Annabelle S. Slingerland
Boston, Massachusetts, United States
108 Bay State Road
Spanning over three generations of leading ophthalmologists, the Beetham Eye Institute has contributed to major breakthroughs in diabetes eye care, from the first location of Dr. William P. Beetham’s ophthalmology practice at 108 Bay State Road in Boston to its current role as the ophthalmology section of the Joslin Diabetes Center. At the beginning of the twentieth century many doctors, such as Drs. Joslin and Beetham, had been attracted to the Back Bay section of Boston. There, Dr. Elliott P. Joslin had treated many people with diabetes in his practice and often encouraged them to “Live so that you may profit from some new discovery.” The discovery of insulin in 1921 transformed the outlook of the patient with diabetes, but it soon became apparent that living with diabetes could mean developing complications such as neuropathy, nephropathy, and retinopathy.
To address this increasing prevalence of diabetic eye disease, it was natural that Dr. Beetham should develop strong ties with Dr. Joslin. By 1933-34, Dr. Joslin had moved his office to the Baker Clinic of the New England Deaconess Hospital, where Dr. Beetham, who had become the principal eye doctor to Dr. Joslin’s patients, performed his eye surgery. Later, in the mid-1960s, Drs. Aiello and Beetham began caring for patients at the Joslin Building, and by the early 1970s they moved their practice to the Joslin Building as part of the Joslin Diabetes Foundation, as the Joslin Diabetes Center was then called.
Progress in diabetic retinopathy

For a long time the ocular complications of diabetes had not been well studied, but in 1935 Drs. Beetham and Waite published in the New England Journal of Medicine a landmark study on the visual mechanisms in diabetes mellitus. Other publications followed and Dr. Beetham’s scholarly approach was continued through several Joslin papers. In 1954-6, Dr. J. Ditzel published on the relationship of retinal changes and glucose control, and photography of the fundus in the early 1950s helped characterize the retinal changes. In 1952, Dr. Beetham had reported the ominous prognosis of patients with proliferative diabetic retinopathy in that 73% of those so diagnosed died within five years; that any degree of diabetic retinopathy at the onset of pregnancy reduced the chance of a successful pregnancy to less than 47%; and that no pregnant woman with proliferative diabetic retinopathy at the onset of pregnancy maintained useful vision herself, even if the pregnancy itself was successful. In the 1990s, the findings of the Diabetes Control and Complications Trial (DCCT) for type 1 diabetes and the United Kingdom Prospective Diabetes Study (UKPDS) for type 2 diabetes confirmed the benefits of intensive glucose control in delaying the onset and slowing the progression of diabetic retinopathy, as Drs. Joslin and Beetham had emphasized half a century earlier.
Breakthrough in ophthalmology, Ruby Laser
As Dr. Beetham’s practice became integrated into the Joslin Diabetes Foundation, Dr. Beetham and his son-in-law, Dr. Lloyd M. Aiello, began to investigate new approaches to diabetic retinopathy. Building on the observation that eyes with significant chorio-retinal scarring were less likely to progress to proliferative diabetic retinopathy, Drs. Beetham and Aiello produced chorio-retinal scars using a ruby laser to treat eyes with proliferative disease, the first treatment being initiated on February 7, 1967. Treating one eye with laser and using the other as an untreated control, they scattered ruby laser scars over wide regions of the retina, leaving the macula area untouched. In their initial reports, they found 80% improvement in treated eyes, with complete resolution of neovascularization in 54% of the eyes. All of the untreated eyes were unchanged or had worsened, while no eyes treated with the ruby laser progressed. The study of Drs. Beetham and Aiello was the first controlled clinical trial to test the effect of scatter panretinal photocoagulation on preserving vision for persons with advanced diabetic retinopathy.
Dr. Aiello recollects that with the established benefit of panretinal laser photocoagulation, he would care for 60-90 patients a day and perform 15-20 laser treatments per day. Every pregnant patient would be monitored every 2-3 months during her pregnancy. While Drs. Aiello and Beetham’s experience with the ruby laser demonstrated beneficial results, their treatments were also met with criticisms. The side effects of the treatments, including difficulty in dark adaptation and loss of peripheral field vision, and the idea of selectively destroying retinal tissue, resulted in significant criticism until the dramatic benefits became widely appreciated.
To address the growing problem of vision loss from diabetes, the Airlie House Symposium in 1968 brought together leading diabetes clinicians and researchers from around the world. Sponsored by the U.S. Public Health Service and held at Airlie House, Warrenton, Virginia, the group debated the effects of tight metabolic control, pituitary ablation, and photocoagulation on treatment for diabetic eye disease. The outcomes of this meeting were significant: the group summarized areas of consensus and disagreement, devised a standard classification of diabetic retinopathy, and made a proposal for controlled clinical trials to investigate the treatment of diabetic retinopathy.
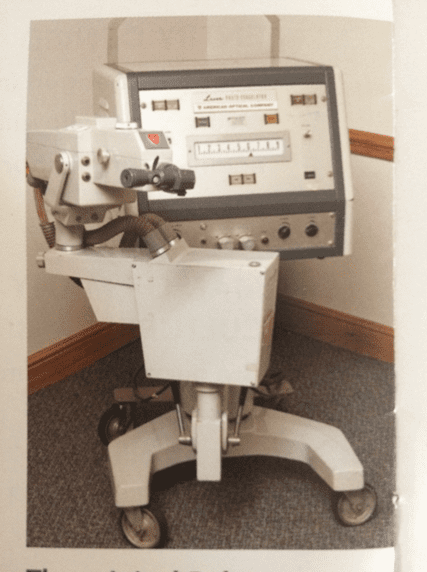
Eyes on diabetes
Following the Airlie House Symposium, the National Eye Institute of the U.S. National Institutes of Health funded the Diabetic Retinopathy Study (DRS) in 1971. This multi-centered clinical trial tested panretinal photocoagulation with an argon laser or a xenon arc photocoagulator versus no treatment to preserve vision in eyes with proliferative diabetic retinopathy. The ruby laser, initially planned in the study as practiced by Drs. Beetham and Aiello, was replaced by the argon laser in the study design due to the argon laser availability and comparative ease of application of laser scars due to the delivery mechanism, although the argon laser’s benefits in panretinal photocoagulation lacked data. The outcomes of the DRS firmly established the benefit of panretinal photocoagulation in preserving vision for persons with proliferative diabetic retinopathy. Dr. Aiello served on the executive committee for the study and as principal investigator at Joslin Clinic for the DRS, which validated the earlier work with the ruby laser.
While the DRS demonstrated the benefit of photocoagulation in preserving vision, several questions regarding the treatment remained unanswered, particularly the timing of initiating the treatment and the possible benefit of laser photocoagulation to treat diabetic macular edema. In 1979, the United States National Eye Institute funded the Early Treatment Diabetic Retinopathy Study (ETDRS). This multi-centered clinical trial enrolled more than 3700 patients at twenty-two clinical sites in the US. The goals of the trial were to study the effect of aspirin on the progression of retinopathy, investigate laser photocoagulation for diabetic macular edema, and elucidate the timing for the initiation of panretinal laser photocoagulation for diabetic retinopathy. The BEI enrolled the largest number of patients for the study and Dr. Aiello served as study co-chairperson. This study demonstrated that 650 mg of aspirin daily had no beneficial or deleterious impact on the progression of diabetic retinopathy, that focal laser photocoagulation for diabetic macular edema as applied in the study reduced the risk of moderate vision loss (a doubling of the visual angle) by approximately 50%, and that scatter (panretinal) laser photocoagulation for diabetic retinopathy reduced an eye’s risk of severe vision loss (best correct acuity of 5/200 or worse) to less than 4%. The benefit of scatter photocoagulation was realized whether the eye was treated early (before the development of high-risk proliferative diabetic retinopathy) or as an eye approached or reached the high-risk stage, although those with type 2 diabetes or type 1 diabetes of long duration experienced better outcomes with earlier treatment.
Recognizing that many persons with diabetes worldwide did not receive or have access to sight-preserving care, in 1990 Drs. Lloyd M. Aiello and Sven Bursell, then at the Beetham Eye Institute, initiated and developed the Joslin Vision Network Diabetes Eye Care Program (JVN). The goal of this program is to extend access to evidence-based diabetic retinal evaluation through a telemedicine program that captures retinal images and pertinent health information to diagnose a level of diabetic retinopathy and recommend an appropriate follow-up and care plan. Rigorously validated for image capture, image grading and review, and patient care follow-up, the JVN has acquired more than 3,000,000 retinal images since its first clinical deployment in June 1999. The BEI continues to be a recognized international leader in telemedicine for diabetic retinopathy.
Third Generation
Dr. Lloyd Paul Aiello, the son of the BEI’s founding director Dr. Lloyd M. Aiello and the grandson of Dr. William P. Beetham, is the current Director of the BEI. In 1996, he teamed up with Dr. George King at Joslin to identify the role of vascular endothelial growth factor (VEGF) in the development of proliferative diabetic retinopathy and macular edema. These studies led to the development of intra-vitreous anti-VEGF agents to treat diabetic macular edema and proliferative diabetic retinopathy. In 2014, Drs. Aiello and King shared the Antonio Champalimaud Vision Award with other Harvard researchers for their efforts in investigating the role of VEGF in eye disease. Dr. Aiello’s work was also recognized by the Ernst H. Barany Prize of the International Society for Eye Research in Tokyo, Japan.
These intra-vitreous anti-VEGF treatments were investigated in the Diabetic Retinopathy Clinical Research Network (DRCR.net). Dr. Lloyd Paul Aiello was the inaugural chair of this research network that became the most prestigious for diabetic eye disease in the USA, being cited several times by Congress for excellence, and is world renowned. While Dr. Aiello has remained an active leader in the DRCR.net, BEI ophthalmologist Dr. Jennifer Sun, MD, MPH, currently serves as the network’s fourth chairperson.
The studies conducted by the DRCR.net established new paradigms for treating diabetic macular edema, revolutionizing the care of diabetic macular edema for which laser is now rare. In 2010 the DRCR.net published the results of their clinical trial, demonstrating that the intravitreous anti-VEGF agent ranibizumab was more effective than laser treatment in preserving vision and even recovering lost vision for eyes with diabetic macular edema involving the center of the macula. Subsequent study results from the DRCR.net demonstrated that the three commonly used anti-VEGF agents used for diabetic macular edema (ranibizumab, bevacizumab, and alflibercept) were all effective in reducing the risk of vision loss and recovering vision. Most recently, the DRCR.net has published study results demonstrating that intravitreous ranibizumab is not inferior to scatter (panretinal) laser photocoagulation in the treatment of proliferative diabetic retinopathy, and in fact is more effective with fewer side effects than laser photocoagulation in treating proliferative diabetic retinopathy. The treatments demonstrated in the DRCR.net are in the process of transforming our care of proliferative diabetic retinopathy.
Epilogue
The Beetham Eye Institute of the Joslin Diabetes Center currently has ten ophthalmologists and thirty staff of optometrists, ophthalmic technicians, eye imagers and readers, clinic and research coordinators, and specialists in telemedicine. With a leading role in the Diabetic Retinopathy Clinical Research Network (DRCR.net), the Beetham Eye Institute continues to play a leadership role in diabetes eye research. With the advancement of ocular telemedicine, the BEI has also taken a leadership role, extending with its Joslin Vision Network diabetes eye care to individuals who might not have access to specialty care. The goal is to prevent vision loss from diabetic retinopathy and ultimately discover a cure for this condition.
Further Reading
- Joslin Diabetes Center Research News, 2017.
- Joslin Diabetes Center, High Hopes, spring 2017, volume 1, number 1.
- D.M. Barnett.A brief history of diabetes from 1891 to 1988 through the publications of the Joslin Diabetes Center.
- D.M. Barnett. Dr. Joslin’s Magnificent Obsession.
- J.H. Waite and W.P. Beetham The Visual Mechanism in Diabetes Mellitus: a comparative study of 2002 diabetics, and 457 non-diabetics for control. N Engl J Med 1935;212:429-43: Published as one of the early ten monographs from 2012-1946, that left the textbooks and preceded the more rapidly published journal articles of today.
- W.P. Beetham. Visual prognosis of proliferating diabetic retinopathy. Br J Ophthalmol 1963;611-9.
- The Diabetic Retinopathy Study Research Group. Preliminary report of effects of photocoagulation therapy. The diabetic retinopathy study. Am J Ophthalmol. 1976;81:383-96.
- Joslin’s Diabetes Mellitus, 13th Ed. Edited by C.R. Kahn and G. C. Weir. Chapter 1. The History of Diabetes. L.P. Krall, R. L., D.M. Barnett. P1-14.
- E P. Joslin, MD A Centennial Portrait. Joslin Diabetes Center. D. M. Barnett.
- M.F. Goldberg MF, L.M. Jampol LM. Knowledge of diabetic retinopathy before and 18 years after the Airlie House Symposium on Treatment of Diabetic Retinopathy. Ophthalmology. 1987 Jul;94(7):741-6.
- Ditzel, Priscilla White, Janien Duckers. Diabetes Changes in the Pattern of the Smaller Blood Vessels in the Bulbar Conjunctiva in Children of Diabetic Mothers: A Preliminary Report. Diabetes. Mar 1954, 3(2) 99-106.
- Ditzel, P. White. Central retinal vein occlusion in juvenile diabetes, case report with consideration of the pathogenic relationship between diabetic retinopathy and retinal vein occlusion. J Chronic Dis. Mar 1956;3(3):253-62.
- Ditzel, U. Sagild. Morphologic and hemodynamic changes in the smaller blood vessels in diabetes mellitus. II. The degenerative and hemodynamic changes in the bulbar conjunctiva of normotensive diabetic patients. N Engl J Med. Apr 1954;250(14):587-94.
- H.F. Root, S. Mirsky, J. Ditzel. Proliferative retinopathy in diabetes mellitus; review of eight hundred forty-seven cases. J Am Med Assoc. Feb 1959;169(9):903-9.
- N.R. Keiding, H.F. Root, A. Marble. Importance of control of diabetes in prevention of vascular complications. J Am Med Assoc. Nov 8, 1952;150(10):964-9.
Acknowledgements
I wish to express my gratitude to those who held so many valuable stories and willingly shared them, to Drs. Jerry Cavallerano, Lloyd Paul Aiello, Lloyd M. Aiello, as well as to Dr. Donald Barnett and Matthew Brown for sharing to save, collect, document, archive, and write on every little detail of the history of the cradle of diabetes care and research. Special thanks also to Dr. Donna Younger for sharing her stories.
ANNABELLE S. SLINGERLAND, MD, DSc, MPH, MScHSR, has been inspired by the role of the Joslin Diabetes Center and Joslin’s Beetham Eye Institute (BEI) in understanding and treating diabetic eye disease and how their efforts have led to continuing advances both during the early days of diabetes care as well as today. The BEI staff continues to strive to preserve the vision of every single patient with diabetes and find the next breakthrough to change their lives. The BEI’s teamwork and devotion have made the BEI an inspiring institution.