Philip R. Liebson
Chicago, Illinois, United States
In 1968 while I was a cardiology fellow at the New York Hospital-Cornell Medical Center, there was a buzz of excitement—Christiaan Barnard was coming to talk about his heart transplants! Our chief cardiovascular surgeon at the time was C. Walton Lillehei, no slouch of a surgeon himself, who had participated in the first open heart surgery at the University of Minnesota in 1952. The team was ready to emulate Dr. Barnard as soon as an appropriate patient and donor were available. In fact, over the next year there was a spate of heart transplants throughout the United States, until it was realized that this was not just another surgical procedure, but a complex process involving immunologic, sociologic, financial, and not least of all, logistical processes that almost defied description.
Where did the first heart transplant take place? In South Africa. Why South Africa, Cape Town to be specific, and why Christiaan Barnard? First of all, Cape Town was at that time as sophisticated in its medical standards as many centers in the United States and Europe. The Groote Schuur Hospital, where the first heart transplants were performed, was a center for well-equipped research laboratories and had a strong staff of full-time physicians who taught in the adjacent medical school while doing their research. Many of these physicians were accorded sponsorship to learn new techniques at the European medical centers. There was especially close cooperation between the cardiology service and cardiovascular surgery in promulgating state of the art interventions.
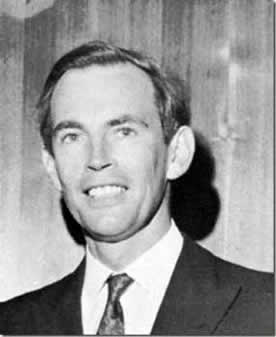
But who was Barnard? He had been head of the Department of Surgery since 1958, and he had the characteristics of a true surgeon: egocentric, brash, hardworking, and arrogant, according to at least one of his colleagues. However, it is just such a personality that leads to advances, especially in surgery. He once heard that a Russian surgeon had grafted a second head onto a dog, and he performed the same procedure, on a dog, of course, the first doubleheader outside of sports.
Christiaan Barnard was a native of South Africa, born in 1922, the son of a minister in the Dutch Reformed Church. One of his brothers died of a heart problem at age five. He obtained his medical degree at the University of Cape Town Medical School in 1945. In South Africa, as in Europe, the initial medical degree was an MB, and it took a dissertation similar to a PhD to get an MD after one’s name. His dissertation was based on the treatment of tuberculous meningitis, in 1953. So at age 31, he had not yet gotten involved in surgery, much less cardiovascular surgery.
Where did he go next? To the University of Minnesota on a two-year scholarship for cardiovascular surgical training under the sponsorship of Dr. Norman Shumway. No doubt, he also became acquainted with C. Walton Lillehei. The scholarship resulted in a thesis on aortic valve prostheses for which he obtained a Master of Science in Surgery. He continued to compile degrees, with a PhD for a dissertation on congenital intestinal atresia. He was indeed a Renaissance man in the area of general medicine.
Coming back to the Groote Schuur Hospital in 1958, he opened the Cardiovascular Surgical Department as its head. Over the next few years, as director of surgical research and head of the division of cardiovascular surgery at the University of Cape Town, he was very successful in the area of congenital heart disease. He also performed the first kidney transplant in South Africa in October, 1967. By that time he had transplanted hearts in at least 50 dogs. Certainly the path to heart transplantation was opened by the pioneering work of Norman Shumway, who had moved to Stanford and in fact performed the first heart transplant in the United States. Shumway continued to perform transplants successfully when the initial spate of transplants following Barnard’s initial success subsided because of poor results.
Finally, on December 3, 1967, Barnard performed the first heart transplant, incidentally assisted by his brother Marius. The operation involved 30 healthcare personnel and lasted nine hours. The donor heart came from a young woman who had been brain damaged after being hit by a vehicle while crossing a street in Cape Town. The recipient was a 54-year-old diabetic with end stage heart disease. The recipient lived for 18 days, dying of pneumonia after receiving immunosuppressive drugs.
His next heart transplant occurred almost a month later, on January 2, 1968, and the recipient, Dr. Philip Blaiberg, lived for 19 months. In 1971, another recipient lived for a record of 23 years. Over six years, Barnard performed 10 orthotopic heart transplants. Between 1975 and 1984, doctors in Cape Town performed 49 heterotopic heart transplants, a technique initially devised by Barnard.
Barnard toured the United States in 1968, resulting in the proliferation of cardiac transplants; most were unsuccessful, leading to a pause in the cardiac transplant program until the development of cyclosporine. In 1968 alone, 107 heart transplants were performed throughout the world. Unfortunately, matching of donors and recipients was poor and the management of rejection was primitive.
He retired in 1983 at 61 due to rheumatoid arthritis involving his hands and became a scientist-in-residence at the University of Oklahoma for several years. He established a foundation in Austria to help underprivileged children worldwide. A Renaissance man, indeed. He died in September 2001, a fateful month, at age 78.
Whenever South Africa is mentioned, the subject of apartheid comes up. Both Christiaan Barnard and his brother Marius were strongly anti-apartheid and Marius was elected to the legislature on an anti-apartheid platform.
The question arises, considering Norman Shumway’s pioneering work on animal transplants, why the initial human heart transplant did not occur in the US. The reason was ethical, the salient feature being the question of killing a person to donate a heart. Perhaps there were fewer questions of such ethical concerns in South Africa. There has been considerable controversy over the definition of brain death in the donor, leading to guidelines for evaluating this condition.
I will conclude this essay with a personal experience with a heart transplant recipient. I had been in the Navy in the early 60s as a medical officer on a destroyer squadron. In the early 90s I was making rounds in the Surgical Intensive Care Unit and came across a patient who had undergone a successful coronary artery bypass. He wore a navy cap and, when I indicated that I had been a naval medical officer on destroyers, he mentioned that he had been attached to one of our squadron destroyers at the same time. Whenever I saw him in cardiac clinic following his surgery we would salute each other with “Desron 7 arriving.” Eventually he underwent a heart transplant and lived a pleasant life for several years. We continued to salute each other during his clinic visits. It was my longest patient follow-up.
Some medical people thought that it was brash of Barnard to perform the first heart transplant when others had spent longer periods experimenting with animal transplants. However, this reminds me of a remark attributed to Will Rogers said in 1927 after the first successful transatlantic flight by a single person: “After this, they’ll all just be an imitation of Lindbergh.”
References
- Hoffenberg R. Christiaan Barnard: his first transplants and their impact on concepts of death. BMJ 2001; 323:22-29.
Heart transplantation. S Afr Ned J 1967:41; 1257-1278. - President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Guidelines for the determination of death. JAMA 1981;246:2184-2186.
PHILIP R. LIEBSON, MD, graduated from Columbia University and the State University of New York Downstate Medical Center. He received his cardiology training at Bellevue Hospital, New York and the New York Hospital Cornell Medical Center, where he also served as faculty for several years. A professor of medicine and preventive medicine, he has been on the faculty of Rush Medical College and Rush University Medical Center since 1972 and holds the McMullan-Eybel Chair of Excellence in Clinical Cardiology.
Highlighted in Frontispiece Volume 5, Issue 2 – Spring 2013