Philip R. Liebson
Chicago, Illinois, United States
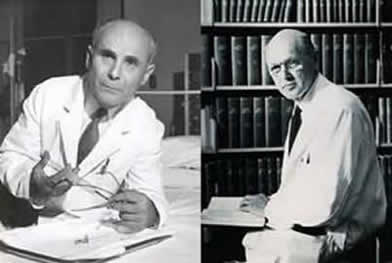
Right: Dickinson W. Richards, Jr. (1895–1973)
During World War I among the allied forces were an artillery lieutenant just out of college and a medical student who acted as an auxiliary battle surgeon because of the high mortality among battalion surgeons. They were, respectively, Dickinson W. Richards, Jr. (1895—1973) and Andre Cournand (1895—1988). Eventually they would pioneer development of cardiopulmonary physiology in Bellevue Hospital’s cardiopulmonary laboratory of the First Division at Columbia University in New York. Both had classical educations, Richards at Yale (where he excelled in Greek, the humanities, mathematics, and the natural sciences) and Cournand at the Lycée Condorcet in Paris (where he eventually withdrew to spend a year in private tutoring in philosophy).
After the War, Richards obtained his medical degree at the Columbia College of Physicians and Surgeons (P & S) in 1923, followed by his residency at Presbyterian Hospital. He spent a year of training with Sir Henry Dale at the National Institute of Medical Research, London, studying humoral agents for control of the circulation. Back at Columbia, Richards began studies on blood oxygenation and carbon dioxide elimination, evaluating blood flow through the pulmonary circulation by what was known as the indirect Fick method. For his research, he initiated a laboratory of pulmonary physiology at Bellevue Hospital.
It was to Richards’s laboratory at Bellevue that Cournand arrived in 1931 for further training in pulmonary medicine. After Cournand had obtained the Croix de Guerre with three bronze stars for his work in the trenches and no man’s land, he completed his medical degree in Paris and trained at the Hôpitaux Laënnec and Necker, spending his years in training in Paris. He was heavily involved in the social life there, especially in the French circle of Freudian analysis, with artistic circles including Yves Tanguy and Max Ernst and musical circles including Darius Milhaud and Edgar Varèse.
Richards was influenced by his classical training, especially the empiricism of ancient Greece and the Hippocratic emphasis on objectivity of experience. Cournand was influenced by the rational and humanistic morality of Descartes and Pascal and the research on circulatory physiology of Claude Bernard. In later years, Cournand would provide his fellows with Claude Bernard’s An Introduction to the Study of Experimental Medicine. After retirement, both Cournand and Richards continued intellectual pursuits at Columbia. He directed the program on the history of biomedical sciences at P & S. He edited the History of Circulation with Alfred P. Fishman, his Columbia colleague, and published essays on William Harvey and Hippocrates. Cournand introduced a medical course on the relationship between medicine and society. They both helped organize interdisciplinary projects at Columbia as members of the Institute for the Study of Science in Human Affairs.
For over three decades these humanistic physicians would develop techniques to study cardiopulmonary physiology and eventually share the Nobel Prize in Physiology or Medicine in 1956 with Werner Forssman, who had performed the first cardiac catheterization on himself. In the early 1930s, when the Cardiopulmonary Laboratory was established, the stethoscope, the electrocardiogram, and the pathology laboratory were the state of the art in cardiac investigations. Cournand and Richards’ early work in the 1930s involved the validation and improvement in use of the Fick technique. The indirect Fick technique involved measurement of carbon dioxide from a rebreathing bag and direct arterial carbon dioxide samples, both as substitutions for oxygen, with the assumption of equilibrium between carbon dioxide in the alveoli and the venous blood. It was felt at the time that mixed venous blood was dangerous and impractical to obtain. Carbon dioxide was substituted for oxygen in the equation: Pulmonary blood flow = O2 consumption/ arterial-mixed venous O2.
Their early investigations led to the estimation of the pulmonary vital capacity and end expiratory volume. This led to evaluation of respirators for the use of oxygen in high-altitude flights by the Air Force. They subsequently provided normal values for pulmonary function tests, studying abnormalities of alveolar-capillary block and, in general, the impact of pulmonary disease on respiratory gas exchange and arterial oxygenation.
In the late 1930s, they turned to direct cardiac investigation, beginning the use of cardiac catheterization in their cardiopulmonary physiology research. In 1929, they were stimulated by an intriguing article in an obscure German medical journal. The author, Werner Forssman, a general practitioner in a small town near Berlin, was interested in the effect of digitalis injected directly into the heart. Forssman had inserted a urological catheter through a dog’s leg vein into the right atrium. The dog survived, and Forssman was prevented from experimenting on a human, so he inserted a catheter in himself, with a surgical nurse assisting. This involved isolating his own antecubital vein, moving it into the chest, walking down two flights of stairs to the X-ray room, and guiding the catheter into the heart. There were no complications, but he did not follow up on his experiment. He joined the Nazi party in 1932 and was in the SS as a medical officer during World War II. There is no record of any further experiments.
While the Blitz was going on in London in late 1940, Richards and Cournand began to use catheters to evaluate venous blood on the right side of the heart in humans, after having spent four years demonstrating the safety and efficacy of catheterization of the right side of the heart in dogs and a chimpanzee.
At first, they used urology catheters and measured intravascular pressures with low-frequency water manometers. The indwelling Cournand needle was designed for serial measurement of arterial blood and blood pressure monitoring. During their early catheterization of patients, they would have cardiology fellows assist with the then-ungainly apparatus. In one instance, a postdoctoral fellow manipulated the fluoroscope to guide the catheter while his wife, also a post-doctoral fellow, lay under the table and manipulated the X-ray tube. Initially, catheters were inserted only into the right atrium, but in 1944 one of the catheters inadvertently advanced into the pulmonary artery. Cournand noted that there were no adverse effects and from then on pulmonary artery monitoring was initiated.
After World War II, Cournand helped design nylon catheters. By 1950s the cardiopulmonary laboratory staff produced publications on hemodynamic abnormalities in congenital heart disease, pulmonary heart disease, and the effects of digoxin in heart failure. Pressure transducers and other electronic equipment produced during the war effort allowed continuous pressure recording. Eventually, fiber optic techniques allowed detection of blood flow through cardiac and intravascular communications.
Further research in the laboratory involved the effects of acute hypoxia on vasoconstriction. Acetylcholine, a selective pulmonary vasodilator, was injected directly into the pulmonary artery in patients with chronic airway obstruction, to demonstrate a significant fall in pulmonary artery pressure resulting from vasoconstriction by hypoxia.
Over the ensuing years, Richards became director of the Columbia Medical Division of Bellevue Hospital but continued his collaboration with Cournand. As a cardiac fellow in the Second Division at Cornell in the mid 1960’s, I had the opportunity to watch procedures in the cardiopulmonary laboratory and attend conferences with Cournand. We would present a case to him with the patient lying on an examining table and he would ask the patient a few questions and spend the next 15 minutes auscultating the patient’s chest while we sat there in virtual absolute silence. Finally, he would pronounce his extended diagnostic and pathophysiologic assessment in his French-accented English. In those days before echocardiography, the stethoscope was still a state of the art instrument.
Cournand was short, stocky and physically vigorous. He would argue with some of his colleagues outside their offices on such subjects as the arts, politics, and sciences, in French and English. Richards allowed the house staff to use his office telephone and library, but had to lock his telephone when he discovered frequent calls to Paris, presumably by Cournand. At one of the Saturday morning conferences among the cardiopulmonary staff Cournand had been discussing a paper when a junior fellow remarked that his comments appeared paranoid. Cournand rose, ran down the table to the junior fellow, and remarked: “Correct! AND BY THE END OF YOUR FELLOWSHIP, DOCTOR, YOU WILL ALSO HAVE A YELLOW STREAK OF PARANOIA DOWN YOUR BACK EIGHTEEN INCHES WIDE.”
Cournand and Richards provided a rich and nourishing environment in the cardiopulmonary laboratory, cultivating a large and distinguished group of investigators that included Alfred Fishman, Yale Enson, William Briscoe, Richard Riley, Harry Fritts, M. Irenée Ferrer and Réjane Harvey among others. Despite Richards’ great efforts to foster modernization of the physical plant of Bellevue Hospital, the New York City Department of Hospitals decided to eliminate the Columbia and Cornell medical divisions in 1968 and the cardiopulmonary laboratory at Bellevue closed its doors forever.
References
- Enson Y, Chamberlin MD. Cournand and Richards and The Bellevue Hospital Cardiopulmonary Laboratory, Chapter 16, pp. 237-251, in Living Legacies at Columbia. De Bary T, ed. Columbia University Press, New York. 2006.
- Levin SM. The first cardiac catheter. J Vasc Surgery 2012. In Press.
Forssman-Falck R. Werner Forssman: A pioneer of cardiology. Am J Cardiol 1997;79:651-660. - Dickinson Woodruff Richards. Lancet 1 1973 (7805):732-733.
- Ventura HO. Dickinson Woodruff Richards and cardiac catheterization. Clinical Cardiology 2007; 30:420-421.
- Forssman W. [Probing of the right heart]. Klin Wochsenschr 1929;8:2085-2087.
PHILIP R. LIEBSON, MD, graduated from Columbia University and the State University of New York Downstate Medical Center. He received his cardiology training at Bellevue Hospital, New York and the New York Hospital Cornell Medical Center, where he also served as faculty for several years. A professor of medicine and preventive medicine, he has been on the faculty of Rush Medical College and Rush University Medical Center since 1972 and holds the McMullan-Eybel Chair of Excellence in Clinical Cardiology.
Highlighted in Frontispiece Volume 5, Issue 2 – Spring 2013

Leave a Reply