Richard de Grijs
Sydney, Australia
When the UK’s National Archives launched the Surgeons at Sea project,1 many media outlets focused on one outlandish claim from the curators’ summary of highlights. In June 1825, twelve-year-old Ellen McCarthy was on board the Elizabeth from Cork (Ireland) to Quebec (Canada) when the ship’s surgeon reported that she
Complained yesterday evening [11 June] of pain in the bottom of the belly increased on pressure, abdomen hard and swollen, picks her nose, starts in her sleep, bowels constipated, pyrexia [fever], tongue foul, pulse quick, skin hot, great thirst.2
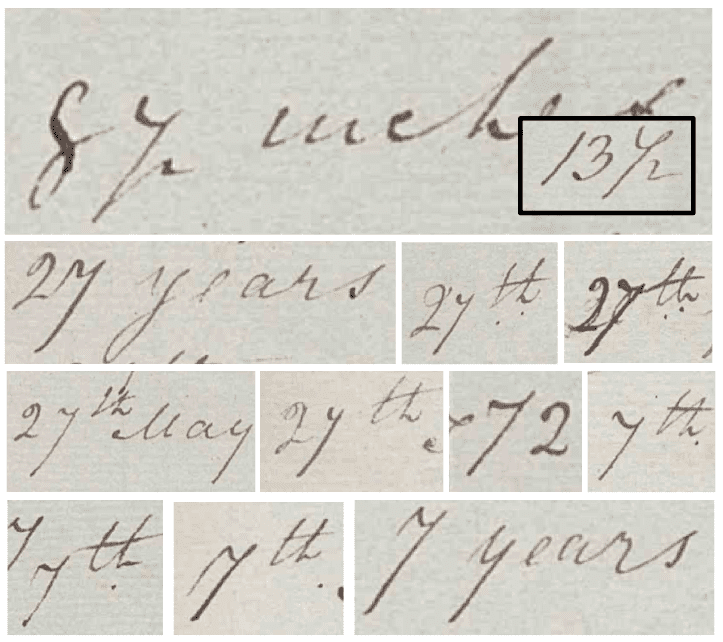
The surgeon gave his patient a cocktail of medicines, although of unknown composition; his notes are too condensed for current experts to fully decipher. The next morning, “Her mother brought me a lumbricus [intestinal worm] … 8½ inches [21.6 cm] long which the patient vomited. The medicine operated well.” The National Archives’ curators appear to have misinterpreted the surgeon’s notes, instead suggesting that the helminth’s length was 87 inches (2.2 m). Careful analysis of his scribbles supports this impression (see figure). Historical records of intestinal parasites “of an enormous size” report lengths of up to 22 inches (56 cm),3 but 87-inch-long helminths are unheard of.
On 15 June, young Ellen was “very ill and feverish”; on the 17th she had been “very feverish thro the night and … at time[s] delirious …, [her] teeth covered with a black crust.” To ease her symptoms, the surgeon prescribed a range of treatments, including administering barley water “made palatable with sugar, no medicine feels better,” calomel (a laxative of mercury chloride), jalap (a laxative tuber), and a tablespoon of brandy punch every two hours. However, none produced better results than oil of “terebinth”—turpentine4:
The rectified oil of Turpentine is a medicine much less used than it deserves to be. The reason probably is, the fear of its producing violent effects on the alimentary canal and urinary organs.5
The laxatives prompted his patient to pass “a vast quantity of offensive slimey matter.” On the night from 16 to 17 June, she expelled two additional roundworms, 7 and 13½ inches long. By 29 June, the surgeon finally declared his patient “convalescent.”
Intestinal worms were a common, “unrelenting scourge” in maritime life:
It is not known how lamentably men are troubled with these offensive Vermin, sometimes in the Bowels, sometimes in the Liver, and sometimes in the Stomach; and indeed, some people have a certain habit and humour fit to breed Worms, especially at some times.6
Weight loss was a common early sign of worm infestation, but it was often attributed to malnutrition. Intestinal parasites were thought to mostly affect young children and “sickly adults.” They were described by the American physician William Potts Dewees (1768–1841) as “producing emancipation, a swelled hard belly, gnawing or pungent pain in the stomach, pale countenance, fetid breath, and irritation of the nostrils.”7
On 13 July 1827, Royal Navy doctor James Patton reported a worm infestation in twelve-year-old Eliz Byate:
The Mother … stated to me that this child had fallen off much in flesh during the voyage—The Girl appears emaciated, complains of wandering pains in her Belly; she is sometimes costive, sometimes free in her Bowels—Is attacked with fever and slight convulsion at night, which disappears during the day—She is observed frequently scratching her nose and anus; these symptoms with the others before enumerated disposed me to suspect intestinal irritation by worms.8
Other symptoms could include coughing, anemia, weakness, extreme lethargy, headaches, bowel irregularities or discomfort, “nausea, vomiting … itching of the nose, and various convulsive affections,”9 unusual food cravings—including geophagy or “dirt eating”10—or loss of appetite, interrupted cognitive or physical development, and, in children, retarded sexual growth. Some symptoms might have been related to the occurrence of helminths not only in the intestines but also in the nose, larynx, mouth, stomach, appendix, peritoneal cavity, and gall bladder.11
At least some surgeons attributed the proliferation of intestinal parasites to the human body’s “viscous humors.” French apothecary and physician Jean de Renou (1568–1620) was convinced that worms contained large quantities of “putrid humours; for there worms are generated, where putretude resides: for, Corruption is their Mother.”12 He theorized that the parasites originated
… from all altered and putrid matter, stones, bones, wood, fruit, cheese, flesh; and all things found at first to turn into worms … some are procreated of salt: they are also generated … in the intestines, and other parts of man’s body.13
Oceanic voyages were prone to helminth infestations because of the often poor preparation of rotten meats that had been kept in unrefrigerated conditions for lengthy periods. Pork, a maritime mainstay, deteriorated quickly; its consumption is routinely associated with the spread of communicable diseases in the close confines typical of contemporary vessels.14,15 Captain Woodes Rogers (1679–1732) attributed the ailments affecting Brazilian coastal residents to the consumption of raw meat, suggesting that “The chief Distemper of the Natives is the Worms beforemention’d.”16
Poor diets were to blame for the spread of worms. Sea surgeon John Moyle (d. 1714) blamed worm infestations on “sometime[s] eating of much raw Fruit, or other vitious [vicious] Diet; that makes fit matter for Worms to Generate,”17 while Johann Dietz (1665–1738), the military surgeon, pointed out that on the ship he served on,
… there was against the mainmast a great tub, fixed some distance from the deck, containing water that was often stinking and full of little worms, for the general drinking.18
Sailors were therefore advised to consume certain dietary items while at sea: “Many crude indigestible vegetables, immature fruits, legumina, sweets, cheese and fresh fish proved useful in restoring a person’s health suffering worm invasion.”19
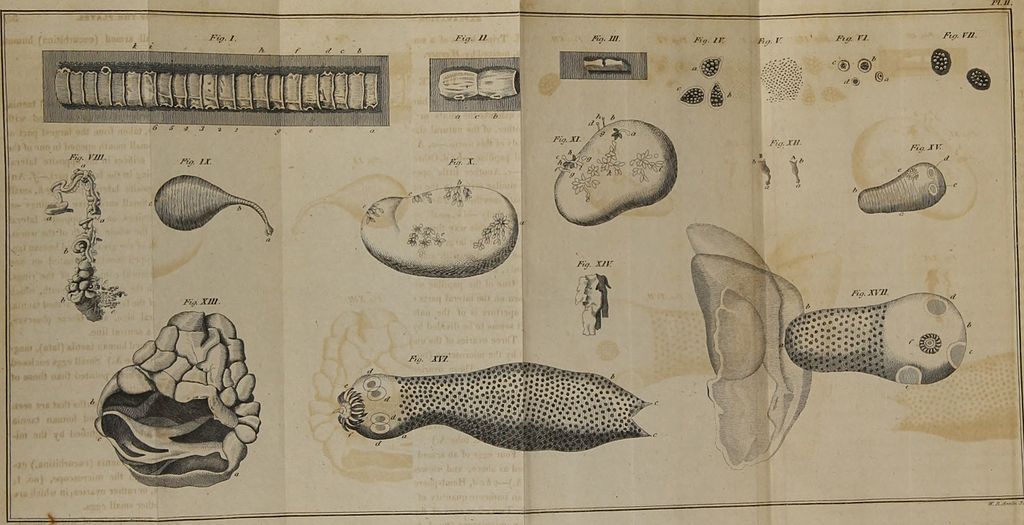
Helminth infections have plagued humanity since ancient times.20,21 In seventeenth- and eighteenth-century texts, helminths were often simply referred to as “worms,” without distinguishing among the broad categories we recognize today—tapeworms (cestodes or “solitary” worms), flukes (trematodes; e.g., clonorchis), and roundworms (nematodes; e.g., Guinea worms, whipworms, and hookworms). Some physicians argued that there were two types of tapeworms—“No species of intestinal worms is more destructive to human nature, or more difficult to be totally destroyed”22—the ascaridies, “being small worms,” and the round and long lumbrici teres.23 During the first half of the twentieth century, the most common intestinal parasites among Chinese steerage passengers arriving in the US were, in order of decreasing frequency, roundworm, whipworm, hookworm, and clonorchis.24
Yet claims that worms self-generated inside the body were persistent, as we learn from sea surgeon John Atkins (1685–1757), with “the Colour, Shape, and Magnitude of such Worms, being clearly owing to the [body] Parts they breed in, and the Matter they are bred from,”25 although their spontaneous generation required “crude putrefying Food, meeting with a weak Concoction, and [a] Deficiency of Bile.”26
Worm infestations did not usually result in death, but symptoms could be debilitating. As a consequence, a range of remedies, treatments, and cures found their way into everyday life.27,28 Medicines, laxatives, and purgatives such as wormwood-infused absinthe, corralina, aconite, ignatia, chia, spigelia, belladonna, nux, ascaridol (oil of chenopodium), mercury (calomel), turpentine, a combination of tartar emetic (a medicine that triggers vomiting) and sodium chloride, myrrh and aloes, lemon juice with ashes, sulfur/spirit of vitriol, meat broth, tobacco, and wormseed were at different times thought to kill or sterilize helminths or their eggs—a form of vermicide—or flush them out, a process known as vermifuge. Common treatments tended to prescribe ingestion of bitter medicines. John Woodall (1570–1643) concluded that “almost all bitter things kille wormes,”29 a suggestion wholeheartedly supported by the apothecary Robert James (1703–1776): “in such Cases, highly bitter Medicines are required.”30
If worms could not be flushed out of one’s system, it was deemed best to let them exit the skin on their own accord, sometimes encouraged by application of salves, ointments, oils, or plasters (e.g., soft bread cataplasms). If a worm was severed too early, the remainder of its body might cause serious infection31:
[T]he man who by the presence of Guinea worm became disabled from duty, was the sail maker and boatswain … About 4 days prior to his application to me, he had observed a small red and elevated spot at the anterior part of the inner ankle, at which, there had, for a week, been a painful degree of irritation. From intemperate habits, a debilitated state of the nervous system had been established and local irritation with constitutional derangement very soon followed the retraction of the ectoxoa [parasite], this having resulted from the man detaching the head with about 2 inches of the body, from the cuticle, when supposing the elevation to be a pustule he used forcible pressure.32
Instead, a more appropriate treatment was recommended:
The orifice at which the worm protruded was each day examined and on the second portion appearing, it was carefully attached to a small strip of adhesive and retained by the aperture. On the removal of each cataplasm an old portion of this nematoidea was obtained and similarly secured until the whole of it was removed … At the end of 30 days the whole of the worm having been abstracted his general health no longer being impeded by this source of irritation became improved and the aperture closed without ulceration, as had been expected.33
As common as helminths were in people’s intestines, physicians were equally inventive in pursuing treatments and cures, usually resulting in a full recovery.
References
- Surgeons at Sea: Royal Navy Medical Officers’ journals, 2010. UK National Archives. https://www.nationalarchives.gov.uk/surgeonsatsea/.
- Power, P., 12 June 1825. Journal of the Convict Transport Ship Elizabeth between the 4th of May and the 21st of June 1825. UK National Archives, ADM 101/76/9. P. 23.
- Milne, A., 1798. Surgeon’s journal from the L’Aimable, 5 September 1797 to 4 September 1798. UK National Archives, ADM 101/81/4. Cited by Convertito, C., 2011. The Health of British Seamen in the West Indies, 1770–1806. PhD Thesis, University of Exeter, UK. P. 161.
- Power, 1825. Op. cit. P. 27.
- Peirson, A. L., 1821. Clinical Remarks. No. 2. New England Journal of Medicine, 10, 231–234.
- Moyle, J., 1702. Chirurgus Marinus: or, the Sea-Chirurgion. 4th ed. Chapter L. P. 315.
- Dewees, W. P., 1842. A Treatise on the Physical and Medical Treatment of Children. Philadelphia PA, Lea and Blanchard. P. 485.
- Patton, J., 1827. Medical and Surgical Journal of Her Majesty’s Convict Ship Persian between the 11th April 1827 to 10th August 1827 during which time the said female convict ship has been employed in a voyage from England to Hobart Town, Van Diemen’s Land. UK National Archives, ADM 10/058/07.
- Mustakeem, S. M., 2016. Slavery at Sea, Chapter 6: The anatomy of Suffering. Chicago IL, University of Illinois Press.
- Sheridan, R. B., 1985 Doctors and Slaves: A Medical and Demographic History of Slavery in the British West Indies, 1680–1834. Cambridge, Cambridge University Press. P. 217.
- Report of the Surgeon-General U.S. Navy, 1906. Washington DC, Government Printing Office. P. 107.
- de Renou, J., and Tomlinson, R. (ed.), 1657. A Medicinal Dispensatory. London, J. Streater and J. Cottrel. P. 269.
- Ibid. Pp. 468–469.
- Cockayne, E., 2008. Hubbub: Filth, Noise, and Stench in England, 1600–1770. New Haven CT, Yale University Press. P. 95.
- Mannix, D., and Malcolm, C., 1969. Black Cargoes: A History of the Atlantic Slave Trade. New York NY, Viking Press. P. 121.
- Rogers, W., 1712. A Cruising Voyage Round the World. London, Andrew Bell and Bernard Lintot. P. 61.
- Moyle, 1702. Op. cit. P. 254.
- Cockayne, 2008. Op. cit. P. 57.
- Van Solingen, H., 1792. An Inaugural Dissertation on Worms of the Human Intestines. New York NY, T. and J. Swords.
- Shulman, S. T., 2004. The History of Pediatric Infectious Diseases. Pediatric Research, 55, 163–176.
- Grissom, J. H., 2014. Parasitic Worms in Early Modern Science and Medicine, 1650–1810. PhD Thesis, University of Oklahoma, Norman.
- Van Solingen, 1792. Op. cit.
- Mustakeem, 2016. Op. cit.
- Annual Report of the Surgeon General of the Public Health Service of the United States, 1922. Washington DC, Government Printing Office. P. 208.
- Atkins, J., 1734. The Navy-surgeon: Or, a Practical System of Surgery. London, Caesar Ward and Richard Chandler. P. 372.
- Ibid. Pp. 372–373.
- Kehoe, M. C., 2003–2023. Parasites and Their Treatment During the Golden Age of Piracy. In: The Pirate Surgeon’s Journals. Tools and Procedures. P. 3; http://www.piratesurgeon.com/pages/surgeon_pages/parasites3.html.
- Moyle, 1702. Op. cit.
- Woodall, J., 1617. The Surgions Mate, Or, a Treatise Discouering Faithfully and Plainely the Due Contents of the Surgions Chest. London, Edward Griffin. P. 213.
- James, R., 1764. Pharmacopoeia Universalis: Or, a New Universal English Dispensatory. London, J. Hodges and J. Wood. P. 201.
- Bourgeois, N., 1788. Voyages intéressans dans différentes colonies françaises, espagnoles, anglaises, &c. Paris, Jean-François Bastien. P. 476.
- Surgeon’s Log of the ‘Dudbrook’, Plymouth to Fremantle, November 1852. https://enrolledpensionerforcewa.org.au/wp-content/uploads/2019/09/Dudbrook-the-Complete-Story-c2017.pdf
- Ibid.
RICHARD DE GRIJS, PhD, is a professor of astrophysics at Macquarie University in Sydney, Australia. He has a keen interest in the history of science and navigation. Richard is also a consultant, as well as a volunteer speaker and guide on the historical tall ships at the Australian National Maritime Museum.
Highlighted in Frontispiece Volume 15, Issue 4 – Fall 2023

Leave a Reply