Mariel Tishma
Chicago, Illinois, United States
Maybe your chest hurts from coughing, or maybe your muscles ache. Maybe you feel sluggish and anxious, worn out, and not sure why. There is a treatment, some say, for all of that and more.
If it is done right, you only walk away with bruises—perfect circles in shades of purple-brown running up and down the body, especially the back, neck, and shoulders. The bruises are signs that the treatment is working, pulling out the fluids that were causing the problem.
Would you take it? Even if a doctor can offer you no proof that it works?
In the case of cupping, many do.
Cupping, like other forms of alternative medicine, is a highly divisive treatment. Some say that it, like acupuncture, is an unexplored miracle cure or at least an underutilized tool. On the other side, voices declare cupping a waste of time and money—nothing more than quackery.
But the truth is fuzzy. There is little conclusive, high quality evidence that cupping works.1 But there is a plethora of anecdotes and patient experiences for a technique with a long history.
Cupping, or the use of a vessel to apply suction to the skin, is an ancient practice that comes in various forms. In simple dry cupping, suction is used to draw the skin inside the vessel without any additions. Wet cupping is the application of a suction vessel after the skin has been cut in order to draw out blood. An ancient variety still used today is fire cupping—in which a vacuum is created using heat—and a popular modern technique is a hand-powered vacuum pump. These are the main varieties of the practice, but there are many others. For example flash cupping consists of quickly applying, removing, and re-applying the cupping vessel. In moving cupping, oil is applied to the skin and the cup slid across the body after suction.
Cupping can be combined with the burning of herbs over the application site or the cups can be filled with water, applied over acupuncture needles, or combined with lasers and electricity.2
When compared with techniques such as acupuncture, the variety and combination of practices in cupping is rather surprising, and perhaps makes it more difficult to study. Differences can be as essential as the material of the cup or suction vessel. Most common today are glass and plastic, but vessels have also been made of bamboo, wood, rubber, and, in the most ancient practices, animal horn.3, 4, 5
Cupping is mentioned in Eber’s papyrus, and Hippocrates gathered descriptions of the practice.6 It is also mentioned as part of the diatritus, a system of medical treatment created by the Greek Thessalus.7
Cupping is a popular treatment in Muslim societies as part of the system of prophetic medicine, which contains treatments directly recommended by the prophet.8 In Arabic, cupping is referred to as hijamah. In this tradition hijamah is not only practiced as treatment of disease—as is most common in other cultures—but it is commonly practiced as a form of preventive medicine as well.9 Hijamah “returns an ill state to its original state”10 by removing bad blood and other fluids, and so almost always involves bleeding.11
Cupping’s history in East Asian cultures, moving qi or energy throughout the body similarly to acupuncture, is more well known.12 Cupping is an integral part of many East Asian medical systems. Ge Hong, a Taoist alchemist and herbalist from China, wrote on cupping around 300 AD,13 and it has remained popular. Within Traditional Chinese Medicine, the patient is assessed and then cups are applied at specific points along energy channels called meridians in order to stimulate specific parts of the body. Dry cupping is “practiced more commonly in the Far East” compared to the Middle Eastern tradition.14
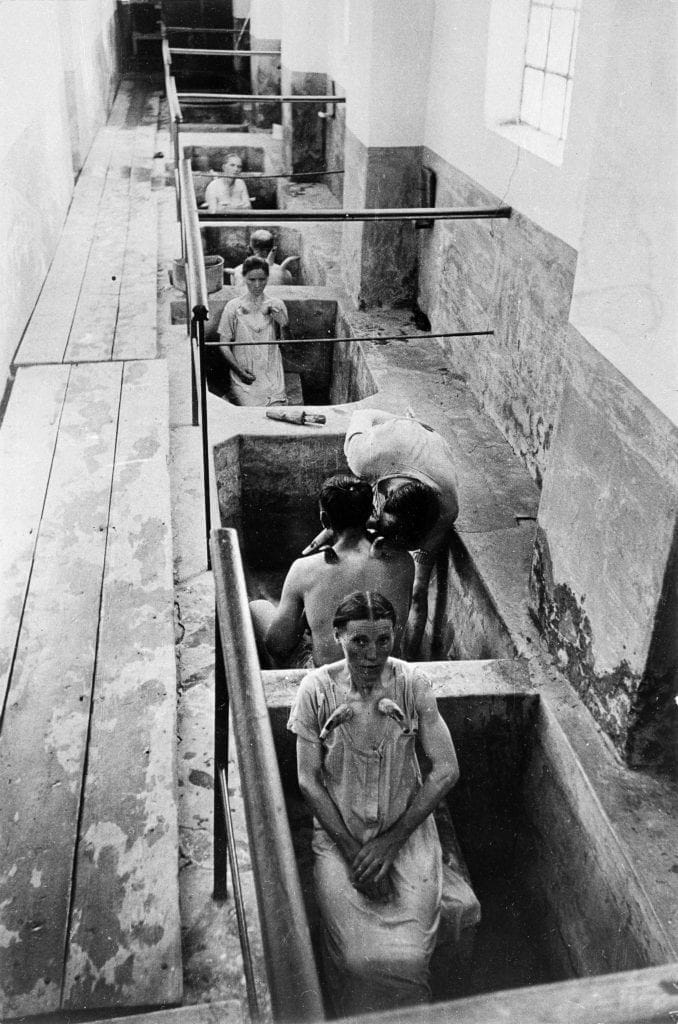
Cupping has a European history as well, rising and falling in waves of popularity over time.15 Cupping experienced a surge in the fourteenth century and during this time it was used commonly for gout.16 It waned in popularity in the seventeenth century, but certainly still remained, and stories from that time exist today. One from 1854 tells of a doctor using dry cupping to relieve pain and facilitate delivery during a difficult labor.17 Cupping was popular in France as late as the 1920s where it was “the universal panacea for aches and pains, for stitch in the side or shortness of breath, and so on.”18 Though no longer part of the official medical system in the modern era, cupping is still practiced in parts of Europe and elsewhere in the world. One physician in 1981 reported that two young patients from Russian families had come in with respiratory problems and the indicative bruising of cupping. Both families had attempted to treat the respiratory issues with cupping, a common practice in Russian culture.19
Cupping has gained attention outside of these specific regions and cultures through literature and celebrity. Essayist George Orwell covered his experience receiving cupping as a treatment for pneumonia in a French hospital in 1929. He writes that he was initially dry cupped using fire as a suction method, then bled using wet cupping. He also describes cupping as “a treatment which you can read about in old medical text-books but which till then I had vaguely thought of as one of those things they do to horses,” reflecting cupping’s waning popularity in his time.20
American cupping practitioners declared 2005 the “cupping therapy year.”21 Perhaps not coincidentally, in the years that followed, actresses such as Gwyneth Paltrow and Jennifer Anniston sported the trademark bruises of cupping to premiers and events, putting the practice into the public eye.22
During the 2016 Olympic Games, swimmer Michael Phelps became a focal point thanks to cupping bruises. He claimed the treatment improved his performance. A cascade of other athletes followed suit, and soon those outside of professional sports hoping to gain an edge were seeking out the treatment as well.23
For some, this is enough to continue receiving and recommending cupping. But finding scientific proof for the unconvinced, and to legitimate the practice for the medical profession, is not that simple.
Most of the research on cupping has been of low quality, whether due to lack of blinding, small sample size, or because of bias.24 Studies have focused primarily on pain relief,25, 26, 27, 28, headache,29 and a few other conditions such as herpes zoster.30 Systematic reviews of pain-based studies most often conclude that there is some reason to believe cupping is good for pain relief, but that it is hard to determine if this is a placebo effect, the effect of relaxation in the moment, or a unique quality of cupping. The same holds true for reviews of the studies on other conditions.
Most studies, inconclusive as they are, focus on whether or not cupping techniques work. Few seem to be searching for what the technique actually does to improve health or relieve pain.
The proposed mechanism of how cupping is supposed to work is increasing the blood flow to affected areas, relaxing the muscles, and reducing overall inflammation.31, 32 Cupping is said to lift the skin and reduce muscle adhesions as well as stimulating the immune system.33 It may relieve pain by counter-irritation, as proposed for acupuncture. It is unclear how these benefits would help conditions such as asthma, but many say that if the practice works, it need not be researched further.
This does not make for a safe, medically approved practice. Because cupping does not have to break the skin, it is perceived as very low risk, perhaps even more so than acupuncture. But there are possible side effects, even for dry cupping, some of which may be serious.
In all fairness, the primary risks are minor, such as the signature circular bruises that helped spread cupping’s popularity. There have also been reports of cupping worsening some skin diseases.34 Also, cupping has been used to treat conditions in which it is not likely to work, such as a cold, that clear on their own anyway, giving a false impression of effectiveness.
On the more serious end, some recipients have been burned from inappropriate application of cups during fire cupping, and also received burn-like wounds from repeated treatments in the same location from reduced circulation and repeated bruising.35 These are more likely to occur during treatment from inexperienced or unregulated practioners. There is also a possibility of skin or wound infections being contracted in wet cupping if the tools and treatment area are not properly sanitized.36
Most distressing of all, some may seek cupping as a treatment for serious conditions such as cancer. This has already been the case for one Chinese celebrity who died in 2016 after choosing cupping and Traditional Chinese Medicine to treat leukemia.37 The use of alternative medicines over conventional ones for serious conditions remains an issue of note.
Perhaps the best way to prevent the misguided use of cupping would be to conduct rigorous studies of what the technique can and cannot do. While some will not be convinced, it may help deter others from putting themselves at risk by foregoing more appropriate treatment. As with other complementary and alternative medicines, some patients will seek out and receive these treatments regardless of proof of their effectiveness. However, if the practice is studied more thoroughly, its risks can be properly categorized, the practice better regulated, and its benefits explained—even if they amount only to relaxation. This will allow recipients to make better decisions about their health.
References
- “Cupping,” National Center for Complementary and Integrative Health, last modified November 09, 2018, accessed September 2019, https://nccih.nih.gov/health/cupping.
- Abdullah Mohammed Al-Bedah, Tamer Shaban Aboushanab, Meshari Saleh Alqaed, Naseem Akhtar Qureshi, Imen Suhaibani, Gazzaffi Ibrahim, and Mohammed Khalil, “Classification of Cupping Therapy: A Tool for Modernization and Standardization,” Journal of Complementary and Alternative Medical Research 1 no. 1 (2016): 1-10, accessed September 2019, DOI: 10.9734/JOCAMR/2016/27222.
- Ilkay Zihni Chirali, Traditional Chinese Medicine Cupping Therapy, 3rd, (Churchill Livingstone, 2014), 1.
- Hajar A Hajar Albinali, “Chairman’s Reflections : Blood-letting,” Heart Views 5 no. 2 (2004): accessed September 2019, http://www.heartviews.org/text.asp?2004/5/2/74/64567.
- Piyush Mehtaa and Vividha Dhapte, “Cupping therapy: A prudent remedy for a plethora of medical ailments,” Journal of Traditional and Complementary Medicine 5 no. 3 ( July 2015): 128, accessed September 2019, https://doi.org/10.1016/j.jtcme.2014.11.036.
- Ibid. 127.
- David Leith, “The “Diatritus” and Therapy in Graeco-Roman Medicine,” The Classical Quarterly, New Series, 58, No. 2 (December, 2008): 595, Accessed September 2019, https://www.jstor.org/stable/27564187.
- Mohamed K.M. Khalil, Sulaiman Al-Eidi, Meshary Al-Qaed, and Saud AlSanad, “Cupping therapy in Saudi Arabia: from control to integration,” Integrative medicine research 7 no. 3 (September, 2018): 215, Accessed September 2019, doi: 10.1016/j.imr.2018.05.002.
- Naseem Akhtar, “History of cupping (Hijama): a narrative review of literature,” Journal of Integrative Medicine vol. 15 no. 3 (May, 2017): 175, accessed September 2019, http://dx.doi.org/10.1016/S2095-4964(17)60339-X.
- Hajar A Hajar Albinali, “Chairman’s Reflections: Blood-letting,”
- Naseem Akhtar, “History of cupping (Hijama): a narrative review of literature,” 174.
- Natalie Köhle, “Cups, Needles, and Noxious Blood” in Control, ed. Jane Golley, Linda Jaivin, Luigi Tomba, (ANU Press, 2017), 179.
- Naseem Akhtar, “History of cupping (Hijama): a narrative review of literature,” 176.
- Tamer S. Aboushanab, Saud AlSanad, “Cupping Therapy: An Overview from a Modern Medicine Perspective,” Journal of Acupuncture and Meridian Studies 11 no. 3 (June, 2018): 84, Accessed September 2019, https://doi.org/10.1016/j.jams.2018.02.001.
- Ibid.
- J. Manson, “Dry Cupping in Labour,” Association Medical Journal, Vol. 2, No. 54(January, 1854): 36-37, Accessed September 2019, https://www.jstor.org/stable/25495255.
- Alfred S. Gubb, “Cupping, Dry And Wet,” Title of Journal The British Medical Journal, 1, No. 3250(April, 1923): 639, Accessed September 2019, https://www.jstor.org/stable/20423115.
- Dearlove, A. P. Verguei, N. Birkin, and P. Latham, “An Anachronistic Treatment For Asthma,” British Medical Journal (Clinical Research Edition), Vol. 283, No. 6307 (December, 1981): 1684-1685, Accessed September 2019, https://www.jstor.org/stable/29504720.
- George Orwell, “How the Poor Die” in Fifty Orwell Essays, ed. Colin Choat, (Project Gutenberg of Australia, 2003), http://gutenberg.net.au/ebooks03/0300011h.html#part39.
- Ilkay Zihni Chirali, Traditional Chinese Medicine Cupping Therapy, 3rd, (Churchill Livingstone, 2014), 7.
- Stephanie Chan, “Cupping: The Eastern Practice Embraced by Michael Phelps and Hollywood Types Explained,” The Hollywood Reporter, August 8, 2016, Accessed December 2019, https://www.hollywoodreporter.com/news/what-is-cupping-michael-phelps-918060.
- Giuseppe Musumeci, “Could Cupping Therapy Be Used to Improve Sports Performance?” Journal of Functional Morphology and Kinesiology 1 no. 4 (October 2016): 373, Accessed September 2019, https://doi.org/10.3390/jfmk1040373.
- Myeong Soo Lee, Jong-In Kim, Edzard Ernst, “Is Cupping an Effective Treatment? An Overview of Systematic Reviews,” Journal of Acupuncture and Meridian Studies 4 no. 1 (March, 2011): 2-3, Accessed September 2019, https://doi.org/10.1016/S2005-2901(11)60001-0.
- Seoyoun Kim, Sook-Hyun Lee, Me-Riong Kim, Eun-Jung Kim, Deok-Sang Hwang, Jinho Lee, Joon-Shik Shin, In-Hyuk Ha, and Yoon Jae Lee, “Is cupping therapy effective in patients with neck pain? A systematic review and meta-analysis,” BMJ Open vol 8. No. 11 (November, 2018): 1-13, Accessed September 2019, doi: 1136/bmjopen-2017-021070.
- Jong-In Kim, Tae-Hun Kim, Myeong Soo Lee, Jung Won Kang, Kun Hyung Kim, Jun-Yong Choi1, Kyung-Won Kang, Ae-Ran Kim, Mi-Suk Shin, So-Young Jung, and Sun-mi Choi, “Evaluation of wet-cupping therapy for persistent non-specific low back pain: a randomised, waiting-list controlled, open-label, parallel-group pilot trial,” Trials vol 12 (2011), Accessed September 2019, doi:10.1186/1745-6215-12-146.
- Asim Ali Khan, Umar Jahangir, and Shaista Urooj, “Management of knee osteoarthritis with cupping therapy,” Journal of advanced pharmaceutical technology & research 4 no. 4 (Oct-Dec, 2013): 217-223 Accessed September 2019, doi: 10.4103/2231-4040.121417.
- Huijuan Cao, Xun Li, Xue Yan, Nissi S. Wang, Alan Bensoussan, Jianping Liu, “Cupping therapy for acute and chronic pain management: a systematic review of randomized clinical trials,” Journal of Traditional Chinese Medical Sciences 1 no. 1 (December 2014): 49-61 Accessed September 2019, http://dx.doi.org/10.1016/j.jtcms.2014.11.003.
- Alireza Ahmadi, David C. Schwebel, and Mansour Rezaei, “The Efficacy of Wet-Cupping in the Treatment of Tension and Migraine Headache,” The American Journal of Chinese Medicine, 36, No. 1 (2008): 37-44 Accessed September 2019, DOI: 10.1142/S0192415X08005564.
- Huijuan Cao, Chenjun Zhu, and Jianping Liu, “Wet cupping therapy for treatment of herpes zoster: a systematic review of randomized controlled trials,” Alternative Therapies in Health and Medicine 16 no. 6 (Nov-Dec 2010): 48-54, Accessed September 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3151529/.
- Piyush Mehtaa and Vividha Dhapte, “Cupping therapy: A prudent remedy for a plethora of medical ailments,” 128-129.
- Chen, B., M.-Y. Li, P.-D. Liu, Y. Guo, and Z.-L. Chen, “Alternative medicine: an update on cupping therapy,” QJM: An International Journal of Medicine 108 no. 7 (November 2014): 524, Accessed September 2019, https://doi.org/10.1093/qjmed/hcu227.
- Laura Johannes, “Centuries-Old Art of Cupping may Bring Some Pain Relief,” Health & Wellness, The Wall Street Journal, November 13, 2012.
- Lee-Mei Chi, Li-Mei Lin, Chien-Lin Chen, Shu-Fang Wang, Hui-Ling Lai, and Tai-Chu Peng, “The Effectiveness of Cupping Therapy on Relieving Chronic Neck and Shoulder Pain: A Randomized Controlled Trial,” Evidence-Based Complementary and Alternative Medicine, 2016, (2016), Accessed September 2019, https://doi.org/10.1155/2016/7358918.
- Abdullah Mohammad Al-Bedah, Tamer Shaban, Amen Suhaibani, Ibrahim Gazzaffi, Mohammed Khalil, and Naseem Akhtar Qureshi, “Safety of Cupping Therapy in Studies Conducted in Twenty One Century: A Review of Literature,” British Journal of Medicine & Medical Research 15 no. 8 (May, 2016): 9, Accessed September 2019, DOI: 10.9734/BJMMR/2016/26285.
- Chen, B., M.-Y. Li, P.-D. Liu, Y. Guo, and Z.-L. Chen, “Alternative medicine: an update on cupping therapy,” QJM: An International Journal of Medicine 108 no. 7 (November 2014): 5324, Accessed September 2019, https://doi.org/10.1093/qjmed/hcu227.
- “Cupping,” National Center for Complementary and Integrative Health.
- Natalie Köhle, “Cups, Needles, and Noxious Blood” in Control, ed. Jane Golley, Linda Jaivin, Luigi Tomba, (ANU Press, 2017), 178, https://www.jstor.org/stable/j.ctt1sq5tvf.19.
Bibliography
- Aboushanab, Tamer S, Saud AlSanad. “Cupping Therapy: An Overview from a Modern Medicine Perspective.” Journal of Acupuncture and Meridian Studies vol. 11 no. 3 (June, 2018): 83-87. https://doi.org/10.1016/j.jams.2018.02.001.
- Ahmadi, Alireza, David C. Schwebel, and Mansour Rezaei. “The Efficacy of Wet-Cupping in the Treatment of Tension and Migraine Headache.” The American Journal of Chinese Medicine, Vol. 36, No. 1 (2008): 37–44. DOI: 10.1142/S0192415X08005564.
- Al-Bedah, Abdullah Mohammed, Tamer Shaban Aboushanab, Meshari Saleh Alqaed, Naseem Akhtar Qureshi, Imen Suhaibani, Gazzaffi Ibrahim, and Mohammed Khalil. “Classification of Cupping Therapy: A Tool for Modernization and Standardization.” Journal of Complementary and Alternative Medical Research vol. 1 no. 1 (2016): 1-10. DOI: 10.9734/JOCAMR/2016/27222.
- Albinali, Hajar A Hajar. “Chairman’s Reflections : Blood-letting.” Heart Views vol. 5 no. 2 (2004): 74-85. http://www.heartviews.org/text.asp?2004/5/2/74/64567.
- Ali Khan, Asim, Umar Jahangir, and Shaista Urooj. “Management of knee osteoarthritis with cupping therapy.” Journal of advanced pharmaceutical technology & research vol. 4 no. 4 (Oct-Dec, 2013): 217–223. doi: 10.4103/2231-4040.121417.
- B. Chen, M.-Y. Li, P.-D. Liu, Y. Guo, and Z.-L. Chen, “Alternative medicine: an update on cupping therapy.” QJM: An International Journal of Medicine vol. 108 no. 7 (November 2019): 523–525. https://doi.org/10.1093/qjmed/hcu227.
- Cao, Huijuan,Chenjun Zhu, and Jianping Liu. “Wet cupping therapy for treatment of herpes zoster: a systematic review of randomized controlled trials.” Alternative Therapies in Health and Medicine vol. 16 no. 6 (Nov-Dec 2010): 48–54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3151529/.
- Cao, Huijuan, Mei Han, Xun Li, Shangjuan Dong, Yongmei Shang, Qian Wang, Shu Xu, Jianping Liu. “Clinical research evidence of cupping therapy in China: a systematic literature review.” BMC Complementary and Alternative Medicine vol. 10 (November, 2010):1-10. http://www.biomedcentral.com/1472-6882/10/70.
- Cao, Huijuan , Xun Li, Jianping Liu. “An Updated Review of the Efficacy of Cupping Therapy.” PLoS ONE vol. 7 no. 2 (February, 2010): 1-14. doi:10.1371/journal.pone.0031793.
- Cao, Huijuan, Xun Li, Xue Yan, Nissi S. Wang, Alan Bensoussan, Jianping Liu. “Cupping therapy for acute and chronic pain management: a systematic review of randomized clinical trials.” Journal of Traditional Chinese Medical Sciences vol. 1 no. 1 (December 2014): 49-61. http://dx.doi.org/10.1016/j.jtcms.2014.11.003.
- Chan, Stephanie. “Cupping: The Eastern Practice Embraced by Michael Phelps and Hollywood Types Explained.” The Hollywood Reporter. August 8, 2016. Accessed December 2019. https://www.hollywoodreporter.com/news/what-is-cupping-michael-phelps-918060.
- Chi, Lee-Mei , Li-Mei Lin, Chien-Lin Chen, Shu-Fang Wang, Hui-Ling Lai, and Tai-Chu Peng. “The Effectiveness of Cupping Therapy on Relieving Chronic Neck and Shoulder Pain: A Randomized Controlled Trial.” Evidence-Based Complementary and Alternative Medicine, vol. 2016 (2016). https://doi.org/10.1155/2016/7358918.
- Chirali, Ilkay Zihni (additional authors firstname lastname). Traditional Chinese Medicine Cupping Therapy. 3rd ed. Churchill Livingstone, 2014.
- “Cupping.” National Center for Complementary and Integrative Health. Last modified November 09, 2018. Accessed September 2019. https://nccih.nih.gov/health/cupping.
- Dearlove, J., A. P. Verguei, N. Birkin and P. Latham. “An Anachronistic Treatment For Asthma.” British Medical Journal (Clinical Research Edition), Vol. 283, No. 6307 (December, 1981): 1684-1685. https://www.jstor.org/stable/29504720.
- Gecsedi, Renee and Georgia Decker. “Incorporating Alternative Therapies into Pain Management.” The American Journal of Nursing, Vol. 101, No. 4, (April, 2001): 35-39. https://www.jstor.org/stable/3522455.
- Gubb, Alfred S. “Cupping, Dry And Wet.” The British Medical Journal, Vol. 1, No. 3250 (April, 1923): 639. https://www.jstor.org/stable/20423115.
- Hon, Kam Lun E. , David Chi Kong Luk, Kin Fon Leong, and Alexander K. C. Leung. “Cupping Therapy May be Harmful for Eczema: A PubMed Search.” Case Reports in Pediatrics vol. 2013 (September, 2013): 1-3. http://dx.doi.org/10.1155/2013/605829.
- Ingall, Marjorie. “Everything You Ever Wanted to Know About Cupping—and Some Stuff You Probably Didn’t.” Tablet Magazine, August 11, 2016. https://www.tabletmag.com/scroll/210759/everything-you-ever-wanted-to-know-about-cupping-and-some-stuff-you-probably-didnt.
- Johannes, Laura. “Centuries-Old Art of Cupping may Bring Some Pain Relief.” Health & Wellness. The Wall Street Journal. November 13, 2012.
- Khalil, Mohamed K.M., Sulaiman Al-Eidi, Meshary Al-Qaed, and Saud AlSanad. “Cupping therapy in Saudi Arabia: from control to integration.” Integrative medicine research vol. 7 no. 3 (September, 2018): 214-218. doi: 10.1016/j.imr.2018.05.002.
- Kim, Jong-In , Myeong Soo Lee, Dong-Hyo Lee, , Kate Boddy, and Edzard Ernst,. “Cupping for Treating Pain: A Systematic Review.” Evidence-ased complementary and alternative medicine: eCAM vol. 2011 (2011): 1-7. doi: 10.1093/ecam/nep035.
- Kim, Jong-In , Tae-Hun Kim, Myeong Soo Lee, Jung Won Kang, Kun Hyung Kim, Jun-Yong Choi1, Kyung-Won Kang, Ae-Ran Kim, Mi-Suk Shin, So-Young Jung, and Sun-mi Choi,. “Evaluation of wet-cupping therapy for persistent non-specific low back pain: a randomised, waiting-list controlled, open-label, parallel-group pilot trial.” Trials vol 12 (2011). doi:10.1186/1745-6215-12-146.
- Kim, Seoyoun, Sook-Hyun Lee, Me-Riong Kim, Eun-Jung Kim, Deok-Sang Hwang, Jinho Lee, Joon-Shik Shin, In-Hyuk Ha, and Yoon Jae Lee. “Is cupping therapy effective in patients with neck pain? A systematic review and meta-analysis.” BMJ Open vol. 8 no. 11 (November, 2018 Year): 1-13. doi: 10.1136/bmjopen-2017-021070.
- Köhle, Natalie. “Cups, Needles, and Noxious Blood” in Control. Edited by Jane Golley, Linda Jaivin, Luigi Tomba. ANU Press, 2017. https://www.jstor.org/stable/j.ctt1sq5tvf.19.
- Leith, David. “The “Diatritus” and Therapy in Graeco-Roman Medicine.” The Classical Quarterly, New Series, Vol. 58, No. 2 (December, 2008): 581-600. https://www.jstor.org/stable/27564187.
- Manson, A. J. “Dry Cupping in Labour.” Association Medical Journal, Vol. 2, No. 54 (January, 1854): 36-37 https://www.jstor.org/stable/25495255.
- Mehtaa, Piyush and Vividha Dhapte. “Cupping therapy: A prudent remedy for a plethora of medical ailments.” Journal of Traditional and Complementary Medicine vol. 5 no. 3 ( July 2015): 127-134. https://doi.org/10.1016/j.jtcme.2014.11.036.
- Miller, Christine. “The History of Negative Pressure Wound Therapy (NPWT): From ‘‘Lip Service’’ to the Modern Vacuum System.” Journal of the American College of Clinical Wound Specialists vol. 4 no. 3 (2014): 61-62. http://dx.doi.org/10.1016/j.jccw.2013.11.002.
- Mohammad Al-Bedah, Abdullah, Tamer Shaban, Amen Suhaibani, Ibrahim Gazzaffi, Mohammed Khalil, and Naseem Akhtar Qureshi. “Safety of Cupping Therapy in Studies Conducted in Twenty One Century: A Review of Literature.” British Journal of Medicine & Medical Research vol. 15 no. 8 (May, 2016): 1-12. DOI: 10.9734/BJMMR/2016/26285.
- Musumeci, Giuseppe. “Could Cupping Therapy Be Used to Improve Sports Performance?” Journal of Functional Morphology and Kinesiology vol. 1 no. 4 (October 2016): 373-377. https://doi.org/10.3390/jfmk1040373.
- Orwell, George. “How the Poor Die” in Fifty Orwell Essays. Edited by Colin Choat. Project Gutenberg of Australia, 2003. http://gutenberg.net.au/ebooks03/0300011h.html#part39.
- Qureshi, Naseem Akhtar , Gazzaffi Ibrahim Ali, Tamer Shaban Abushanab, Ahmed Tawfik El-Olemy, Meshari Saleh Alqaed, Ibrahim S. El-Subai, Abdullah M.N. Al-Bedah. “History of cupping (Hijama): a narrative review of literature.” Journal of Integrative Medicine vol. 15 no. 3 (May, 2017): 172-181. http://dx.doi.org/10.1016/S2095-4964(17)60339-X.
- Shmerling, Robert H.. “What exactly is cupping?.” Harvard Health Publishing. Published September 30, 2016. Accessed September 2019. https://www.health.harvard.edu/blog/what-exactly-is-cupping-2016093010402.
- Soo Lee, Myeong, Jong-In Kim, Edzard Ernst. “Is Cupping an Effective Treatment? An Overview of Systematic Reviews.” Journal of Acupuncture and Meridian Studies vol. 4 no. 1 (March, 2011): 1-4. https://doi.org/10.1016/S2005-2901(11)60001-0.
- Valmyre, A. “Cupping.” The British Medical Journal, Vol. 1, No. 3295 (Feb. 23, 1924): 351-352. https://www.jstor.org/stable/20435844.
- Zhida, Tao. “Non-Drug Therapy in Medical Care.” India International Centre Quarterly vol. 18, no. 2/3 (SUMMER-MONSOON 1991): 155-160. https://www.jstor.org/stable/23002372.
MARIEL TISHMA currently serves as an Executive Editorial Assistant with Hektoen International. She has been published in Hektoen International, Argot Magazine, Syntax and Salt, The Artifice, and Fickle Muses. She graduated from Columbia College Chicago with a BA in creative writing and a minor in biology. Learn more at marieltishma.com.