Carrie Barron
Austin, Texas, USA
“He is the most un-talked about, unacknowledged, unknown and most important figure in the African American community…A genius.”1 In 1944, a surgeon with his trusted guide by his side performed the very first open-heart surgery on a fifteen-month-old, nine-pound girl.
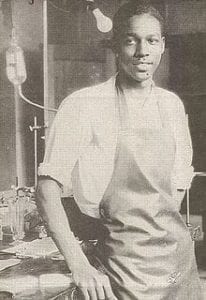
1930, Nashville. A twenty-year old African-American man, honors student, and son of a carpenter had his eyes set on becoming a physician. This was not unfounded. In his middle class community there were fire fighters, doctors, and teachers. Working as a carpenter he saved for seven years to finance his education. But then the Great Depression hit, banks foreclosed, and he lost everything. To support his wife and two children, he needed a job. A doctor at Vanderbilt was looking for someone to assist in his research lab. When Mr. Vivien Thomas entered the lab and met Dr. Alfred Blalock, the world would be forever changed.
The job was to clean the lab and the cages of the animals used for experiments. Dr. Blalock, a onetime playboy from a prominent family in Georgia had evolved into a passionate researcher. He was studying shock. Many soldiers’ lives had been lost due to this cardiovascular condition. Vivien gazed at the shelf of medical text books and the table of test tubes and took the job. His title was janitor.
There was something about Vivien. Blalock had been looking for “someone I can teach to do anything I can do and maybe do things I can’t do.”2 On the second day, by the time Blalock arrived, Vivien had set up the experiment and anesthetized the dog. He quickly learned to calculate the equations for experiments, perform them, and record the data meticulously. Soon Vivien was conducting vascular and thoracic experiments on the animals.2 Impressed with Vivien’s talent, drive, and poise, Blalock, needing a capable collaborator, promoted him to lab technician.
During one particularly intense case, Vivien made a small error. Blalock, whose explosive temper was legion, screamed, cursed, and excoriated Vivien. Or tried to. Vivien waited until he was done, said, “I was not raised to accept language like that,” picked up his hat, and headed for the door. “I am sorry, Vivien. It won’t ever happen again.”1 Apparently, it did not.
In 1941, Blalock, who had been turned down by Johns Hopkins for a residency for mediocre grades, was offered Chair of Surgery because of the work he and Vivien had done on blood transfusions.3 This innovation saved the lives of thousands of soldiers. Blalock would agree only if a position could be created for Vivien. For Vivien, this meant sacrificing nearby family, a home he had built himself, tree-lined streets in a commodious community, and his wife’s sense of comfort. Higher ambition, or perhaps a higher calling beckoned.4
When they entered their new research lab, the odor was putrid, the space was strewn with debris, and the equipment antiquated. The hallowed halls, bathrooms, and cafeterias of Hopkins were segregated. African Americans were relegated to lower floors and menial jobs. The city was even worse. There was no acceptable home for Vivien and his family that compared to their home in Nashville, but finally, he located a decent dwelling.
Sometimes Vivien and Blalock stayed late in the lab to talk while Blalock smoked his second pack of cigarettes. In spite of having had tuberculosis, he took his chances. Outside those walls, it was different. A random person might direct Vivien to get their coffee and use derogatory language when addressing him. He still strode the halls in his crisp white lab coat. Dr. Blalock suggested that he remove it so as to avoid the racist assaults. Vivien was also troubled by the fact that he was paid a janitor salary for a lab technician job. Though Blalock tried to get him more pay, he was only marginally successful in a rigid, hierarchical, and racist system.
Vivien kept working. He was doing good work, great work, or perhaps “God’s work.” They both understood that he surpassed Blalock in surgical expertise. He had practiced extensively on the animals and was also naturally gifted. Blalock said that Vivien’s hands were more important to him than his own. Once Blalock put his hands inside an animal to inspect a suture that Vivien had made. “Did you do that Vivien? It feels like something the Lord made.”5
Then in 1943 a young woman, the first female pediatric cardiologist at Hopkins, joined the department. Her name was Dr. Helen Taussig, and she had attended Hopkins for medical school. She was partially deaf from whooping cough as a child. Through her custom-designed stethoscope and her laying of hands, she could diagnose heart disease.
At the time, the congenital condition known as “blue baby syndrome,” or tetralogy of Fallot, was fatal. Four separate heart defects caused decreased blood flow to the lungs. The children presented with blue lips and fingers and cyanotic skin. After taking a few steps, they could not breathe and had to sit down. Most barely made it to three years of age. Taussig noted that their condition worsened after the patent ductus arteriosis, which connects the main pulmonary artery to the descending aorta, closed naturally soon after birth. Usually the closure is protective for the lungs, but Taussig surmised that this open duct could be an asset. Could constructing a ductus that connected the heart to the lungs save blue babies?6
At the time, open heart surgery was considered impossible, even amoral as the patient would surely die on the table. These babies were dying anyway. When Taussig approached Thomas and Blalock with her idea about changed “piping” they were intrigued. The trio tried and failed but then figured out a way. By taking a branch of the subclavian or carotid artery, dividing it, and connecting it to the pulmonary artery, blood flow was increased to the lungs. It had worked in a dog. Could it be done in a baby?7
In 1944, for a baby named Eileen Saxon, there was no time left. In spite of the admonishment of colleagues, Blalock decided to operate. Tiny Eileen was wheeled into the operating room with observing surgeons in the surround. Although he had invented the instruments for the procedure, Vivien was not permitted in the operating room. This presented a conundrum: Blalock could not perform the procedure without him. Vivien had done hundreds of these operations in the animals and Blalock only one. Blalock needed Vivien’s help, or Eileen could die.
“Where is Vivien!?” Blalock shouted. Someone scrambled to locate Vivien. Once scrubbed in, he stepped up on a stool behind Blalock to guide the surgeon through each step. Her arteries were miniscule. Her heart rate could not drop for too long. Blalock checked with Vivien. “Is this all right, Vivien?” “Is the incision long enough?” “Watch, Vivien, and don’t let me put these sutures in wrong!”8 After ninety minutes, the last stitch was in. There was no bleeding from the suture. Then someone said, “Look!” Blalock leaned over to see a “glorious pink color” flowing into Eileen’s little lips and face. It was a miracle. Or rather a miraculous achievement by “a chain-smoking surgeon, a deaf female doctor, and a self-taught African-American lab tech.”6
Those who had said it was unethical and those who had said to go forth, cried that day. Soon hundreds of parents of “blue babies” flocked to Johns Hopkins. Blalock became famous all over the world and a celebration was held in his honor at an exclusive hotel. Vivien was there, but he was tasked with serving drinks because the hotel was segregated. Vivien’s monumental role in this groundbreaking operation was not mentioned. Of the 300 articles Blalock published, Vivien is credited in only two.8
In 1976, Vivien Thomas was awarded an honorary doctorate. He had helped discover the cause of traumatic shock, designed the first operation to treat tetralogy of Fallot, conducted the first atrial septectomy, and helped develop the electrical defibrillator.8 Generations of surgeons at Johns Hopkins, whom he had trained, returned for the ceremony. A surprise was in store. The day Vivien received his diploma, his portrait was unveiled. Tears rolled and people rose from their seats in respect. The “Old Hands” Club of Johns Hopkins surgeons had commissioned the piece, and today it hangs on the wall next to the portrait of Dr. Alfred Blalock. Dr. Vivien Thomas continued as a medical school faculty member, surgical instructor, and director of the research lab. One trainee said that he was masterful at breaking down complex procedures into simple steps and could teach just about anybody.1 Re-naming the Blalock-Taussig shunt the Blalock-Taussig-Thomas shunt and doing what one can to correct a corrosive, unethical past has been proposed.9
Current medical literature is replete with articles about how to teach or facilitate character, caring, ethics, integrity, and humanism in medical trainees. History offers wisdom but history forgets or neglects some remarkable people, especially if they are persons of color. The “unacknowledged, un-talked about and unknown,”1 invisible10 genius Dr. Vivien Thomas epitomized the highest ideals in medicine. He may be the one of the greatest role models we have ever had.
References
- Kalin A, Potter L, Freeman M, et al. Partners of the heart. Distributed by PBS Home Video2004.
- Thomas V, Thomas V. Partners of the heart : Vivien Thomas and his work with Alfred Blalock : an autobiography. Philadelphia: University of Pennsylvania Press; 1985.
- Blalock A. Shock: further studies with particular reference to the effects of hemorrhage. 1934. Archives of surgery (Chicago, Ill : 1960). 2010;145(4):393-394.
- Joyner A, Yeo CJ, Maxwell PJ. Vivien Thomas: master craftsman, gifted teacher, and unsung hero. The American surgeon. 2015;81(2):118-120.
- Sargent J, Rickman A, Mos D, et al. Something the Lord made. HBO Films2004.
- Morris T. The Underdog Doctors Who Saved America’s “Blue Babies”. Narratively2018, January 31.
- Evans WN. The Blalock-Taussig shunt: the social history of an eponym. Cardiology in the young. 2009;19(2):119-128.
- Ng CT. Vivien Thomas (1910-1985): the backstage pioneer and educator. Journal of investigative surgery : the official journal of the Academy of Surgical Research. 2014;27(3):131-138.
- Brogan TV, Alfieris GM. Has the time come to rename the Blalock-Taussig shunt? Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2003;4(4):450-453.
- Hamlett R. Heart Surgery’s Invisible Man. The Baltimore Sun 1993, November 4.
CARRIE BARRON, MD, is a psychiatrist and psychoanalyst. At Dell Med, she serves as the Director of Creativity for Resilience. In her book The Creativity Cure, Dr. Barron promotes insight, writing, creating, and quality relationships for wellbeing. Her work has been featured in peer-reviewed journals, magazines, podcasts, blogs, and speaking events across the country, and her Psychology Today blog has had over three million readers.

Leave a Reply