Mary Pan
Seattle, Washington, United States
I hovered over the patient, looking at him for the first time. It was then I realized he was dead. Lifeless. Pallor without a hint of blush, tubes protruding out of each orifice. This realization stretched out beyond and before me. I was eager and horrified and mesmerized. I was a third-year medical student, and it was my first night on call.
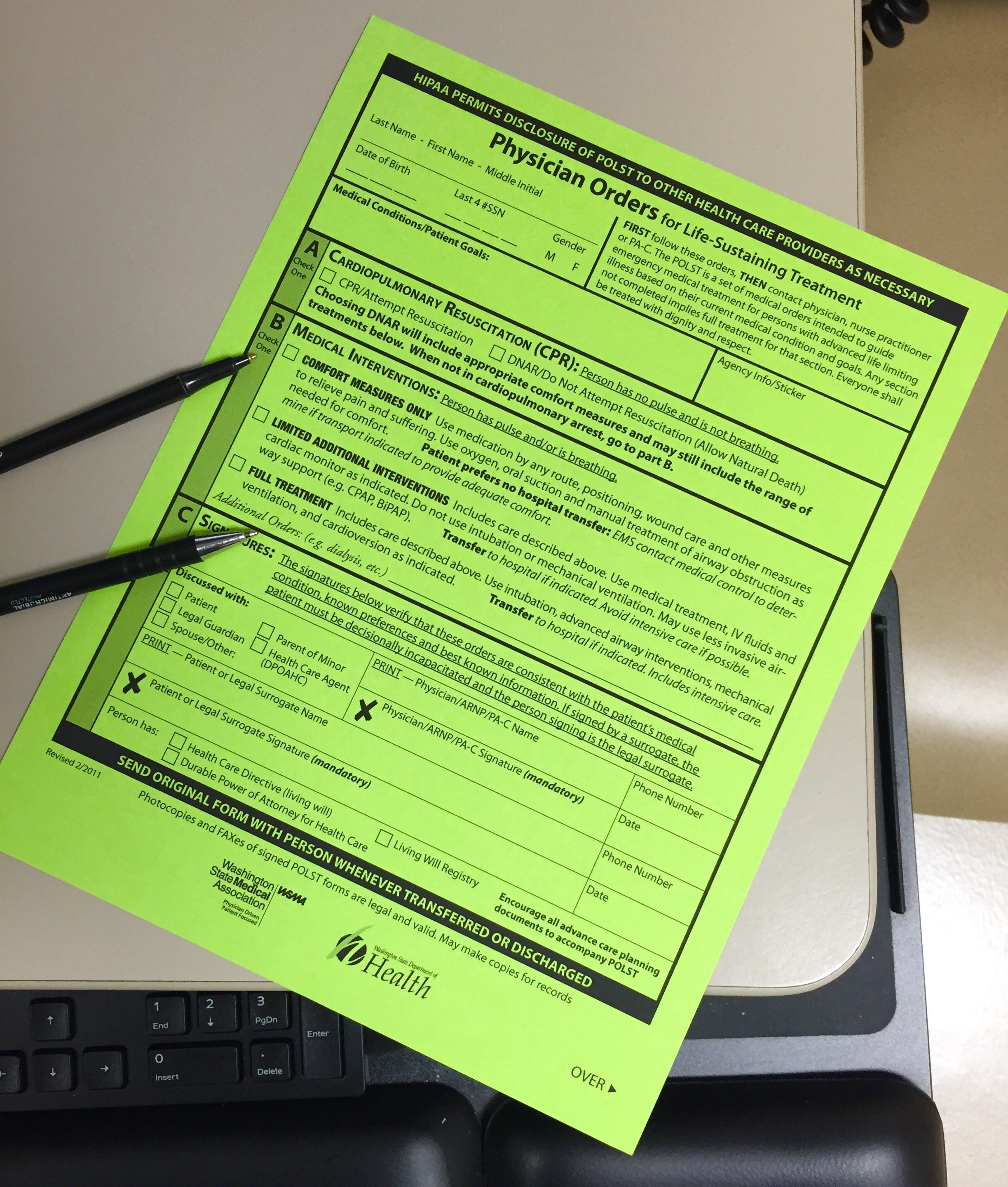
I pulled out the bright green form and a pen. We had already spent fifteen of this twenty minute elderly well care appointment discussing the patient’s chronic medical conditions and preventive care needs and had yet to get to the physical exam. Although they can be uncomfortable and lengthy, conversations about end-of-life choices are helpful for patients to consider their wishes. This patient was frail and elderly and hard of hearing. I found myself shouting the explanation of the form in my hand, alternating my gaze between her and her attentive daughter.
In that interminable moment, as I gazed at the pallid body, I was transported to my first year of medical school, where I dissected a formaldehyde-soaked cadaver. Pushing, prodding, poking. Searching out the muscle groups, the blood vessels, the nerves, tracing their origin to their destination. Deciphering how all worked in concert to orchestrate movement and digestion and breathing. Pushing, prodding, poking some more.
“Have you seen this form before?” I held up the neon green cardstock. “It’s called a POLST form—Physician Orders for Life-Sustaining Treatment. It gives your caregivers information about your wishes if something were to happen and you could no longer speak for yourself. We’ll talk about it today and then you’ll put the original on your fridge at home. We’ll keep a copy here for our records.” The POLST, developed in Oregon in 1991 and now in use, in various forms, in 43 states, addresses a gap in end-of-life care planning. It is a simple one-page directive to help guide medical treatment if a patient were to stop breathing or not have a pulse. Despite the fact that this type of form can be helpful in advising medical providers, caregivers, and loved ones, most adults don’t have any advance directive indicating their wishes for end-of-life care.
I stared at the patient’s body, splayed out before me in the ICU. It demanded reverence and action. The code team was called, intercom echoing overhead, despite the obvious fact that all that was left was a body. Lack of pulse, the absence of breathing . . . these were the least of what made him dead. He, whoever he was, was no longer present. Even I, a novice in medicine and life, could see that.
The patient had mild dementia but nodded in understanding. Her daughter repeated what I was saying, just in case the woman was nodding in agreement just to appease us. I was grateful a family member was present. Often, even when these decisions are made ahead of time, families—or a hospital or medical team—have a hard time adhering to the patient’s decision. There may be disagreements among loved ones about what the patient wanted. There may be unrealistic expectations about the likelihood of resuscitation or quality of life thereafter. In our culture we hold on, we push through; we pull ourselves up. We don’t talk about death or dying. Most of us don’t see death or dying up close and therefore don’t have the context to understand what these decisions might mean.
I throw myself into the chest compressions, feeling the unnatural cracking and resistance from the large sternum. I focus my efforts on his chest, avoid looking at his face. I am mechanical, self-conscious and quietly horrified as I pound on pale flesh, almost transparent under the fluorescent lights of the ICU. The patient’s room is overflowing with dozens of people, carefully orchestrated chaos. The internist on call is now in command. His voice seems to echo from far away, as if through a tunnel, as I pound methodically. Pushing, prodding, poking. Did we get a blood gas? When was the last dose of epinephrine? Give more atropine. It has now been twenty-five minutes since we first watched the patient’s blood pressure drop into nothingness.
I turned to my elderly clinic patient. “The first question asks about what to do if your heart were to stop beating and you were not breathing. Would you want attempted CPR—cardiopulmonary resuscitation, including chest compressions, or allow a natural death?”
The internist looks around at everyone. “Any ideas?” Silence. The pattern of chest compressions and bagging—forcing air from a bag into the patient’s lungs—rhythmically repeats. The internist realizes we have exhausted the checklist. We have tried everything: pushing, prodding, poking this body in an attempt to will it back to life. We failed. “Does anyone have any objections to pulling this?” No one objects. I expect him to pronounce the patient dead. But then I see him, this confident physician, hesitate. What if something was missed?
Incredulous, the patient stared at me, then glanced at her daughter, puzzled. “Wouldn’t I want everything possible to be done? Why would anyone ever choose not to have everything done?” It’s an excellent question. One most of us would ask if we’d never encountered an actual attempt at resuscitation. We believe what we see on television: a couple of rescue breaths, thirty seconds of chest compressions and the person is alive! Able to talk and walk right away.
Insecurity is heightened by the unknown. This self-doubt leads to more being done, even when unwarranted. Everyone’s eyes are fixed on the patient’s cardiopulmonary monitor. Suddenly the physician running the code orders another dose of epinephrine. I look down at the patient, this time at his face. It’s blue; just a whisper of robin’s egg, like a late winter sky. His body is stark white. He is still dead. And yet, we go on.
I mark the “Attempt Resuscitation” box on the bright green form and move on to the physical exam. I wish I had more time. I want to lean in and have a real conversation. I want to make sure she understands the possible repercussions of trying to bring her back to life. The broken ribs, the tubes—endless tubes—in natural and manufactured orifices, the mechanical sound of the machine that she will be hooked up to—the whir and click that will echo through the sterile halls of the ICU in the empty night, the ravaging of a body that maybe—even likely—just needs to rest. I want to give her the perspective of that young medical student hovering over the clearly dead body. I want to tell her, to show her, it’s okay to say no. Do Not Attempt Resuscitation. In a way, maybe in the most profound way, this is saying yes. Yes, it’s okay for me to go. Yes, it’s okay to let me go.
MARY PAN is a family medicine physician with postgraduate training in global health, bioethics, and narrative medicine. She received her MD degree from the University of Washington and her Diploma in Tropical Medicine and Hygiene from the London School of Hygiene and Tropical Medicine. She practices family medicine in Seattle, Washington.

Leave a Reply