerated.
Catastrophic events mobilize voluntary, non-remunerated donors. The similarity to the “rally round the flag”-effect3 is evident.
Blood donation and remuneration 1914–36
During World War I several thousand transfusions were performed on the Allied side, nearly all of them by bleeding fellow soldiers when transfusion was needed. The donors usually got two weeks of extra leave as compensation.4
Between the two world wars blood donor registries were organized in main cities in Western Europe and in the USA and Canada. Remuneration varied considerably, but was quite extensive in some places. As an example, blood donors in Oslo, Norway from 1933 got NOK 40,- per donation. Today this equals NOK 1,600,- or 160 EUROs. In addition the Norwegian Red Cross, which organized the blood donor registry, charged the hospital NOK 10 (now = NOK 400 or 40 EUROs) for the service.5
During the late 1920s’ the Soviet Union started to develop a public transfusion system based on blood banks. When World War II broke out, the Soviet Union was the only country with a blood bank-based transfusion system. Donors were given an extra day off work, and various other rewards.6
Thus, there was no widespread tradition for voluntary, non-remunerated blood donation (VNRBD) between the two world wars.
Non-remunerated blood donation 1936–45
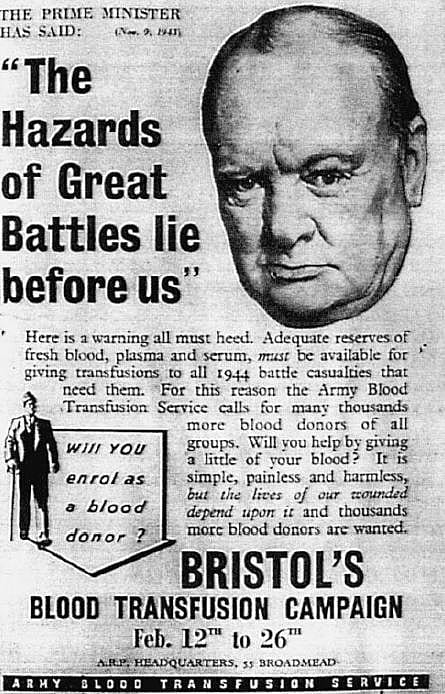
During the Spanish Civil War in 1936–1939 a blood bank-based transfusion service was organized in Barcelona. About 27,000 donations were collected; the donors were not remunerated.7 The Barcelona service inspired the first blood bank system in the UK, which was set up in London at the start of World War II in 1939. Again the donors were not remunerated. Gradually blood banks for VNRBD were set up throughout the UK, making VNRBD a part of the civilian support of the fighting soldiers (Fig. 1). More than 700,000 pints of blood were taken in England alone before the end of the war in 1945.8
In the US the American Red Cross organized a “Plasma for Britain” program in addition to whole blood donations for the soldiers, again without remuneration to the donors (Fig. 2).9
The French set up their Organisme de Réanimation-Transfusion in Algeria in 1942–3 and thus had a transfusion service following their armed forces when they advanced into Italy and France. Giving blood without remuneration became a sign of support of the new France, cleansed from fascism and oppression.10
By contrast, Germany never developed any civilian blood donation system to support the military forces. Instead they used blood from soldiers specially assigned for such service, to ensure that the blood used was of Aryan origin.11
VNRBD thus is a tradition from the allied fight against oppression during World War II. The catastrophic situation mobilized people to give blood to help those who fought.
Medical technology and blood donation after World War II

Medical technology had improved radically during World War II, and the need for blood in civilian health services increased shortly after 1945. Many countries established blood banks. International organizations, including the Red Cross/Red Crescent, the World Health Organization, the Council of Europe, and the International Society of Blood Transfusion all recommended that transfusion services be based on VNRBD, in keeping with the traditions from World War II.12 Recruitment of donors became more complex, however, since there was no longer a war or catastrophe. It is now clear that in normal situations the majority of VNRB donors are recruited by inspiration from donors in their personal networks, expressing social and personal identity. Feelings of duty and of altruism also play important roles.13
In 1964 Judith Graham Pool of Stanford University found that the coagulation enzyme which haemophilia A patients are lacking (factor VIII) could be recovered from the plasma of donors.14 The need for blood plasma for production of factor VIII then increased rapidly. As the need could not be met by VNRBDs, commercial centres for donation of plasma were established, especially in the USA and in poorer Latin American countries. Donors received a substantial remuneration, and poor people could survive by being ”professional” plasma donors.15
The English sociologist Richard Titmuss published his book—The Gift Relationship. From Human Blood to Social Policy—in 1970.16 He strongly recommended that all donation of blood and plasma be voluntary and non-remunerated. He had two main arguments:
1. Security
Data from the USA, Japan, and Germany showed that the transfusion transmissible diseases hepatitis B and ”non-A-non-B” hepatitis (later known as hepatitis C) were much more frequent in paid than in unpaid donors. This related to the relative poverty of many paid donors. Plasma donations at the commercial centers were often controlled poorly, as profit was the main goal for the owners.17
2. Solidarity, social acceptability, and identity
In keeping with the experiences from World War II, Titmuss saw VNRBD as a practice of solidarity and active engagement for fellow human beings. He also held that a VNRBD-based system is more effective than one which treats human blood as a commodity by paying the donors. He emphasized that the act of VNRBD is a highly ethical one and that it strengthens the social and individual identity of the donors.
The HIV/AIDS crisis 1980–86
The insufficient control of blood and plasma donations led to the global HIV/AIDS crisis in transfusion. Thousands of blood recipients were infected, and thousands died. In addition, thousands were infected with hepatitis C (HCV). Both HIV and HCV occurred most frequently among paid donors, strongly substantiating Titmuss’ first argument.18
The crisis provoked an intense focus on security against transfusion transmissible infections. Donor selection criteria were refined, and new tests for infectious diseases and for inactivation of infectious agents were developed. In 1998 Eastlund19 found small, if any differences in security between blood products from VNRBD and remunerated donors. Today Titmuss’ first argument seems of minor significance for the transfusion systems in Western countries. For blood collection in developing countries, the argument still seems valid, because the donors are often poor, and the incidence of transmissible diseases is high.
Current status of VNRBD
The global consumption of plasma products has increased rapidly and is much higher than what can be produced from the 110 million annual VNR blood and plasma donations in the world. A radical increase of VNRBD seems impossible, as the public does not perceive the situation as a crisis. Currently remunerated plasma donations cover more than 50% of the global consumption of plasma and plasma products.20 The majority are taken at plasma donation centres in the US. Much of the use is not evidence based, and there is reason to maintain that the consumption is too high, especially for immunoglobulins used to modulate poorly defined immune-mediated mechanisms.21
The Ovieto Convention of the Council of Europe prohibits the sale and purchase of human organs for transplantation.22 The Convention does not mention blood, but since blood is a liquid human tissue, buying and selling of blood, plasma, and products thereof in a market based on supply and demand remains a difficult ethical dilemma.
One may hope that large, randomized, controlled trials of immunoglobulin therapy in patients with well-defined diagnoses will lead to significantly reduced consumption. The consumption of erythrocyte concentrates for transfusion is decreasing in several Western countries,23, 24 making more VNRBD donors available for plasma donation. Gradually VNRBD may therefore come to cover the global use of blood, plasma, and products thereof.
A French historian of religion stated in 1988: “Blood donation is replacing ancient blood sacrifice.”25 Quite often established VNRB donors feel sorry or sad when they are no longer accepted as donors. The act of VNRBD says: “I sacrifice my blood for you,”—but also: “I am being seen. I am significant. I am a member of a community.” This substantiates Titmuss’ second argument. The value of VNRBD goes far beyond the price of the blood, for the donors and for the society as a whole.
End notes
- Schmidt PJ. 2002.
- Akkök CA. 2011.
- Baker WD., Oneal JR. 2001.
- Gunson H, Dodsworth H. 1996.
- Heier HE. 2019. Ch 13,.
- Starr D. 1998. Ch. 4.
- Duran-Jorda F. 1939.
- Gunson H, Dodsworth H. 1996.
- Starr D. 1998. Ch.4.
- Starr D. 1998. Ch.8.
- Starr D. 1998. Ch.7.
- Heier HE. 2019. Ch.17.
- Misje AH et al,
- Pool JG et al. 1964.
- Starr D. 1998. Ch.11
- Titmuss R. 1970
- Starr D. 1998. Ch 11.
- Starr D. 1998. Ch 14.
- Eastlund T. 1998.
- Octapharma AG. 2019
- Perez EE et al. 2017.
- https://www.coe.int/en/web/conventions/full-list/-/conventions/treaty/186 access Jan 7, 2020.
- Borkent-Raven BA et al. 2010.
- Transfusion Statistics Norway, 2017.
- Roux J.-P. 1991
References
- Schmidt P. Blood and Disaster – Supply and Demand. New Engl J Med 2002: 346: 617-620
- Akkök CA. The Oslo Blood Bank 22 July 2011. J Nor Med Ass. 2011; 131 (24): 2460-1.
- Baker, William D.; Oneal, John R. “Patriotism or Opinion Leadership?: The Nature and Origins of the ‘Rally ‘Round the Flag’ Effect”. The Journal of Conflict Resolution 2001; 45 (5): 661–687
- Gunson H, Dodsworth H. Fifty Years of Blood Transfusion. Transfusion Medicine 1996; 6 (Suppl. 1); 1-88. |
- Heier HE. Blod! Mellom magi, myter og medisin gjennom 2500 år (Blood! Between magics, myths and medicine through 2500 years). Oslo 2019: Kolofon Forlag. ISBN 978-82-300-1943-6 (in Norwegian) (Chapter 13)
- Starr D. Blood: An epic history of medicine and commerce. 1998: Alfred A. Knopf, New York. ISBN 0679-41875-X. Chapter 4: Blood on the Hoof.
- Duran-Jorda F. The Barcelona Blood Transfusion Service. Lancet 1939; 233: 773-775.
- Gunson H, Dodsworth H. Fifty Years of Blood Transfusion. Transfusion Medicine 1996; 6 (Suppl. 1); 1-88.
- Starr D. Blood: An epic history of medicine and commerce. 1998: Alfred A. Knopf, New York. ISBN 0679-41875-X. Chapter 4: War begins.
- Starr D. Blood: An epic history of medicine and commerce. 1998: Alfred A. Knopf, New York. ISBN 0679-41875-X. Chapter 8: Blood at the Front.
- Starr D. Blood: An epic history of medicine and commerce. 1998:Alfred A. Knopf,New York. ISBN 0679-41875-X. Chapter 7: Blood Cracks like Oil.
- Heier HE. Blod! Mellom magi, myter og medisin gjennom 2500 år (Blood! Between magics, myths and medicine through 2500 years). Oslo 2019: Kolofon Forlag. ISBN 978-82-300-1943-6 (in Norwegian) (Chapter 17).
- Starr D. Blood: An epic history of medicine and commerce. 1998:Alfred A. Knopf,New York. ISBN 0679-41875-X. Chapter 11: The Blood Boom.
- Pool JG, Gershgold EJ, Pappenhagen AR. High-potency antihaemophilic factor concentrate prepared from cryoglobulin precipitate. Nature 1964; 203: 312.
- Misje AH, Bosnes V, Gåsdal O, Heier HE. Motivation, recruitment and retention of voluntary non-remunerated donors: a survey-based questionnaire study. Vox Sang 2005; 89 (4): 236-44.
- Titmuss RM. The Gift Relationship: From Human Blood to Social Policy. Expanded and Updated Edition by Ann Oakley and John Ashton. London 1993: The New Press. ISBN 978-1565844032.
- Starr D. Blood: An epic history of medicine and commerce. 1998:Alfred A. Knopf,New York. ISBN 0679-41875-X. Chapter 11: The Blood Boom.
- Starr D. Blood: An epic history of medicine and commerce. 1998:Alfred A. Knopf,New York. ISBN 0679-41875-X. Chapter 14: The blood-services complex.
- Eastlund T. Monetary blood donation incentives and the risk of transfusion-transmitted infections. Transfusion 1998; 38 (September): 874-882.
- Octapharma AG. Personal information from Manager Nordic, Tor-Einar Svae 2019.
- Perez EE, Orange JS, BonillaFS et al. Update on the use of immunoglobulin in human disease: A review of evidence. J Allergy Clin Immunol 2017;139: S1-46.
- https://www.coe.int/en/web/conventions/full-list/-/conventions/treaty/186. Access Jan 7, 2020.
- Borkent-Raven BA, Janssen MP, van der Poel CL. Demographic changes and predicting blood supply and demand in the Netherlands. Transfusion 2010; 50: 2455-60.
- Transfusion statistics Norway 2017. https://www.helsedirektoratet.no/rapporter/transfusjonsstatistikk. Access January 4, 2020.
- Roux J-P. Il nous fait vivre, mais il nous fait peur: Les mystères du sang. Le Nouvel Observateur 1991; 1390: 6-11
Image Sources
- https://commons.wikimedia.org/wiki/File:Blood_transfusion_ww2_poster.jpg UK government. Public domain. Accessed February 23, 2019 and Jan 14, 2020.
- Whitman. Your blood can save him., poster, 1945; (digital.library.unt.edu/ark:/67531/metadc454/: accessed February 23, 2019 and January 14, 2020), University of North Texas Libraries, Digital Library, digital.library.unt.edu; crediting UNT Libraries Government Documents Department.
HANS ERIK HEIER was born in 1944. Studied medicine at University of Oslo (UiO) 1963-9. PhD (UiO) 1979. Acknowledged Specialist of immunology and transfusion medicine 1982. Master of Health Administration (UiO) 2000. Professor of transfusion medicine (UiO) 2004–11. President, International Society of Blood Transfusion (ISBT) 2002-4. Harri Nevanlinna Memory Medal, Finnish Red Cross Transfusion Service 2001. Honorary Member of ISBT 2010.
Submitted for the 2019–2020 Blood Writing Contest

Leave a Reply