Mariam Abdulghani
Michigan, United States
In the early 1970s, the Bangladesh Liberation War caused a mass exodus of refugees from East Pakistan (now Bangladesh) into West Bengal, India. Some ten million people found sanctuary in camps along the Indian-Pakistan border, where the conditions of war during the monsoon season led to a cholera outbreak. The disease attacked a population already debilitated by exhaustion and starvation, leading to a heavy death toll. Some 30% of patients died of illness within a few days.1
Further exacerbating this issue, the government of India, the state government of West Bengal, and non-governmental agencies were unable to provide enough intravenous saline solution and trained medical personnel to meet the needs of and treat cholera effectively in an increasingly ailing population.2
One witness to this tragedy was Dilip Mahalanabis, a pediatrician and clinical scientist working in one of the refugee camps in West Bengal. He had already become familiar with ORT through his work on the staff of the Johns Hopkins Center for Medical Research and Training in Calcutta (JH-CMRT).3
As a mixture of water, glucose, and salt, ORT administration was known to cause glucose absorption in the small bowel, which in turn increased the absorption of sodium and water. This phenomenon was found to occur even in the presence of cholera enterotoxin.4,5
Furthermore, early hospital trials for ORT in the 1960s demonstrated the effectiveness of ORT as a maintenance therapy in patients with cholera.6,7
These results notwithstanding, the consensus among medical experts was that ORT should be used with extreme caution and only in a hospital.8,9 Investigators stated that ORT should not be promoted for home or ambulatory treatment for diarrhea.10
At the time, the most common treatment for diarrhea was the much more expensive intravenous rehydration therapy via saline solution in a hospital setting.11 Aware of these recommendations, Mahalanabis and his team wondered whether ORT could be used outside of a hospital.12 With the assistance of JH-CMRT and of governmental and voluntary agencies, Mahalanabis and his team began administering oral fluids to all patients not in urgent need of intravenous therapy.13
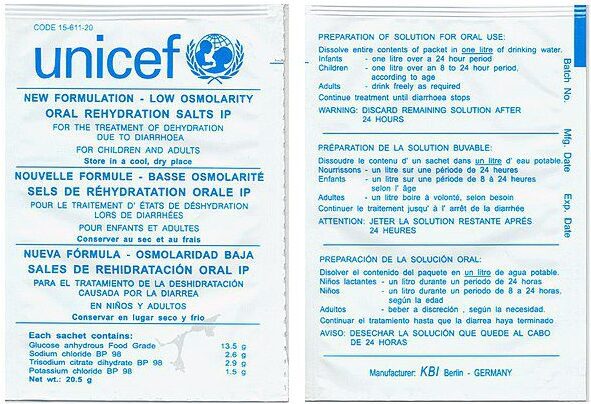
His team weighed the various ingredients and placed them in plastic bags, sealing them with a hot iron. All materials and equipment used for packaging and dispensing were obtained locally, and the cost of each packet was around 1.5 cents per liter of fluid. When dissolved, the mixture provided an electrolyte composition of 90 mEq sodium, 30 mEq sodium bicarbonate, 60 mEq chloride, and 121 mM glucose.14 The advantages offered by ORT included the minimal cost of preparation and transport, local availability of ingredients, and ease and safety for use by non-medical persons.15
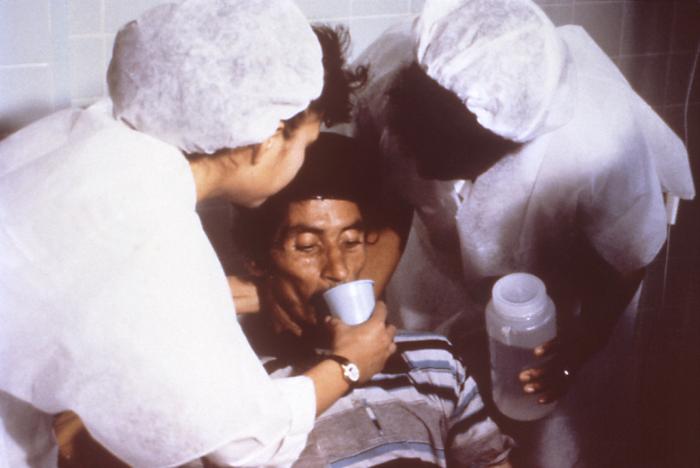
These packets were rushed to the camps, where family members collected the solution in small cups from central containers and urged their loved ones to drink large volumes. Health workers were primarily responsible for replenishing supplies in the containers and for checking on patients.16
In a personal account, Dr. Mahalanabis summarized his overall experience: “[The] camp condition was appalling.” As intravenous fluids were “scarce. . . . we went ahead with ORT for all. Mothers, relatives, friends, [and] anybody available were mobilized to give oral rehydration salts to all patients. We had to ration intravenous fluid for the very moribund in shock.”17
Over a period of eight weeks during July and August 1971, thousands of patients were treated.18 The case fatality ratio was 3.6%, compared to rates of 20–30% in other camps where only intravenous solutions were used.19 Thousands of lives were saved. Yet most physicians were not convinced. Many deemed it an inferior therapy, one to be used only when intravenous fluids were unavailable. Several medical journals even rejected Mahalanabis’s paper describing his experiences, but researchers like Mahalanabis persisted and launched other community projects to demonstrate the efficacy of ORT.20
It was not until Dhiman Barua, a cholera specialist from the World Health Organization (WHO), visited the refugee camps that ORT gained greater attention. He was impressed by what he saw and understood the implications of using ORT to manage diarrhea in children—he proceeded to promote ORT for cholera and childhood diarrhea, mobilizing the support of UNICEF and encouraging discussion on a global scale.21,22 His “unyielding pressure,” along with the efforts of researchers, led to the creation of WHO’s Diarrheal Diseases Control Program in 1978 and the popularization of ORT throughout the world.23,24
At the time when the program was created, almost five million children under five years old were dying annually from diarrhea.25 Most pediatric departments were fully occupied, rehydrating children with intravenous solutions. Since the inception of ORT, the global estimates of mortality due to diarrhea have dramatically decreased from 4.6 million in 1980 to 1.8 million in 2000.26
Today, ORT remains a simple, cheap, and effective treatment for diarrheal illnesses. It has saved millions of lives and has been hailed as “potentially the most important medical advance of the 20th century.”27,28
End notes
- Olivier Fontaine and Charlotte Newton. “A revolution in the management of diarrhoea.” Bulletin of the World Health Organization 79, no. 5 (2001): 471-2.
- Dilip Mahalanabis et al. “Oral fluid therapy of cholera among Bangladesh refugees.” The Johns Hopkins Medical Journal 132 (1973): 197-205.
- Fontaine and Newton, “A revolution in the management of diarrhoea.”
- Dilip Mahalanabis. “Oral Rehydration Therapy, a Simple Solution: History and Global Application.” Science and Culture 80 (2014): 154-6.
- RB Fisher and DS Parsons. “Glucose movements across the wall of the rat small intestine.” The Journal of Physiology 119 (1953): 210-223.
- N Hirschhorn et al. “Decrease in net stool output in cholera during intestinal perfusion with glucose containing solutions.” New England Journal of Medicine 279 (1968): 176-80.
- NF Pierce et al. “Oral replacement of water and electrolyte losses in cholera.” Indian Journal of Medical Research 57 (1968): 848-55.
- Fontaine and Newton, “A revolution in the management of diarrhoea.”
- Dhiman Barua. “Application of science in practice by the World Health Organization in diarrhoeal diseases control.” Journal of Diarrhoeal Diseases Research 11 (1993): 193-6.
- Mahalanabis et al, “Oral fluid therapy of cholera among Bangladesh refugees.”
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Fontaine and Newton, “A revolution in the management of diarrhoea.”
- Mahalanabis, “Oral Rehydration Therapy, a Simple Solution,” 156.
- Mahalanabis et al, “Oral fluid therapy of cholera among Bangladesh refugees.”
- Fontaine and Newton, “A revolution in the management of diarrhoea.”
- Ibid.
- Ibid.
- Yancey, Diane. “An Easily Treatable Disease.” In: Cholera (Detroit: Gale Cengage, 2013), 63-70.
- Fontaine and Newton, “A revolution in the management of diarrhoea.”
- Mahalanabis, “Oral Rehydration Therapy, a Simple Solution,” 156-7.
- AR Samadi et al. “Replacement of intravenous therapy by oral rehydration solution in a large treatment centre for diarrhoea with dehydration.” Bulletin of the World Health Organization 61 (1983): 471-6.
- Mahalanabis et al, “Oral fluid therapy of cholera among Bangladesh refugees.”
- “Model List of Essential Medicines.” World Health Organization. https://list.essentialmeds.org/. Accessed September 1, 2021.
- Mathuram Santosham et al. “Progress and barriers for the control of diarrhoeal disease.” Lancet 376, no. 9734 (2010): 63-70.
MARIAM ABDULGHANI is a family medicine physician who resides and practices in southeastern Michigan. When she is not in the clinic, you can find her exploring new cafes, reading non-fiction books, and spending time with her family and friends.
Highlighted in Frontispiece Volume 15, Issue 3 – Summer 2023

Leave a Reply