Anaeze C. Offodile II
Joel T. Katz
Boston, Massachusetts, United States
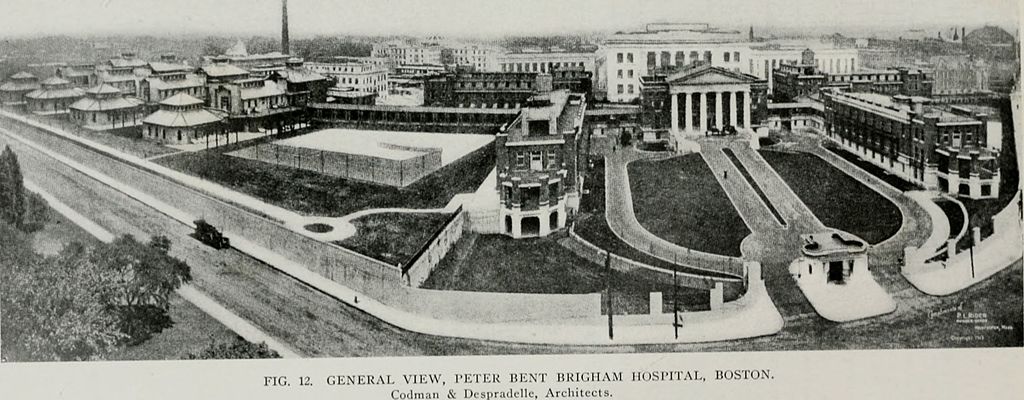
Before his death in 1877, Peter Bent Brigham, a prominent restaurateur, businessman and abolitionist in the Boston area, left a significant bequest for the creation of a hospital to provide care for the indigent and sick patients of Suffolk County.1 This would materialize several decades later when the 110-bed Peter Bent Brigham Hospital (PBBH) opened its door for the first time in 1913. It was by design located adjacent to the newly relocated Harvard Medical School (HMS) and in the process established for the first time an intellectual and physical association between a medical school and teaching hospital.2
This new hospital was largely patterned after the first modern academic medical center in the United States (US), the Johns Hopkins Hospital in Baltimore. However, the trustees of PBBH also sought to improve on the Hopkins prototype by rectifying one of its main limitations – establishing the first full-time academic model whereby the hospital could direct the educational and research activities by employing their own staff and controlling all academic appointments. Much like at Hopkins, the first Chairs (Harvey Cushing of Surgery, Henry Christian of Medicine and William Councilman of Pathology – nicknamed the “Three C’s”) represented a new breed of physicians bridging clinical excellence, innovation, investigation, and establishing the overarching goal of educating physician-leaders. They individually and collectively sought to bridge the wide nineteenth century chasm between science and medical practice, and thereby take advantage of the emerging links between physiology of health and disease that was already underway and celebrated in Europe – outside the vision of most Americans – by Lister, Koch, Pasteur, Roentgen, and others. Furthermore, Mr. Brigham’s explicit requirement to provide care for the “sick persons in indigent circumstances in the county of Suffolk” led the PBBH to move teaching away from elite private hospitals towards what many consider the key pillars of subsequent US academic teaching hospitals – research, teaching and charity care.
To lead the new hospital, these three chiefs were selected from a national pool to avoid the entrenched partisan battles so common at existing Boston hospitals. For the first time in the US, only full time physician staff were eligible for hire. Christian had to give up his lucrative private practice to become the first Chair; he also resigned as Dean of HMS, which he considered less prestigious and likely a stepping-stone to the Chair role. Councilman taught the entire Harvard pathology curriculum and senior students were granted plum inpatient and outpatient clerkship roles at PBBH, thereby improving the quality of students HMS could attract. By controlling all PBBH appointments, HMS could, for the first time, adhere to a carefully designed clinical curriculum and assure that faculty no longer viewed the trainees as a means to enhance their personal financial productivity. PBBH instituted a new and rigorous system of medical records documentation that set the stage for landmark clinical research. The PBBH School of Nursing (1912-1985) was an innovative and ambitious forerunner in professionalizing the field of nursing.
The first PBBH patient was Mary Agnes Turner, a 45-year-old woman admitted on January 22, 1913 for varicose vein surgery.2 Cushing made the symbolic first incision while David Cheever performed the successful operation. The most common admitting diagnosis in the first year of operation was syphilis (for Salvarsan therapy). Early house staff and faculty caring for these patients came to set the pace for innovation in American medicine during the early twentieth century. These included Cushing (Father of Neurosurgery who first described the now eponymous condition of pituitary basophilism), Elliot Cutler (performed the first mitral valve repair), Francis Weld Peabody (medical humanist), Soma Weiss (a pioneer in research bridging physiology and clinical outcomes), and Samuel Levine (the first American physician to diagnose premortem coronary thrombosis and a pioneer in the creation of treatment approaches for it). In very short order, innovation became the currency with which the PBBH interacted with the larger medical society. Accordingly, research was expected of the resident staff, who for the first time received appropriate credit for their contributions. Shortly after, other great institutions, such as Massachusetts General Hospital, followed suit.
In the succeeding decades, this ethos of scientific inquiry translated into many groundbreaking medical advances including but not limited to effective treatment for pernicious anemia (1926), the first use of an iron lung (“Drinker Respirator”) to save a polio victim (1929), the first artificial kidney in the US (1947), blood banking technology (1949), and the first successful solid organ transplantation (1954).3 Two of these were awarded Nobel Prizes in Physiology/Medicine in 1934 (pernicious anemia – George Minot and William Murphy) and 1990 (renal transplantation- Joseph Murray). PBBH cardiologist Bernard Lown, original developer of the direct current (DC) defibrillator, was the corecipient of the 1985 Nobel Peace Prize as founder of International Physicians for the Prevention of Nuclear War.
Clinically, the PBBH was also at the forefront of improving the quality of health care delivery in the US. Patient safety, anesthesia, intensive care, complex congenital and acquired heart disease, sepsis management were all championed at the PBBH. 2 This commitment became amplified with the entrance of the US into the two World Wars, as several prominent PBBH surgeons (Cushing in WW1 and Cutler, Francis Newton, and Carl Walter in WW2) treated wounded soldiers and in the process pioneered the understanding of fluid resuscitation, blood transfusions, peri-operative monitoring, and surgical repair of traumatic wounds. 2 Dr. Cutler, the Chairman of the Department of Surgery at the time, organized instructional courses for community surgeons who were about to be deployed. These sessions often proved to be the only advanced clinical instruction that these physicians received before taking care of injured soldiers at the war front. Additionally, Cutler was appointed the chief surgical consultant in the European theater in WW2 and helped devise the portable surgical hospital which is a forebear to the Mobile Army Surgery Hospital (MASH) unit used in the Korean War.2
The above accomplishments become more impressive knowing that PBBH from the start was always small, exceptionally poor, and under-resourced. On several occasions, due to poor financial planning and questionable administrative decisions, the institution barely escaped bankruptcy. From the 1950s onwards, the hospital leadership actively pursued opportunities that would alleviate its fiscal shortcomings. 2 The director of the Howard Hughes Medical Institute (HHMI) when it started in 1953 was PBBH Department of Medicine Chairman, Dr. George W. Thorn, who also was Mr. Hughes’s personal endocrinologist. HHMI payment for clinical research activities at PBBH went a long way towards the Hospital’s survival during lean times. In 1980, PBBH merged with two other great Boston medical institutions- the Robert Breck Brigham Hospital (focused on the “treatment of incurables,” i.e., rheumatologic conditions), and the Boston Hospital for Women, to form the Brigham and Women’s Hospital (BWH). 2-3
Today, BWH continues to uphold a legacy of clinical excellence closely tied to premier clinical training and research. BWH is the home of the Thrombolysis in Myocardial Infarction (TIMI) study group, the Nurses’ Health Study, and the Physicians Health Study, the Ariadne Labs, and the Division of Global Health Equity headed by Dr. Paul Farmer, among other innovative programs. The landmark 2008 JUPITER (Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin) trial, performed first total face transplant in the US (2011), and perennial inclusion in the U.S. News honor roll of America’s Best Hospitals serve as testaments to its position at the vanguard of medicine and patient care. 3 The BWH maintains close clinical and research ties to the adjacent Dana Farber Cancer Center, and, since 1994, has been, along with Massachusetts General Hospital, a principal member of Partners Healthcare.
References
- Shillito J, Black PM. The Harvard Neurosurgical Service at the Children’s Hospital Boston and Brigham & Women’s Hospital, 1912-2007. Neurosurgery. 2008; 63(3): 579-93
- Tilney N. A Perfectly Striking Departure: Surgeons and Surgery at the Peter Bent Brigham Hospital 1912-1980. 1st Ed. Sagamore Beach, MA. Science History Publications; 2006
- Tishler P, Wenc C, Loscalzo J (Eds). The Teaching Hospital: Brigham and the Evolution of Academic Medicine, 1913-2013. McGraw-Hill Press, New York, NY, 2014.
ANAEZE C. OFFODILE received his medical degree from Columbia University in New York. He is a 2013 graduate of the General Surgery Residency Program at Brigham and Women’s Hospital (BWH) and is currently pursuing additional training in Plastic & Reconstructive Surgery at Lahey Hospital and Medical Center, Burlington-MA.
JOEL T. KATZ graduated from John Hopkins Medical School and is the current Program Director of the Internal Medicine Residency at BWH. He also has dual appointments as an Associate Physician in the Divisions of Infectious Diseases and General Medicine, BWH. He is a 1994 graduate of the BWH Internal Medicine Residency.
Highlighted in Frontispiece Spring 2017 – Volume 8, Issue 4

Leave a Reply