Mariel Tishma
Chicago, Illinois, United States
 |
| Clara Louise Maass portrait. Credit: National Museum of Health and Medicine. CC BY 2.0. |
Clara Maass was born on June 28, 1876, in the quiet New Jersey township of East Orange. The oldest daughter of Hedwig and Robert E. Maass, she grew up helping to raise and provide for her eight younger siblings. She learned quickly to put others’ needs before her own, finding her first paying job at the age of fifteen, after having started work five years earlier as an unpaid “mother’s helper.”1 Her early experiences in caregiving aided her when, at seventeen, she entered nursing school at the Newark German Hospital. As the child of German immigrants, she was able to tend especially well to the area’s German-speaking population, an attribute the hospital had been searching for. She graduated in 1895, and rose quickly through the ranks, becoming the hospital’s head nurse three years later.
In 1898, following her appointment as head nurse, the Spanish-American War broke out. While this would not have an immediate effect on Maass, news of the war inevitably traveled. Perhaps more importantly, after initial reluctance, the US Army recognized the need for female nurses in the war effort. Consequently, they began a search and hired 1,563 contract nurses to care for the sick and wounded.2 Clara Maass was one of them.
Maass gave up her role as head nurse and volunteered twice during the war’s duration. After her initial four-month contract ended, she joined again, expanding her travels to include the southern states and as far from her home as Manila in the Philippines. Her second contract was cut short after seven months when she fell sick with dengue but this was the only thing that halted her tireless work.3
More soldiers in the Spanish-American War died from sickness than from battle wounds, and Maass likely suspected this before she volunteered as a contract nurse. Once her work began, she learned the full extent of the role of infection as she was exposed to typhoid, malaria, and yellow fever. This may have been her first encounter with these diseases, but she herself did not contract them during her service, partially due to the improved sanitation measures used by the nurses, but also from luck. At the time, the transmission vectors for typhoid and yellow fever had not been confirmed and knowledge of the mosquito vector for malaria was relatively new, having been discovered by Ronald Ross in the mid-1890s.4
Her service as a contract nurse would not be the last time Maass would cross paths with yellow fever, but before the two would meet again, the method of transmission would be confirmed. The work of this discovery had begun with Dr. Carlos Finlay,5 but was completed by Major Walter Reed and the U.S. Army Fourth Yellow Fever Commission Board.
The Yellow Fever Commission Board was formed May 23, 1900.6 Prior to their work, a bacteriologist named Giuseppe Sanarelli claimed to have isolated the organism causing yellow fever, and in order to prove it he had injected it into five patients. These patients were uninformed they were part of an experiment and three of them died. The scientific community reacted with appropriate outcry, putting pressure on Reed and his team to get things right in their own experiments.7 Their first steps toward ethical experimentation began with self-experimentation.
After many fruitless experiments, two members of Reed’s team — though not Reed himself — were inoculated by infected mosquitoes in August and September 1900. Dr. James Carroll and later Dr. Jesse Lazear were inoculated. Whether Lazear’s infection was accidental or intentional remains unclear. Regardless, both men contracted severe yellow fever; Carroll survived, but Dr. Lazear died one week after inoculation.8 His death halted the team’s self-experimentation and drew the attention of the Army. Both men’s contraction of yellow fever was enough to reinforce the necessity of the trials – as more civilian deaths from the disease were likely – while also adding needed proof to the mosquito vector theory. 9 The scientific community now on their side, further trials were required in order to convince the theory’s detractors, including those in governmental power. Once these detractors were convinced, further moves could be made to eliminate mosquitoes and control the disease. To this end, the team was given permission to recruit outside volunteers.10
Volunteers for the second round of study were carefully selected, and each was paid $100 for participating and an additional $100 if they contracted yellow fever. Monetary payment for medical trials remains controversial today, but at the time was an improvement over the unpaid and undisclosed trials of the past. Throughout the process, “Reed and his colleagues took pains to ensure that volunteers understood the risks associated with their participation in the experiments,”11 up to and including explaining that in the event of their death their payment would go to their appointed next of kin. Participants willing to move forward signed a contract declaring they knew the risks, and the experiment could begin. After this second round of trials, the mosquito vector theory was confirmed.
Following Reed’s studies, doctors in Havana, Cuba, began investigating immunity to yellow fever. Specifically, they wanted to discover if surviving an infection, especially one medically induced, made one immune – an important first step towards a vaccine. At the time Havana was struggling to contain an epidemic of yellow fever, so any steps to control the disease were given priority. As part of this effort, Dr. William Gorgas at Las Animas hospital began to gather volunteers for a new yellow fever experiment. This is where Clara Maass re-enters the story, as she volunteered for Dr. Gorgas.12 The other participants included soldiers, Cuban citizens, and several Spanish immigrants to Cuba. Twenty-eight initial inoculations took place, and only one volunteer developed mild yellow fever. However, in a second round of fourteen injections, seven volunteers developed yellow fever and three died.13
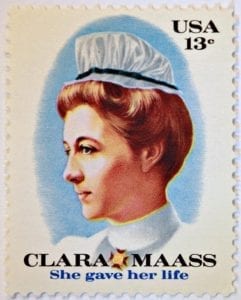 |
| US stamp honoring Maass. C. 1976. Photograph by John Flannery. CC BY-SA 2.0. |
Maass was inoculated for the first time in June 190114 but became infected after a second trial on August 14. She died ten days later, the only American to die as part of Gorgas’ trials. Her motivation for participating was tied to her desire to serve. She believed that if she became infected and survived, she would no longer be at risk of contracting yellow fever and would be better able to care for patients with the disease. The other two participants to die were Spanish immigrants, who in essence wanted to get yellow fever “over with.” One civilian volunteer stated, “I suspected that I would probably get it [yellow fever] spontaneously anyhow, so I decided I’d rather have it under favorable circumstances.”15
There is no evidence that Maass, or any other participant under Gorgas, signed a consent form. Reed’s experiments did increase documentation of consent for a few US researchers, but did not become standard procedure until years later. However, as a nurse Maass had an intimate view of what yellow fever could do, and what it might do to her if she contracted it, including death. With this awareness, she still chose to volunteer for the experiment, making her consent informed, even if she did not give official informed consent. In a way, her volunteering could be considered an extension of Reed’s team’s self-experimentation. She had already been a part of the medical community’s fight to treat and eradicate yellow fever through her nursing work. By participating in the experiment, she escalated that involvement. The Cuban citizens who participated and likely had seen members of their communities or families succumb to the disease volunteered with a similar awareness.
The same cannot be said for the immigrant participants in the study, who volunteered hoping to become immune. They had heard of the disease, and had been warned they would likely contract it, but there was no way for them to know exactly what it entailed without having seen it first hand, as Maass had.
Maass’ death put an end to the yellow fever experiments. With her death publicized, the Cuban public finally accepted mosquitoes as the vector for the disease. Havana was able to begin controlling the mosquito and eventually the disease. Even still, there was a reaction in the US to the yellow fever experiments, specifically those that paid volunteers. An editorial published in The Hospital in October 1901 stated that “we should still question the morality of healthy people selling themselves for experimental purposes,” regardless of whether participants lived or died.16 This is a debate that continues today, and answers are not easy to reach.
It also cannot be ignored that figures like Reed and Maass are the most well remembered from this incident (at least to US audiences) whereas the Spanish immigrants to Cuba, Cuban citizen participants, and the Cuban and Spanish physicians who laid the groundwork for the research have not earned the same fame. They also risked careers, and some lost their lives.
Still, looking through the scope of history if it had not been for the work of Reed and the sacrifice of Maass, the confirmation of the mosquito vector theory and control of Havana’s yellow fever epidemic may have remained out of reach. Their legacy remains important, as Reed’s contract was an essential part of the progression toward ethical medical experimentation and informed consent. Clara Maass’ death transformed her into a martyr and hero, honored for her dedication to the service of others. In that spirit, we must not forget the others who died for the same cause she did — helping the many.
End Notes
- Enrique Chaves-Carballo. ” Clara Maass, Yellow Fever and Human Experimentation” Military Medicine 178, no. 5 (2013): Accessed January 25, 2019. https://doi.org/10.7205/MILMED-D-12-00430.
- Ibid.
- Ibid.
- Russell Roberts. Discover the Hidden New Jersey. (New Brunswick, New Jersey: Rutgers University Press, 1995), 51.
- Susan E Lederer. “Walter Reed and the Yellow Fever Experiments.” in The Oxford Textbook of Clinical Research Ethics, ed. Ezekiel J. Emanuel, Christine C. Grady, Robert A. Crouch, Reidar K. Lie, Franklin G. Miller, and David D. Wendler. (New York, Oxford University Press, 2008), 10.
- Chaves-Carballo. “Clara Maass, Yellow Fever and Human Experimentation”
- Lederer. “Walter Reed and the Yellow Fever Experiments.” 4.
- Achil Mehra. “Politics of Participation: Walter Reed’s Yellow-Fever Experiments.” Virtual Mentor 11, no. 4 (2009): Accessed January 25, 2019. doi: 10.1001/virtualmentor.2009.11.4.mhst1-0904. 327.
- Ibid, 328.
- Lederer. “Walter Reed and the Yellow Fever Experiments.” 10.
- Ibid. 12.
- Roberts. Discover the Hidden New Jersey. 52.
- Chaves-Carballo. ” Clara Maass, Yellow Fever and Human Experimentation”
- “CLARA LOUISE MAASS.” American Association for the History of Nursing (AAHN). Accessed January 25, 2019. https://www.aahn.org/maass.
- Mehra. “Politics of Participation: Walter Reed’s Yellow-Fever Experiments.” 328.
- “The Yellow Fever Experiments in Havanna (1901)” The Hospital 31, no. 784 (1901): 2 Accessed January 25, 2019.
References
- Chaves-Carballo, Enrique. ” Clara Maass, Yellow Fever and Human Experimentation” Military Medicine 178, no. 5 (2013): 557-562. Accessed January 25, 2019. https://doi.org/10.7205/MILMED-D-12-00430.
- “CLARA LOUISE MAASS.” American Association for the History of Nursing (AAHN). Accessed January 25, 2019. https://www.aahn.org/maass.
- Lederer, Susan E. “Walter Reed and the Yellow Fever Experiments.” in The Oxford Textbook of Clinical Research Ethics, edited by Ezekiel J. Emanuel, Christine C. Grady, Robert A. Crouch, Reidar K. Lie, Franklin G. Miller, and David D. Wendler, 9-17. New York, Oxford University Press, 2008.
- Mehra, Achil. “Politics of Participation: Walter Reed’s Yellow-Fever Experiments.” Virtual Mentor 11, no. 4 (2009): 326-330. Accessed January 25, 2019. doi: 10.1001/virtualmentor.2009.11.4.mhst1-0904.
- Roberts, Russell. Discover the Hidden New Jersey. New Brunswick, New Jersey: Rutgers University Press, 1995.
- “The Yellow Fever Experiments in Havanna (1901)” The Hospital, 31, no. 784 (1901): 2 Accessed January 25, 2019.
MARIEL TISHMA currently serves as an Executive Editorial Assistant with Hektoen International. She’s been published in Hektoen International, Argot Magazine, Syntax and Salt, The Artifice, and Fickle Muses. She graduated from Columbia College Chicago with a BA in creative writing and a minor in biology. Learn more at marieltishma.com.
Highlighted in Frontispiece Volume 11, Issue 2– Spring 2019
Winter 2019 | Sections | Women in Medicine

Leave a Reply