John Graham-Pole
Antigonish, Nova Scotia, Canada
Hospital for Sick Children, Great Ormond Street, London, 1970: I’m astounded I’ve landed one of the coveted G.O.S. senior resident jobs. The academic nature of the place immediately daunts me. Everyone bows down to its status as the foremost pediatric research hospital in Europe, perhaps in the world, the faculty all confining their work to one or two specialized diseases. I hit the ground running to get up to speed on my bosses’ special interests—in one case, an almost exclusive diet of cystic fibrosis, in another, arcane metabolic and inherited disorders whose names—if they’ve yet been designated— are utterly unfamiliar.
But alongside ordering batches of previously unheard-of laboratory tests on each new patient, I have more mundane tasks to perform. My first Friday on call, the chief resident lets me know there’ll be a bevy of children being admitted for overnight blood transfusions.
“All thalassemics,” he adds. “Greek Cypriots from Kentish Town or thereabouts. We transfuse them pretty much every month, just to keep them alive. They’ll start showing up around five o’clock. Same every Friday—we bring them in overnight once the school week’s over, so they don’t miss out on their lessons. It can take a whole night and well into Saturday to get the job done.”
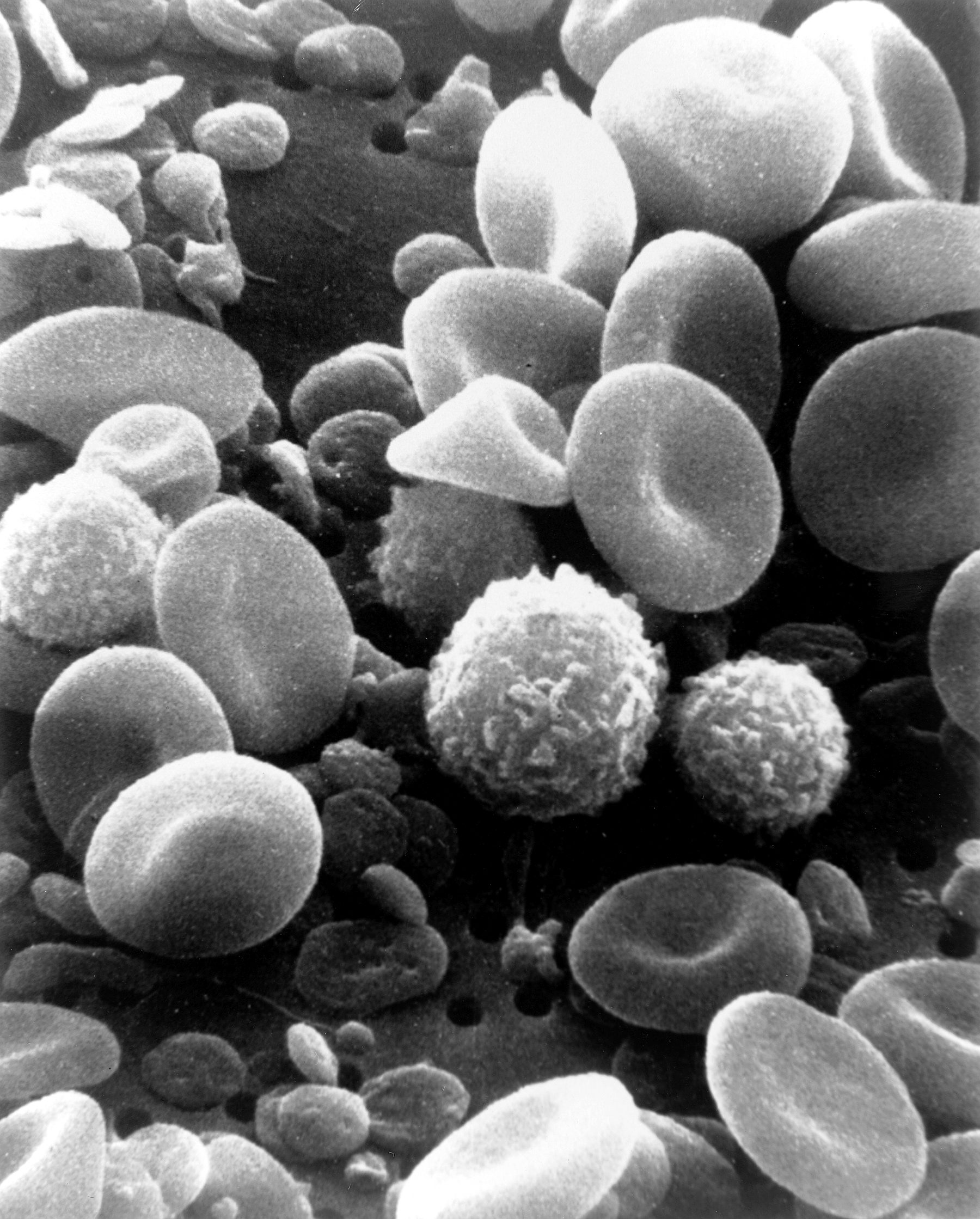
I struggle to recall my medical school teachings on the subject. I know these children have all inherited this gene named for the Mediterranean Sea (hence, θάλασσα), which renders them critically anemic from soon after birth. I recall glazing over the complex explanations in my genetics textbook, but the word hemoglobinpathy had somehow stuck—that some genetic defect in these children stops them from making any normal hemoglobin in their red blood cells. So they end up needing blood transfusions every month if they’re to even live, let alone thrive and grow. And the constant effort to generate fresh red cells of their own causes their bone marrow spaces to expand inexorably, so many of their bones, especially those of their faces and skulls, become hugely deformed—a condition called bossing that, once seen, is instantly recognizable.
These young ones also get overloaded in a few years with all the iron being released from their transfused red cells, which becomes highly toxic especially to their hearts and livers and hormone-producing glands. So their growth is stunted, and full post-pubertal development a distinct rarity: the adolescent boys’ voices often don’t break, and the girls rarely develop adult-sized breasts, or even go through menarche. So our transfusions may be lengthening their lives but they’re adding fuel to the flames by pouring more iron into their systems. All in all, a short and not very happy life.
We house officers have more immediate reasons for asking why our maker created this particular challenge to humankind. Where the rubber really meets the road—for both the children and for us—is that from an early age, it gets harder and harder to locate a virgin vein where we can get our I.V.’s started. Two of the eight of us are on call every weekend, starting Friday evening at five o’clock, and we quickly learn that we’ll be spending most of the night dragging our I.V. trays from bed to bed as we struggle to keep the blood flowing down these children’s scarred and brittle veins. There’s even some competitiveness about how few we have to start, then restart, before a transfusion is finally done, often not before elevensies on Saturday morning.
We set our I.V.’s up on the youngest patients first, so the nurses can get them settled for bed at a reasonable hour. No mean task, because the children derive some relief from these otherwise dreaded admissions by hanging out with their friends, playing games to take their minds off the trauma to come, or simply bemoaning their miseries. I’d overheard two ten-year-olds comparing numbers of sticks during their last admissions.
“He poked me here, then here, then here,” says one, pointing out each in turn. “I told him this is my best vein,” now indicating an unlikely site on her left wrist, “but he just wouldn’t listen. I’d like to stick it right in him, see how he likes it.”
Causing me to resolve to always query my patients about their favored veins. But it’s often harder still for the teenagers, because their veins are so scarred we may not establish any blood flow, even when we’re lucky enough to thread a 25-guage catheter in. Parents often insist on sitting through the whole ordeal, which piles on the stress of the whole situation.
My spirits, already at their low point on this first Friday on-call, plummet at the sight of Ilena’s name on my list. At eighteen, she’s the oldest of the Cypriot girls, and rumor has it on her last admission she flirted with breaking existing records for the number of I.V.’s started. It’s already eight-forty-five when I get to her bedside, and I’m astounded to find that Liz Letsky, the hematologist primarily responsible for these children’s care, is still here. A vivacious Jewish woman in her mid-thirties, she seems to know her patients’ life histories as intimately as their case histories. But I’ve never known faculty members hang around this late.
What’s going on? Is Ilena’s illness finally getting the better of her?
But it looks more like a birthday party than a deathbed scene. Ilena and Dr Liz, along with two other teenage girls decked out in colorful pajamas, are tucking into large chunks of cake, topped with a liberal layer of lurid pink icing. And washing it down with what looks to all the world like hard cider. At the sight of me trailing my tray behind me, Ilena clambers off her bed, rises to her full four-feet nine, and greets me with a huge beam.
“Doctor, I am the first!”
“Ilena, I’m very sorry to say you’re my last. I got way behind with those little ones. I’m really sorry.”
“No, no, doctor. You don’t understand. I am the first!” I take in that she’s blushing, which only serves to deepen the mystery. Dr Letsky takes note of her patient’s embarrassment and comes to the rescue.
“John, you are looking at the very first of all my young women patients to menstruate. Yes, Ilena has started her periods! Now, isn’t that cause for celebration?”
It’s my turn to blush.
Swept up in the party spirit, the full significance of what I’ve witnessed doesn’t hit me till I’m settling down to sleep, sometime well after midnight. A G.O.S. medical record has been broken: despite all the toxic iron deposited in Ilena’s ovaries, the transfusions that have kept her alive must have spared a small part of her reproductive capacity. Ilena has become the first in two generations of female thalassemia patients at the hospital to menstruate; maybe all the blood, sweat and tears are worth it.
—
2016 Postscript: In the past thirty-plus years, several thousand patients have received stem cell transplants for thalassemia major; their current expectation of cure is about 80%.
JOHN GRAHAM-POLE is emeritus professor of pediatric oncology and palliative care from the University of Florida. He’s published/co-edited six books on arts health and poetry, and had short stories and essays published in Ars Medica, CMA Journal, Hektoen, Journal of Poetry Therapy, Medical Humanities, and Yale Journal of Humanities. He has just completed a novel and a memoir. He co-founded the Center for Arts Medicine (www.arts.ufl.edu.cam), and works with artists, health professionals, and family caregivers, to promote the expressive arts in our physical, psychological, and social well-being. He lives in blissful retirement with his wife, Dorothy, in Antigonish, Nova Scotia.

Leave a Reply