Enrique Chaves-Carballo
Overland Park, Kansas
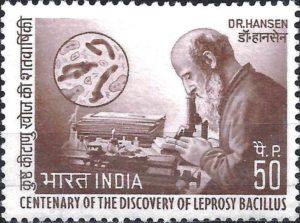 |
| Fig 1. Indian 50 paisa stamp shows Armauer Hansen at work in his laboratory. Via Wikimedia. Copyright Post of India, licensed under the Government Open Data License. |
The history of leprosy goes back to antiquity and is replete with unscientific prejudices, including the belief that the disease was highly contagious. Therefore, lepers were ostracized from society. It was not until the nineteenth century that Armauer Hansen (1841–1912), a Norwegian physician versed in histopathology, published in 1874 his findings establishing an infectious nature of leprosy. He found “in every leprous tubercle…small staff-like bodies, much resembling bacteria, lying within the cells.”1 Hansen, however, was unable to fulfill Koch’s postulates, which required isolation, cultivation of the organism, and then reproducing the disease in another animal species.
The offending organism, Mycobacterium leprae, resembles the tuberculosis bacterium in that it stains PAS positive and is acid-fast. However, it is fastidious and unable to grow in artificial media, and it only grows in a few selected animals such as mice and armadillos. A curious characteristic of M. leprae is its preference to attack the peripheral nerves and colder tissues such as the nose and fingers, causing disfiguring swelling and later necrosis. Characteristic findings in advanced cases are main en griffe (claw hand), missing digits, prominent superficial nerves, and perforating ulcers.2 The tubercular type presents with leontiasis (coarsening of the facial features) and satyriasis (compulsive sexual behavior). According to Darling, death occurs not so much from “leprotic toxemia” as from necrosis, ulceration, and secondary and terminal infections.3
The government of Panama required by law the segregation of lepers but was unable to enforce it because of a lack of funds. According to William Gorgas, Chief Sanitary Officer of the Canal Zone, an offer was made for the Americans to take care of these lepers at a rate of seventy-five cents per day per capita.4 Gorgas described in more detail the arrangement:
We established a colony [in 1907] on a beautifully located peninsula running out into the bay of Panama, and almost as much isolated as if it were on an island. Here they could have their gardens, chickens, and fruit-trees, etc. The location is naturally one of the prettiest on the bay.
We now have there some fifty lepers, who are living contented and happy. We have a white male trained nurse in general charge; a white female trained nurse in charge of the women, and some four or five other employees. We have a teacher for the children, and the lepers are always employed for any work of which they are capable, and are paid for this work so as to encourage them to seek it.
Dr. Henry R. Carter devoted a great deal of time and attention to the establishment of this colony, and it was due to his painstaking personal care that the matter turned out so successfully.4
 |
| Fig 2. Renovated mess hall building for lepers at Palo Seco. National Archives.
|
The site was originally a 500-acre fruit farm, located next to the Pacific Ocean on the west coast of the canal entrance and situated about six miles from Panama City. The first buildings were one-story frame structures in use until 1927, when two new modern buildings were erected of concrete and wood and each two stories high.5 One was for a dispensary, infirmary, offices, and storeroom; the other contained the kitchen, mess-hall (with seating capacity for 120), laundry, cistern, and refrigerating machinery. The superintendent made a definite effort to promote hygienic, dietetic, and social standards. Sample menus included cereal, cheese or eggs, butter, bread, and coffee each morning; salad or soup, meat, potatoes, rice, vegetable, butter, and milk at noon; and meat, rice, potatoes, vegetable, butter, bread, and tea or coffee for the evening meal. Social activities to keep residents “happy” included movies two or three times weekly, phonographs, a pool, fishing, swimming, and other amusements. A monthly allowance of $1.50 per month allowed each resident to purchase items at the colony storeroom such as clothes, tobacco, and toiletries.
Palo Seco was renovated twice: in 1938 and 1945. The latter consisted of nine new buildings housing apartments for individuals as well as for married residents, two churches, a kitchen, and two dining rooms (one for residents and one for employees). Nearby was an administrative office, a dental clinic, a commissary and warehouse, a sick ward, and a clinic and treatment room. The laundry, run by residents, could handle 200 pounds of clothes daily. One of the most important components was the recreation building where parties and dances were held, there were facilities for playing pool, and musical and folkloric groups from Panama came to celebrate Christmas.5
Detailed statistics showed that a total of 320 people were isolated at Palo Seco during the thirty-year period 1904–1933. Of these, 142 died, eighteen absconded, and eighteen were repatriated. The average age at onset was thirty-one years and average age at death was forty. The more common complications were anemia, nephritis, tuberculosis, and syphilis. Nine patients required amputation for extensive leprous tissue damage.5 Compared to the United States, the incidence of leprosy in Panama was about 100 times higher.
The 1977 Carter-Torrijos treaties stipulated that all territories and buildings in the Canal Zone should be transferred to Panama. Palo Seco was no exception. Since few lepromatous patients remained, it was converted into a long-term facility mainly for palliative care of the elderly and handicapped children by the Ministry of Public Health of Panama.6
Among the many remedies applied to leprous patients in the past were: potassium iodide, arsenic, antimony, copper, sera, vaccines, and aniline dyes. Other failed treatments include thymol, strychnine, baths of various kinds, X-rays, radium, and electrical currents.7 The first effective treatment against leprosy was chaulmoogra oil, which had been used in Asia for hundreds of years before it was introduced to Western medicine in the nineteenth century by Frederick John Mouat, a British physician, in 1854.8 Mouat entered the Indian Medical Service a year after obtaining his medical degree from Edinburgh and remained there for thirty years. He became a professor at the Bengal Medical College, and it was during this time that he became acquainted with chaulmoogra oil. In his paper, he was apologetic for not having more proof of its efficacy:
It is with considerable reluctance that I venture to submit for consideration of the profession in India, a few remarks upon the Cahulmoogra, as the opportunities which I have hitherto had of employing are too few and restricted to enable me to recommend it with the confidence that I could wish. Its success was, however, so remarkable and indisputable in one well-marked case of the worst form of leprosy, that I venture to hope an external application of it to that most loathsome and intractable of diseases, may prove so successful, as to secure the general introduction of the remedy.8
Chaulmoogra oil was initially administered topically with only limited success. Oral administration was poorly tolerated because of nausea and stomach distress. Finally, parenteral administration was tried but the injections were painful and resulted in abscesses even though therapeutic results were better. The oil was used sporadically at Palo Seco beginning in 1908, until patients were recruited for treatment with intramuscular injections in 1921. By 1930, a total of sixty-five patients received the injections. Side effects were mainly soreness and induration at the site of injection. Twenty of thirty-nine patients who received injections showed various degrees of improvement. The authors concluded that the results were “very satisfactory, and although it is yet too early to make a definite prognosis as to the outcome and results, still it can be safely said that the intramuscular injections of the ethyl esters of the chaulmoogra oil acids is superior to all other remedies in the treatment of leprosy.”9
Chaulmoogra oil was eventually replaced with more effective antimicrobials dapsone (4:4-diamino-diphenyl-sulfone) and other sulfone derivatives in the 1940s. Chaulmoogra oil therapy was officially abandoned at the Public Health Service leprosy hospital at Carville in 1947. The efficacy of sulfones allowed for the medical discharge of leprosy patients to outpatient treatment. By the 1950s, chaulmoogra oil had become just “a colorful relic of pharmacy’s past.”7
The estimated number of leprosy cases worldwide decreased from about ten million in the 1970s to 200,000 at present, mainly distributed in tropical and subtropical regions of Asia, Africa, and South America. The World Heath Organization has declared leprosy a neglected tropical disease and has launched an ambitious plan to eradicate it by 2035 with multiple drug treatment (MDT: rifampicin, dapsone and clofazimine).10
If successful, leprosy may become, as chaulmoogra oil itself, a relic of the past.
References
- Tan SY and Graham C. Armauer Hansen (1841-1912): discoverer of the cause of leprosy. Singapore Med J 2008; 49:520-521.
- James WC. A case of anesthetic leprosy. Proceedings of the Medical Association of the Canal Zone (Proceedings) 1908; I:166-171.
- Darling ST. Observations on the factors concerned in the cultivation of leprosy bacilli and on the development of a therapy. Proceedings 1911; IV (Part 1):122-132.
- Gorgas WC. Sanitation in Panama. New York: D. Appleton and Company, 1911.
- Horwitz E, Anderson HH. Leprosy in Panama. First thirty years of segregation. Am J Trop Med & Hyg 1936; s1-16:358-369.
- Personal communication. Ministerio de Salud Pública de Panamá (Ministry of Public Health of Panama). https://minsa.gob.pa.
- Parascandola J. Chaulmoogra oil and the treatment of leprosy. Pharm Hist 2003; 45(2):47-57 (Pub 2003048). https://lhncbc.nlm.nih.gov/LHC-publications/pubs/ChaulmoograOilandtheTreatmentofLeprosy.html.
- Mouat FJ. Notes on native remedies. No. 1. The chaulmoogra. Indian Ann Med Sci 1854; 1:646-652.
- Horwitz P. A preliminary analysis of the treatment of lepers at Palo Seco with the ethyl esters of the fatty acids of chaulmoogra oil. Proceedings 1921; XIV:55-59.
- WHO International Fact Sheets. Leprosy. January 11, 2022. https://who.int/news-room/fact-sheets/detail/leprosy.
ENRIQUE CHAVES-CARBALLO is a retired physician living in Overland Park, Kansas.
Fall 2022 | Sections | Infectious Diseases

Leave a Reply