Mindy Schwartz
Introduction

Few diseases have captured the imagination more than tuberculosis (TB). Tuberculosis fascinates many people – scientists and epidemiologists, artists and humanitarians, sociologists and physicians. It is as much the stuff of art and song as a merciless killer of the young and old. Even its name conjures the image of the waif with a chronic cough and worrisome hemoptysis. Edvard Munch’s picture of his sister Sophie captures the pathos.
Known since antiquity as consumption, tuberculosis remains one of the most important infections of mankind. Its study illustrates the social context of medicine and offers many important lessons. The effective oral therapies developed in the 1950’s ushered a wave of optimism, leading one to think that tuberculosis would soon be a thing of the past. Nothing could be further from the truth. Today, a third of the world’s population has been exposed and is infected with the organism, over 90% in the developing world. While tuberculosis has become less common in developed countries, the widespread expansion of HIV in Africa and throughout the world has caused a dramatic resurgence, with more than 8 million new cases each year worldwide and more than 2 million persons dying from it. Most victims are from countries that cannot offer modern drug therapy or even simple modern conveniences. Frightening also is the specter of antibiotic resistant tuberculosis, borne of inadequate treatment and rendering cure difficult and prohibitively expensive. The control of tuberculosis remains a global health issue. In the nineteenth century, TB was known as “the captain of all men of death” – and so it remains.
Background
Over time tuberculosis has been known by a variety of names including phthisis pulmonaris and consumption. Its organism, Mycobacterium tuberculosis, traces its roots back to soil organisms that existed 15,000 to 20,000 years ago. The well-known findings of advanced pulmonary tuberculosis are weight loss, fever, chronic productive cough, and at times dramatic, life-threatening hemoptysis. Usually contracted by inhalation, less commonly by ingestion, and rarely through an infected wound, it may affect other organs such as the bones – particularly the spine, kidneys, brain, lymph nodes, intestine, and skin.
Modern DNA techniques have facilitated the identification of tuberculosis, which has been documented in relics from ancient Egypt, India, and China. Classic findings of spinal tuberculosis, known as Pott’s disease, have been well documented in Egyptian mummies. Bone invasion by the mycobacterium causes the characteristic hunchback or hump, clinically known as a gibbus, and may have affected Quasimodo (Victor Hugo’s Hunchback of Notre Dame) and be the origin of the curved spine of familiar Southwest Kokopelli figure.

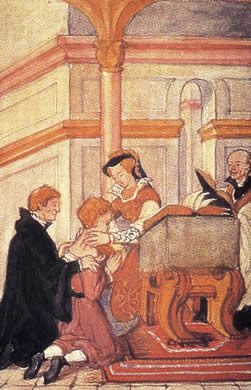
Scrofula
In the Middle Ages tuberculosis of the cervical lymph nodes was known as the “king’s evil” or scrofula – a term thought to derive from the Latin “scrofa,” meaning “sow”. It was widely believed that the kings of England and France had a “supernatural gift” to be able to cure scrofula simply by touching those affected. In the past, isolated tuberculous lymphadenitis may have been an infection with a more benign course, possibly leading to its widespread acceptance. The beginnings of this ritual were first performed by Clovis of France (481-511) and Edward the Confessor of England (1042-1066), and continued through Queen Anne (1665-1714) in the 18th century. King Charles II (1660-82) is said to have touched 92,102 people in his 22-year reign, touching as many as 600 in one ceremony. Over time the addition of a small gold piece was added to the touching ceremony. Shakespeare gave an accurate description of this well-known ritual in Macbeth (Act IV, Scene 3).
MACDUFF What’s the disease he means?
MALCOLM ‘Tis call’d the evil:
A most miraculous work in this good king;
Which often, since my here-remain in England,
I have seen him do. How he solicits heaven,
Himself best knows: but strangely-visited people,
All swoln and ulcerous, pitiful to the eye,
The mere despair of surgery, he cures,
Hanging a golden stamp about their necks,
Put on with holy prayers: and ’tis spoken,
To the succeeding royalty he leaves
The healing benediction. With this strange virtue,
He hath a heavenly gift of prophecy,
And sundry blessings hang about his throne,
That speak him full of grace.
The White Plague
Tuberculosis peaked in the 18th century in Western Europe having had a prevalence as high as 900 deaths per 100,000. The development of European cities created situations ripe for the spread of the infection by poor housing, primitive sanitation, malnutrition, and overcrowding. While the epidemic began to wane long before the modern advances in science and medicine, the reasons are still debated.
Tuberculosis and the arts
One of the most fascinating aspects of tuberculosis is its impact on the arts, literature, poetry, and music. There was once thought to be a direct association of tuberculosis and genius – as many of the greatest contributions to the arts and literature were made by those actively infected with tuberculosis. The list of famous artists who suffered from tuberculosis includes the poets John Keats and Percy Bysshe Shelley, the authors Robert Louis Stevenson, Emily Bronte, Katherine Mansfield, and Edgar Allen Poe, the musicians Nicolo Paganini and Frederic Chopin, and the artist Amadeo Modigliani. Many works of fiction emphasize tuberculosis as a common, familiar, and evocative condition. Victorian novels such as Dickens’ Nicholas Nickleby and Victor Hugo’s Les Miserables document the decline of the tubercular protagonists, as do the operas La Traviata and La Boheme.
Koch and the identification of tuberculosis
The nineteenth century was a watershed in the understanding of infectious disease. It is hard to underestimate the significance of Robert Koch’s demonstration of the causative organism, Mycobacterium tuberculosis, in 1882. The organism’s unique protein coat had delayed its identification until a specific staining technique was developed. Koch’s bacillus has been named AFB (acid fast bacilli) for the red-colored dye the organism retains. (Koch was awarded the Nobel Prize in 1905. He also made seminal contributions to photomicrography and developed plating and culturing techniques that are still used today). His discovery was followed shortly by the identification of the x-ray by Wilhelm Roentgen in 1895. This allowed early diagnosis and isolation of infected individuals.
Sanitaria
Another important development in the nineteenth century was the sanitarium movement. Initially started in Silelsia in 1859 by Hermann Brehmer, sanitaria, or places for treating chronic diseases, became widespread by the late 19th and early 20th centuries. In 1884, Edward Livingston Trudeau pioneered sanitaria in the U.S. with the creation of the Adirondack Cottage Sanitarium in Saranac Lake, New York. At its height, this sanitarium consisted of more than 50 buildings, with an infirmary, library, patient and staff cottages, a chapel, and its own post office. Like many similar institutions, it closed in 1954. Another sanitarium, at Davos in Switzerland, was the setting for Thomas Mann’s famous novel The Magic Mountain.
Sanitaria also became centers of discovery and treatment. Infectious persons were isolated from society and treated with rest and improved nutrition. In 1904, a group of concerned individuals, physicians and lay leaders, came together to form the National Tuberculosis Association, which later evolved into the American Lung Association. In 1907, Christmas seals were first used to help raise funds for sanitaria in Delaware. These were but a few of the widespread public health campaigns that helped contain tuberculosis in the U.S.
Immunization and BCG
One of the great advances begun in the nineteenth century was the development of the vaccination – the deliberate exposure to infectious agents (or their derivatives) to stimulate the immune system to form protective immunity. In the 1880s, Louis Pasteur began his studies on immunizing against anthrax, chicken cholera, and, later, rabies. Koch hoped to develop an effective vaccine from an extract of the protein coat of the tuberculin organism. In 1908, the French scientists Albert Calmette and Camille Guerin grew Koch’s organism in a variety of media in an attempt to decrease the organism’s virulence. This lead to the now famous vaccine called BCG. Since its introduction in 1921, more than two billion doses of BCG have been delivered worldwide. BCG is thought to prevent the development of miliary and meningeal tuberculosis; it has not been shown to decrease the risk of pulmonary tuberculosis. Search for an effective tuberculosis vaccine remains one of the top priorities of public health organizations.
Surgical therapy
Before drug therapy, surgical treatment of tuberculosis was common and often life saving. It has dramatically declined, but has experienced a limited resurgence. Its rationale came from an observation by Dr. James Carson, a Scottish physician (1821), who noted clinical improvement in patients who had a pleural effusion. In 1892, the Italian physician Carlo Forlanini introduced nitrogen into the pleural space based on an observation that pneumothorax led to a decline in death. Various techniques evolved, all with the aim of decreasing the expansion of the affected lung. They included compression of the upper ribs, thoracotomy, phrenic nerve crush to immobilize the diaphragm, and even the injection of air, silica, and ping pong balls into the pleural space. The compression of the lung caused scarring and was eventually replaced by the more easily delivered and effective antibiotic therapy.
Antibiotics
Effective antibiotic therapy began in 1944 with the discovery of streptomycin. It led to clinical improvement but also to the development of antibacterial resistance, which even now remains a major problem. Better results followed the development of PAS (para-aminosalicyclic acid), the first oral agent. The introduction of INH (isoniazid) in the early 1950s ushered in the modern era of effective chemotherapy. Modern antituberculosis therapy now always requires the use of multiple drugs – with INH and rifampin as the foundation of treatment for sensitive infections. Currently, there are fewer than 20 agents with activity against mycobacterium. Many newer drugs are in the pipeline, and a safe, inexpensive, and effective agent would be a truly important discovery.
Decline and resurgence
The decline of tuberculosis over the last 150 years preceded what many consider to be the era of modern medicine. The diminished transmission was felt to be due to improved housing, lower population density, isolation of sick individuals in sanitaria, and improved nutrition. Even prior to the use of isoniazid in 1954, there was a consistent and steady decline in the incidence of the disease. Effective treatment and improved public health resulted in decades of improvement, as the infection was identified and patients were diagnosed, isolated, given effective treatment, often free of charge, and closely monitored. Tuberculosis hospitals were closed and treatment moved from the hospital to the clinic. But in 1985 this steady decline was abruptly halted, and the number of new TB cases began to increase, in the U.S. and throughout the world, at an astonishing level.
Scientific discoveries
It is important to remember that over the last 50 years there has been continued scientific progress in the treatment of tuberculosis. Its natural history and complications are now well understood, and diagnosis is made with a high degree of specificity, including the ability to separate non-pathogenic mycobacterium from aggressively resistant strains. Not only has the organism been isolated and identified, its genome has been analyzed and sequenced. DNA fingerprinting techniques have enabled us to distinguish different strains of mycobacterium and track outbreaks, and we have learned a great deal about the pharmacokinetics of drugs used to treat tuberculosis. This molecular epidemiology, tracking the spread of organisms through populations, is the culmination of centuries of scientific progress. Yet science has not cured this infection; now as ever, TB is a social disease.
Social dimensions
While clearly an infectious disease, tuberculosis is also a social disease. Social determinants have an important effect on the extent, severity, and prognosis of the infection. Beyond the infecting organism, an individual’s risk for tuberculosis and its sequelae are dependant on nutritional status, life circumstances, mental health, public health infrastructure, and personal health efficacy. Historically, this infection has always had a particular penchant for the debilitated, the old, the malnourished, the immigrant, and the incarcerated. While these social factors have always been important, the sinister synergy of TB and HIV/AIDS has led to an unparalleled catastrophe. HIV suppresses the immune system, allowing TB to bloom. Patients co-infected with both exhibit a more severe disease, more pulmonary infections, more resistant infections, and higher morbidity and mortality. There are small hot spots of tubercular strains resistant to all available drugs. In these cases, the fulminant infections are accompanied with a mortality rate worse than was seen in the seventeenth century. The social consequence is that TB and HIV have decimated the working infrastructure of entire countries and left in their wake an unprecedented number of orphans, many with HIV. The HIV epidemic has caused an explosion of tuberculosis, especially in Africa, Asia, and the former Soviet Union. The economic devastation left by the synergy of these infections is unfathomable.
The future
Public health measures remain critical in the fight against tuberculosis. The use of directly-observed therapy (DOT) – bringing medication to patients and watching them take it (advocated by Karel Styblo) – is now the standard of care throughout the world. The global commitment to TB elimination is demonstrated by the development of public and private partnerships such as the World Health Organization and the Stop TB Partnership. The stated goal is to reduce the worldwide burden by 50% relative to 1990 levels, with a goal of eliminating it in the next 40 years. It will take unwavering international will and a huge global financial commitment, but without it, the consequences would be more dire than they are now.
The history of tuberculosis teaches us many lessons. Of these the most important is that science can improve our lives in innumerable ways, but cannot cure our social ills. The continued presence of tuberculosis is a reminder that we must guard against the social factors that create an environment in which this disease thrives. TB may be forgotten by many of us unaffected by its ravages, but it is not gone. It will continue until we no longer need to be reminded of our role in its perpetuation.
Bibliography
- Bates JH, Stead WW. The history of tuberculosis as a global epidemic. Med Clin North Am. 1993 Nov;77(6):1205-17.
- Centers for Disease Control and Prevention (CDC). Extensively drug-resistant tuberculosis–United States,1993-2006. MMWR Morb Mortal Wkly Rep. 2007 Mar 23;56(11):250-3.
- Chung KT, Biggers CJ. Albert Lleon Charles Calmette (1863-1933) and the antituberculous BCG vaccination. Perspect Biol Med. 2001 Summer;44(3):379-89.
- Colditz GA, Brewer TF, Berkey CS, Wilson ME, Burdick E, Fineberg HV, et al. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA. 1994 Mar 2;271(9):698-702.
- Daniel TM. The impact of tuberculosis on civilization. Infect Dis Clin North Am. 2004 Mar;18(1):157-65.
- Daniel TM. Captain of death : The story of tuberculosis. Rochester, NY, USA: University of Rochester Press; 1997.
- Goldman RC, Plumley KV, Laughon BE. The evolution of extensively drug resistant tuberculosis (XDR-TB): History, status and issues for global control. Infect Disord Drug Targets. 2007 Jun;7(2):73-91.
- Grzybowski S, Allen EA. History and importance of scrofula. Lancet. 1995 Dec 2;346(8988):1472-4.
- Lerner BH. Contagion and confinement : Controlling tuberculosis along the skid road. Baltimore, Md.: Johns Hopkins University Press; 1998.
- Reichman LB, Tanne JH. Timebomb : The global epidemic of multi-drug-resistant tuberculosis. New York: McGraw-Hill; 2002.
- Rom WN, Garay SM. Tuberculosis. 1st ed. Boston, Mass.: Little, Brown; 1995.
- Ryan F. The Forgotten Plague : How the battle against tuberculosis was won–and lost. 1st American ed. Boston: Little, Brown; 1993.
MINDY A. SCHWARTZ is an Associate Professor of Medicine in the Section of General Internal Medicine at the University of Chicago. In addition to her clinical practice, Dr. Schwartz is an accomplished educator and a member of the Academy of Distinguished Medical Educators at the University of Chicago, Pritzker School of Medicine. She teaches both nutrition and history of medicine to medical students and residents. Her innovative approach involves combining the use of historic content to improve clinical training. She is also the Arnold P. Gold Humanism chapter advisor for the Gold Humanism Honor Society at the Pritzker School of Medicine.
Highlighted in Frontispiece Volume 1, Issue 4 – Summer 2009

Leave a Reply