Gregory Rutecki
Cleveland, Ohio, United States
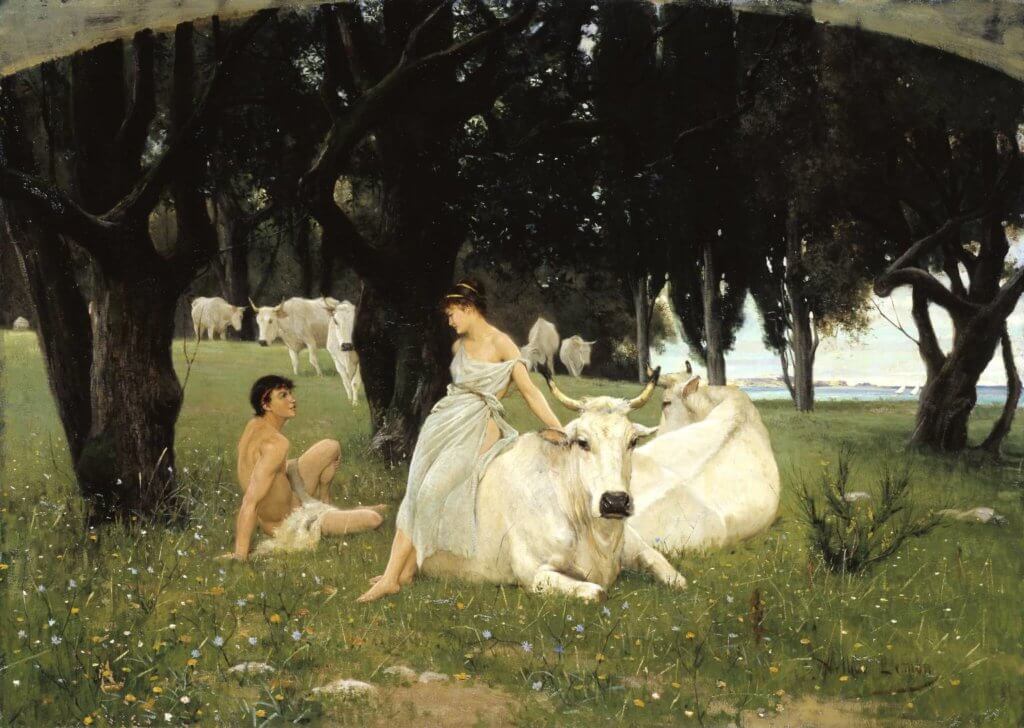 |
| Daphnis & Chloe, by Henry Woods, R.A |
William May and Samuel Shem have described inadequacies of doctor-patient relationships that are characterized as code models.1,2 May observed that these medical codes binding patients and their physicians together shape relationships similar to habits or rules, are aesthetic, and value style over compassion. Shem wrote The House of God when these codes were prevalent models for trainees, and observed that physicians-in-training learn how to deal with patients’ bodies and ailments but not how to be with patients as people.3
My own residency in 1974-1977—concurrent with the The House of God—imbedded such a code into my earliest patient encounters. Medical knowledge, proficiency, and skill were the ideals. Best practice was extolled at morning report: quoting journals, looking at peripheral smears, and “covering each and every clinical base”—arcane or not. To crusade against death as long as possible, without encouraging personal humanistic involvement with patients, was the accepted norm.1 Compassion, literally “as suffering with,” had its disadvantages in the context of 1970s academic patient-doctor interactions.1 But while I was still young and in private practice, a patient named Chloe changed my healing style forever.
It was 4 a.m. and my phone rang. Chloe was in the emergency room. She was a carefree and soon-to-be-married twenty-one-year-old with a rare disease—hemolytic uremic syndrome, or HUS—that often irreversibly wipes out blood cells and kidney function. Since HUS had a high rate of death and complications, if I cured Chloe I would be a “morning report hero.” Sick patients with rare diseases established the clinical reputations of young clinicians like me. It was not the patient per se, but rather my skill that mattered. What Chloe really needed was absent—a compassionate healer.
My heart sank when I first met Chloe, as I realized that her previously uncomplicated life would change irrevocably. Her plaintive face was more than a testing ground for HUS and my expertise. I saw a scared young woman in pain, and for the first time in my career I realized the essence of doctoring was not that of a one-dimensional crusader who diagnosed and cured rare diseases. This young clinician needed to see a much bigger picture to be an authentic healer.
Chloe was in for the long haul. Needle sticks, artificial kidney treatments, and other forms of blood purification were a daily ritual. She had a phobia of needles, and as we talked through her sobbing she slowly accepted uncomfortable but essential treatments. After two months of repeated poking, piercing, and prodding, and countless detours involving infection, bleeding, and ventilators, her blood counts finally normalized.
Unfortunately, not everything fell in line. She was still in kidney failure. Three, four, and five months passed without a drop of urine. She and I learned things about each other no one else knew. She was terrified that she would not be able to marry and have children. I showed her pictures of my wife and boys and told her to hang in there. Was I nurturing false hope? Although it was difficult for me to be optimistic, I never wore a frown when we made eye contact. Nearing a point of no return at six months, Chloe said she was making urine. I was pessimistic, but drew blood tests anyway, which confirmed she had working kidneys! We were both tearful at the end of this shared and lengthy healing journey. Our daily personal talks would cease, but each of us would be changed forever. My change was critical—Chloe was the first patient I saw as a real person in need and not merely a challenge for my medical skills.
A year later she invited me to her wedding. When my wife and I arrived, the priest asked if I was Chloe’s doctor. I said yes. When the ceremony started, I was asked to stand. The priest told the congregation that the bride and groom wanted them to know that she would not be here for her special day if not for me. Her grandmother came up and tearfully hugged me. I almost backslid into the adulation of a job well-done at morning report. But the personal significance of her special day refocused me. I was one of the first to know about the birth of her first child, and the holidays never pass without a card from her.
I was fresh out of training when I cared for Chloe—a hot shot, journal jockey whose cures were like notches on a gun. Chloe made me a caring, holistic physician and there would be no turning back. Now I am nearing retirement. Medicine has been a demanding mistress. There were unpredictable and frequent times away from a wife and two sons. There were sleepless nights and stress-filled days that inevitably accompany any physician’s investment in skill and empathy. My experience with Chloe embodied all the reasons why I became a physician. Our relationship—forged in the fire of life-threatening illness—became a paradigm that has endured. Chloe changed the trajectory of my professional life, and more so, my identity as an authentic healer.
Samuel Shem sensitively captured the best of the doctor-patient relationship in The House of God:
“The ‘we’ (doctor and patient) . . . which seemed so solid . . . to hold this ‘we’ . . . That was my job as a doctor. To use my experience with others who had suffered and my vision born of that experience to bring someone who is out on the edge of the . . . ‘sick’ into the current of the human . . . This is healing . . . This is what good doctors do. We are with people at crucial moments of their lives, healing.”2
The best part of this healing is that it touches the body, soul, and mind of both patient and healer with joyful memories that will last forever.
References
- May W.F. Code, covenant, contract, or philanthropy. Hastings Center Report 1975; 5:29-38.
- Shem S. The House of God. New York, New York, 1978.
- Shem S. Mount Misery. 1998; Ivy-Ballantine, N.Y. p.497-498
GREGORY W. RUTECKI, MD, received his medical degree cum laude from the University of Illinois, Chicago (1974). He completed internal medicine training at the Ohio State University Medical Center in 1977 and a fellowship in nephrology at the University of Minnesota in 1980. After 12 years of private nephrology practice, he re-entered Academic Medicine at The Northeastern Ohio Universities College of Medicine (awarded “Master Teacher” designation) and became the E. Stephen Kurtides Chair of Medical Education at Evanston Northwestern Healthcare and Professor of Medicine at the Feinberg School of Medicine, Northwestern University. He now practices medicine at the Cleveland Clinic.
Spring 2018 | Sections | Doctors, Patients, & Diseases

Leave a Reply