Clemens Schmitt
Berlin, Germany
Sensing the first symptoms and signs of a potentially serious development, diagnosing a manifest malignant state, and determining the adequate treatment in order to eradicate the disease at its roots and ultimately eliminate “the last evil cell“—that is what cancer medicine is all about.1 It resembles in some ways the strategy required in diplomacy and politics when faced with terrorism of a novel dimension—infiltrate and overpower established borders of existing territories that are sprouting dangerously like a parasite by abusing the rules of normal growth and interaction. These areas are a brood characterized by its everything-else-destroying nature as well as its invasive and globally spreading attitude. Cancer or terror? Can we learn how to treat terrorism from cancer medicine?
Early detection, when the evolving danger could have been securely removed in toto by a limited surgical operation, is rare. Prodromi, more subtle signs of a rising threat, are also too easily neglected, limiting the chances of a later successful intervention. Moreover, after the bad news has eventually been communicated, there is often a moment of shock, desperation and misbelief, further delaying needed action.
As a next step following diagnosis, staging examinations are required to detect potential satellite spread. The presence of metastases not only would translate into a worse prognosis but also guide treatment decisions. Not even “radical” surgery will help the patient with metastases, because numerous remote satellites cannot be resected in curative intent. After careful consideration, single metastases may be selected for surgical intervention if they impose a particular danger to the organ they have conquered or cause local complications, can be extirpated with a high likelihood of no malignant structures remaining, and if there are only a few of those focal lesions. Otherwise, operations intended to fight multiple sites are not justified.
Sometimes one decides to combine local resection with rays, delivered either from an internal source or externally applied with the guidance of a remote-controlled precision targeting device. Strikes launched from a distance, reminiscent of drone or missile attacks, become a tactical alternative particularly when local operations appear inadequate. Of note, some collateral damage will be unavoidable, and complete cure is unfortunately no longer an option at this point.
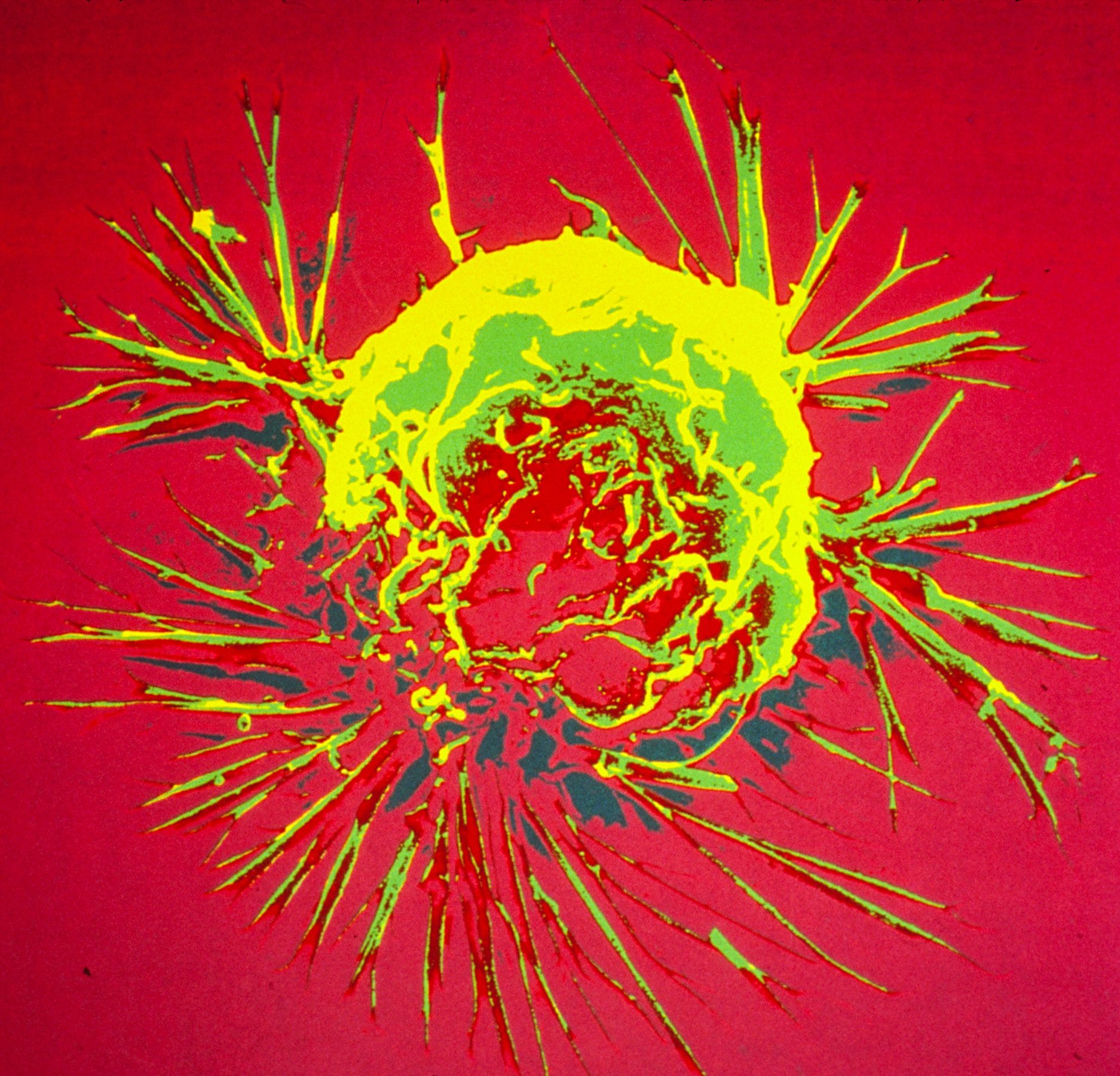
An additional problem is the occult dissemination of just a few or even single cancerous cells flying below the “radar” of the initial imaging surveillance diagnostics. Those cells may remain silent for long periods of time, and are in this hibernation-like condition largely unsusceptible to any kind of treatment. Certain yet-to-be-decoded stimuli will wake up these “sleepers,” allowing them to expand, unveil their malignant potential, and often literally explode. The rules of malignant spreading, of infiltrative growth at remote sites, are only partially understood. Which routes will the primary cellular sources of the satellite manifestations take to ultimately enter foreign territories and distant organs? Do they need to overcome barriers or do they settle down where border control is less sophisticated and therefore, frontiers particularly permissive? That spread-out cells manage to grow in hostile terrain, actually under “inadequate culture conditions,” was already hypothesized back in 1889, when the English surgeon and oncologist Stephen Paget formulated his “seed and soil” hypothesis, arguing that it takes both the aggressive seed, the radical elements, and the nurturing soil (the surrounding social milieu) to allow the intruder to successfully implant and expand.2 If the ground has been paved and if growth-promoting niches for the de-rooted but potentially extremely dangerous cells have been formed, satellite sites will flourish and may eventually themselves become the origin of further dissemination elsewhere.
Systemic treatment is the approach of choice against a globally disseminated disease. Chemotherapeutic agents, classic anti-cancer poisons, work in principle even at advanced stages. They typically force the lesions to regress, sometimes even to vanish, albeit with substantial side effects: weakened body-wide defense, susceptibility to infection, reduced regenerative capacity of the whole organism, lasting fatigue and limited physical and cognitive performance, and even secondary malignancies. While the most rapidly expanding cells will be hit most effectively, “sleeping” micrometastases, and “cancer stem cells” often escape. Resistance will rather quickly and invariably emerge, putting the malignant forces back in the league. Alternative strategies, a “Plan B” is needed: a second-line therapy, which may again achieve some control, a limited response but typically followed by the next relapse and finally without any significant efficacy. Eventually the malignant sites dominate, interfere with life-essential organ functions and eventually drive them to extinction.
In the upcoming era of the so-called “precision medicine” it is the goal to understand the blueprint, the building principle, of a malignant process like a profiler would characterize the personality of an unknown opponent—to identify a leading characteristic, often simultaneously a weakness or vulnerability. Such “targeted therapies” come with enormous hopes and expectations but are rarely lastingly effective. Often, they evoke impressive but short-lived responses, because malignancies quickly learn how to get around them and change their molecular face, developing bypassing or evading strategies to expand and metastasize further. Tumors are equipped to rapidly become resistant, being highly mutable and their composition more heterogeneous than one might have thought on first sight. An assembly of many small subunits that appear to be similar, but continuously gain additional and different capabilities that equips them to withstand anti-cancer treatment measurements. Thus, targeted therapies may effectively eliminate many of these subunits, but fail to eradicate the tumor in its entirety, miss the “last cell”, because some resistant subclones are very likely to re-emerge.
The newest hope consists of the discoveries and developments made in immune oncology – to direct components of the immune system against the malignant elements wherever they may hide, or to unleash the power of a blunted anti-tumor immunity to effectively attack cancer structures. Ironically, it is the very same defense system that initially failed to neutralize the budding malignant growth and to eliminate it like a foreign intruder. Tumors are smart and not easy to catch; they even actively induce tolerance. But this is exactly what cancer medicine, specifically immune oncology, has now managed to convert into a sharp weapon: to reactivate a specific anti-tumor defense that was repressed via subversive communication tools and misled check-point control at the interface between malignant cells and the host immune cells. This may work even better if the cancer cells are highly aberrant due to many mutational alterations particularly visible to the immune system. It is an anti-cancer treatment that utilizes the patient’s own forces to strike back, to release the systems-wide blockade that so far had precluded the immune machinery from exerting its systems-wide lethal action. Albeit for the price that defense activity gets globally enhanced, thereby accepting surveillance intelligence to observe and potentially attack normal cell elements as well.
In 1971 former US president Richard Nixon declared “war on cancer.”3 Now, almost half a century later, the enemy is still around, more viable than ever, far from being defeated. Epidemiological studies continue to remind us that changes in our lifestyle may effectively prevent cancer; yet many malignant clones arise regardless of our preventive nutritive and social efforts. Terrorism is a rapidly expanding threat of highest malignant potential which has deeply infiltrated our society and metastasized at many sites therein. The roots of evil are deep. To dry out the soil that nourishes the seed and feeds the roots will take a therapy different from conventional strategies of the past, a novel therapy that we do not as yet readily hold in our hands. But we have promising ideas, thought-differently concepts. It is on us to develop those further, to make them more effective against the most serious challenges to life and humanity.
References
- VT DeVita, S Hellman, SA Rosenberg. 2001. Cancer: principles and practice of oncology. Lippincott Williams & Wilkins.
- S Paget. 1889. The distribution of secondary growths in cancer of the breast. The Lancet, 1(3421):565-614.
- R Nixon. 1971. Statement about the National Cancer Act of 1971. The American Presidency Project (http://www.presidency.ucsb.edu/ws/?pid=3276).
- C von Clausewitz. 1874. On war. Project Gutenberg, 2006 (http://www.gutenberg.org/ebooks/1946).
CLEMENS A. SCHMITT is a Professor of Medicine, Vice Director and Chief Executive Clinician at the Medical Department of Hematology, Oncology and Tumor Immunology at the Charité – University Medical Center in Berlin. He is also the Director of the “Berlin School of Integrative Oncology (BSIO)”, an inter- and transdisciplinary graduate school funded within the German “Excellence Initiative” that trains young natural scientists and research-experienced physician scientists to experimentally address the most pressing challenges in clinical cancer care and related fields. His research interests are based on the view that common principles and rules underlie distinct cancer types, and can be therapeutically exploited in a systems-medicine way.