Amogh BJ
Trivandrum, Kerala, India
Nanditha Venkatesan
Raipur, Chhattisgarh, India
For centuries rheumatic fever (RF) and its sequelae scourged the lives of millions of people. Despite a substantial decline in deaths from the disease, rheumatic heart disease remains a problem, especially in areas of poverty. Over the past few centuries, a growing understanding of its causation and pathogenic mechanisms has benefitted both the treatment and prevention of the disease.

Early perceptions
Although febrile arthritis was known even in the time of Hippocrates, it was the French physician Guillaume de Baillou who first used the word “rheumatism” to describe an acute febrile polyarthritis distinct from gout.1 In 1685 Thomas Sydenham noted that the disease “chiefly attacks the young and vigorous.” He provided a vivid description of the clinical manifestations of acute RF and the progression of the disease:
“The sad list of symptoms begins with chills and shivers; these are followed immediately by heat, disquietude, thirst, and the other concomitant of fever. One or two days after this (sometimes sooner) the patient is attacked by severe pains in the joints. . . . This pain changes its place from time to time, takes the joints in turn, and affects the one that it attacks last with redeems and swelling.”
Sydenham rightly described sore throat as a harbinger of acute RF in the young. He pointed out that “blood of rheumatism is as like the blood of pleurisy, as one egg is like another,” referring to the inflammatory nature of both diseases. Hence, the treatment closely followed the view on inflammation propounded by Galen, namely that the “percolation of blood caused an imbalance in humors.”2 Sydenham advocated bloodletting and dilution remedies:3 “Water of water lillies, Purslain water, Lettuce water, Syrup of lemons, Syrup of violets; mix and make a julep to be taken ad libitum.” Sir Richard Blackmore in his treatise Gout, a Rheumatism, and the King’s Evil recorded the popular use of refrigerating remedies to bring down the fever.4 Of these the most effective was willow bark, which had been used as early as 400 BC to reduce pain and fever. Other remedies were a wide range of volatile salts such as Spirit of Hartshorn, Dr. Goddard’s Drops (a mixture of ivory, dried viper, a horn of a deer, and human skulls of those that died a violent or traumatic death such as hanging), and Sal Volatile Oleofum (alcohol and ammonium chloride) to awaken those who had fainted or were semi-conscious. Leeches were recommended for obstinate symptoms.
Rheumatic fever licks the joints but bites the heart (Lasegue)
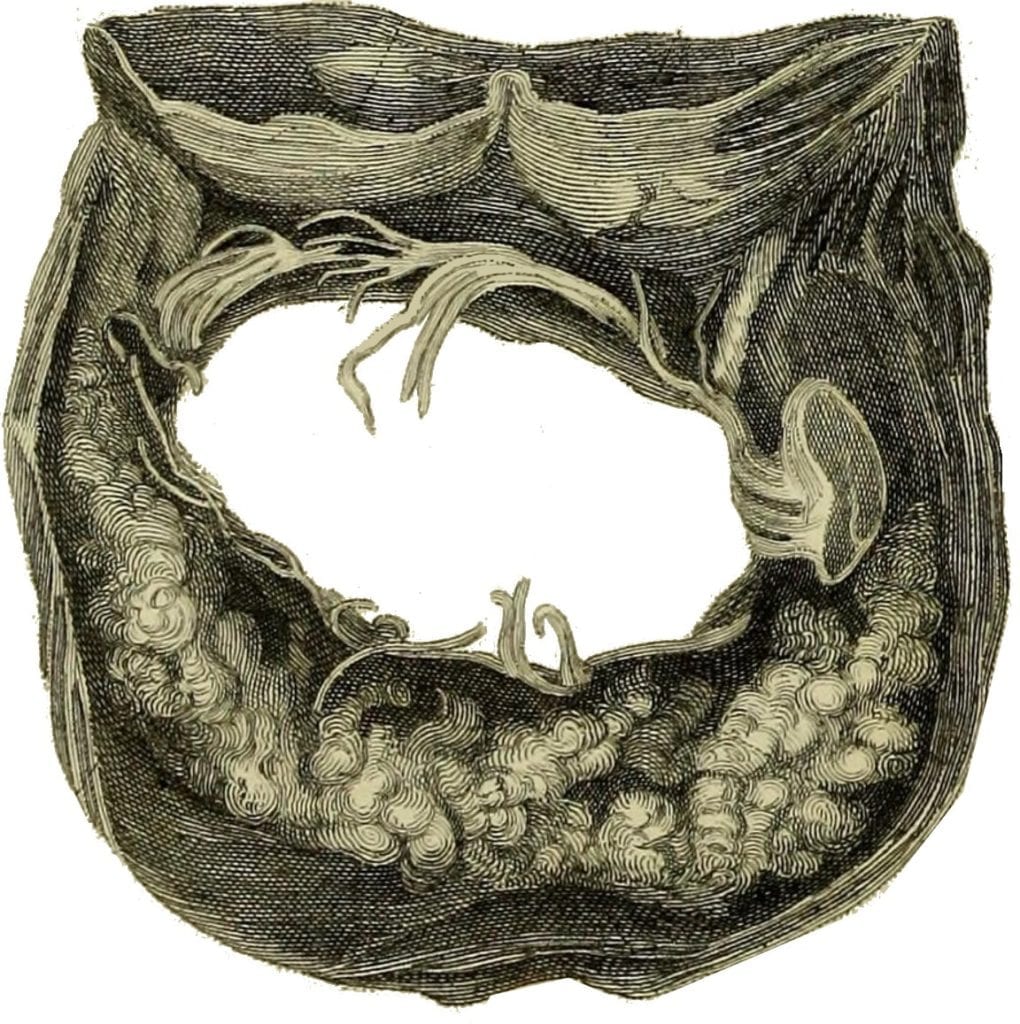
Pathologist Mathew Baillie, in his book The morbid anatomy of the most important parts of the human body, noted that “the valvular apparatus between the auricles and ventricles, is liable to the formation of bony and earthy matter” and are “occasionally thickened, having lost all its transparency.”5
He recorded the possible association between cardiac enlargement and rheumatism as described by his colleague and teacher, David Pitcairn. William Charles Wells in 1812 suggested an association between RF and heart disease based on the symptoms he observed.6 He did not propose any theory of causation. After the invention of the stethoscope by Rene Laennec, murmurs resulting from valvular diseases of the heart were recognized and James Hope described auscultatory findings in patients with RF.7 The stethoscope facilitated epidemiological studies that identified heart disease. Based on auscultatory findings, Jean-Baptise Bouillard, a noted physician at the Sick Children’s Hospital in Paris, was able to pick up asymptomatic heart disease and estimated that nearly half the people with acute rheumatism suffered from pericarditis, endocarditis, or both. In the book Nouvelles Recherches Sur Le Rhumatisme,8 he stated:
“In the great majority of cases of acute generalized febrile articular rheumatism, there exists a variable degree of rheumatism of the fibrous tissue of the heart. This coincidence is the rule, and the non-coincidence the exception.”
The complete spectrum of RF was soon recognized, and this had a major impact on the management of the disease. The presumption that scarring in the heart primarily depended on the severity and duration of inflammation led to the first rational approach to the treatment of rheumatic carditis, advanced by Sibson, who highlighted rest as the most important component.9 Surgical management of chronic valvular disease started much later, in 1923, with American surgeons Eliot Carr Cutler and Samuel Levine performing the first closed trans-ventricular mitral commissurotomy in a twelve-year-old patient with mitral stenosis.10
The use of salicylates
The bark and leaves of the willow tree had been used to treat febrile illnesses since the time of Hippocrates. In 1763 the Reverend Edmund Stone, an English natural philosopher, reported willow bark as the first specific treatment for RF.11,12 Following this report to the Royal Society, many physicians began to prescribe Peruvian bark, cinchona, and willow bark. A case report in 1813 claimed that these remedies allowed a patient to go “horseback riding on the 6th day of disease.”13 In 1826 Henri Leroux, a French chemist, isolated salicin from the willow bark.14 Nearly five decades later, Thomas John McLagan in The Lancet announced that “we have in salicin a valuable remedy in the treatment of acute rheumatism.”15

The infective origin of rheumatic fever
The Austrian surgeon Theodor Billroth in 1874 described “small organisms as found in either isolated or arranged in pairs, sometimes in chains” in skin and soft tissue infections. He named the organisms “streptococci,”16 a name taken from the Greek words streptos, meaning chain, and kokkos, meaning berry. In 1901 Poynton and Paine found streptococci in the synovial fluid of a young boy with acute RF.17 This led to the view that the manifestations of RF, including cardiac involvement, were due to direct bacterial invasion. Later the American microbiologist Rebecca C. Lancefield proposed a serological classification of beta-hemolytic streptococci based on the carbohydrate antigen on the bacterial cell wall, followed in 1921 by the American physician Alvin F. Coburn and the Irish physician WRF Collis establishing Group A Streptococci, or Streptococcus pyogenes, as the causative agent of RF.18–20
The following year, an autoimmune theory for joint and heart involvement was proposed. The theory derived support from the observation that antistreptolysin (ASO) titers were elevated in patients with pharyngitis and associated with later complications of RF.21
The miracle of antibiotics
The discovery of the cause of RF changed the way the disease was managed. After 1935 sulfa drugs such as sulfanilamide, sulfapyridine, and sulfamerazine were put into use along with conventional medications.22 A landmark advance was made in 1942 when penicillin saved the life of thirty-three-year-old Ann Miller who was dying from life-threatening streptococcal septicemia after childbirth and had not benefitted from treatments with sulfa drugs and blood transfusions.23 The beneficiary role of antibiotics in the treatment of RF has stood the test of time.
In a cohort study involving the long follow-up of 1,000 young people with RF, American physicians Edward F. Bland and Duckett Jones found an association between the number of recurrent attacks of RF and mortality.24 Their findings indicated that preventing recurrent attacks could change the outcome of the disease. Secondary prophylactic treatment with sulfa drugs and penicillin was hence advocated.25 Another advance in the management of RF was the use of corticosteroids, after Philip Showalter Hench and his team in 1949 reported their advantage for the treatment of inflammatory conditions.26
The way forward
Thanks to advances in the understanding of pathogenesis and treatment of RF, as well as improvements in standards of living, the burden of RF and its sequelae have declined significantly. In many developed nations what once was the second-most common cause of death has now virtually disappeared.27 This is gratifying since RF affects predominantly the young, causing a loss of the most productive years of life and perpetuating poverty.
A better understanding of the immunogenicity of streptococci and development of a vaccine is still needed. Difficulties in developing a vaccine include the wide variety of strains of S. pyogenes present in the environment and the efforts needed for appropriate trials for safety and efficacy of the vaccine.
Much of our understanding of the biology of diseases has been made by physician-scientists, a vanishing model of practice.28 A physician-scientist is in a unique position to identify problems at the bedside, take them to the bench to find solutions, and return to the bedside with benefits for patients. We hope more students and young doctors will be inspired to take up these challenges as the next generation of physician-scientists.
References
- Kaiser H, Keitel W. Guillaume de Baillou (1538–1616) – Vater des „Rheumatismus“? Zeitschrift für Rheumatologie. 2006;65(8):743-746. doi:10.1007/s00393-006-0079-7
- Granger DN, Senchenkova E. Inflammation and the Microcirculation, Chapter 2: Historical Perspectives. Morgan & Claypool Life Sciences; 2010. Accessed April 12, 2020. https://www.ncbi.nlm.nih.gov/books/NBK53379/
- Sydenham T, Greenhill WA, Latham RG, et al. The works of Thomas Sydenham, M.D. Printed for the Sydenham Society; 1848.
- Blackmore R. Discourses on the Gout, a Rheumatism, and the King’s Evil: Containing an Explication of the Nature, Causes, and Different Species of Those Diseases, and the Method of Curing Them. J. Pemberton; 1726.
- Baillie M 1761-1823 (viaf)47543063. The Morbid Anatomy of Some of the Most Important Parts of the Human Body By Matthew Baillie,. The second edition, corrected and considerably enlarged. London : printed for J. Johnson; and G. Nicol; 1797. http://lib.ugent.be/catalog/rug01:001096022
- KEIL H. DR. WILLIAM CHARLES WELLS AND HIS CONTRIBUTION TO THE STUDY OF RHEUMATIC FEVER. Bulletin of the Institute of the History of Medicine. 1936;4(10):789-816.
- Rosenberg CE, Golden JL. Framing Disease: Studies in Cultural History. Rutgers University Press; 1992.
- Rolleston JD. Jean Baptiste Bouillaud (1796-1881). A Pioneer in Cardiology and Neurology. Proc R Soc Med. 1931;24(9):1253-1262.
- Reynolds SJR. A System of Medicine, Ed. by J.R. Reynolds. Macmillan and Company; 1877.
- Cohn LH. The first successful surgical treatment of mitral stenosis: the 70th anniversary of Elliot Cutler’s mitral commissurotomy. The Annals of thoracic surgery. 1993;56(5):1187-1190.
- Stone E. XXXII. An account of the success of the bark of the willow in the cure of agues. In a letter to the Right Honourable George Earl of Macclesfield, President of R. S. from the Rev. Mr. Edward Stone, of Chipping-Norton in Oxfordshire. Philosophical Transactions of the Royal Society of London. 1763;53:195-200. doi:10.1098/rstl.1763.0033
- Hedner T, Everts B. The early clinical history of salicylates in rheumatology and pain. Clin Rheumatol. 1998;17(1):17-25. doi:10.1007/BF01450953
- Haygarth J. A Clinical History of the Acute Rheumatism, Or Rheumatick Fever …: A Clinical History of the Nodosity of the Joints … Richard Cruttwell; 1813. https://books.google.co.in/books?id=qi3tuQEACAAJ
- Tsoucalas G, Karamanou M, Androutsos G. Travelling through Time with Aspirin, a Healing Companion. Eur J Inflamm. 2011;9(1):13-16. doi:10.1177/1721727X1100900102
- Maclagan T. The treatment of acute rheumatism by salicin. The Lancet. 1876;107(2741):383-384.
- Etymologia: Streptococcus. Emerg Infect Dis. 2016;22(11):1977-1977. doi:10.3201/eid2211.ET2211
- Poynton FJ, Paine A. A further Contribution to the Study of Rheumatism. The Experimental Production of Appendicitis by the Intravenous Inoculation of the Diplococcus. Proc R Soc Med. 1912;5(Pathol Sect):18-29.
- Carroll KC. Biographical Feature: Rebecca Lancefield, Ph.D. Munson E, ed. J Clin Microbiol. 2019;57(8):e00728-19, /jcm/57/8/JCM.00728-19.atom. doi:10.1128/JCM.00728-19
- Collis W. Acute Rheumatism and Haemolytic Streptococci. Lancet. Published online 1931:1341-1345.
- Coburn AF. The Factor of Infection in the Rheumatic State. Williams & Wilkins; 1931.
- Todd E. Antihæmolysis Titres in Hæmolytic Streptococcal Infections and their Significance in Rheumatic Fever. British journal of experimental pathology. 1932;13(3):248.
- Thomson WH. A Treatise on Clinical Medicine (1914). Books LLC; 2009. https://books.google.co.in/books?id=XN5dRAAACAAJ
- Curtis J. Fulton, penicillin and chance. Yale School of Medicine. Accessed April 12, 2020. https://medicine.yale.edu/ysm/news/yale-medicine-magazine/fulton-penicillin-and-chance/
- Bland EF, Jones D. Rheumatic fever and rheumatic heart disease: a twenty year report on 1000 patients followed since childhood. Circulation. 1951;4(6):836-843.
- Proceedings of Conference on Rheumatic Fever: Washington, D.C., October 5-7, 1943. U.S. Government Printing Office; 1945.
- Hench PS. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone: Compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis; preliminary report. In: Vol 24. ; 1949:181-197.
- Bland EF. Rheumatic fever: the way it was. Circulation. 1987;76(6):1190-1195.
- Schafer AI. History of the physician as a scientist. The Vanishing Physician-Scientist. Published online 2009:17-38
AMOGH BJ, MBBS, is a house surgeon and student research coordinator at Government Medical College Thiruvananthapuram. His areas of interest include medical education, epidemiology, and immunology. In his spare time he enjoys painting, performing stage magic, and volunteering as a science teacher for underprivileged children.
NANDITHA VENKATESAN, MBBS, is a final year medical student at All India Institute of Medical Sciences, Raipur. She has a keen interest in emergency medicine and global health. She enjoys reading and writing, and is a contributing member of a nonprofit research group called Asar that focuses on data-led local policymaking in India.
Acknowledgements
The authors would like to thank Dr. Chandrasekharan C Kartha (Chairman of the Research Advisory Committee of ICMR Multi-Disciplinary Research Unit at Government Medical College, Trivandrum) for reviewing the article.
Highlighted in Frontispiece Volume 12, Issue 4 – Fall 2020 & Volume 15, Issue 1 – Winter 2023

Leave a Reply