Bonnie Salomon
Illinois, United States
It is a conceit of many a reader to interpret poetry as it affects their daily life. It certainly is a fancy of this reader, pouring over Emily Dickinson’s poems as a literary respite. While teaching a medical ethics course at a local college this past autumn, I stumbled onto several Dickinson poems that reverberate with the concerns and challenges of contemporary medical ethics. Certainly, Dickinson was not specifically concerned with the issues of palliative care, end-of-life dilemmas, or truth-telling in medicine. While the poet did not intentionally explore concepts of medical ethics, selected Dickinson poems might still enlighten medical ethics discussions. Dickinson’s poetry gives context and form to clinical scenarios that are ethically challenging and morally ambiguous. Poetry sometimes rolls up its sleeves and comes to work with us. In this case, Dickinson dons a lab coat, following me as I confront issues at the bedside. Her language is truly richer than anything found in a philosophical tract. It is a conceit to read Dickinson as a medical ethicist, but it is a conceit I find valuable.
End-of-life issues
THE HEART asks pleasure first,
And then, excuse from pain;
And then, those little anodynes
That deaden suffering;
And then, to go to sleep;
And then, if it should be
The will of its Inquisitor,
The liberty to die.
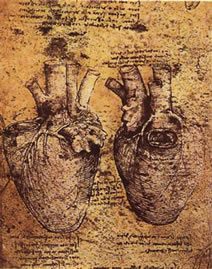
Leonardo da Vinci (1452–1519)
This poem, in astonishing detail, precisely describes the issues in end-of-life care. Dickinson follows the psychological steps taken during treatment of a terminal illness. Initially, all of us pursue happiness, usually when we are strong, healthy, and young. Asking pleasure first, the heart—as disease and disability eventually creep into life—later seeks “an excuse from pain,” ultimately culminating in a desire for that which will “deaden suffering.” From chasing pleasure, we descend gradually into pain and suffering, requesting only relief. When the pain becomes intolerable, the heart asks “to go to sleep,” a peaceful death, free of pain. If it should be the will of the inquisitor, the individual who is suffering, then all that is asked is the “liberty to die.” Note Dickinson’s use of the word “inquisitor.” She does not use a more traditional word, such as patient, person, or victim. The sufferer is an inquisitor, asking for relief, asking for answers, asking for a solution. What the inquisitor asks for, ultimately, is the striking idea: “the liberty to die.” Here, Dickinson makes death out to be a kind of right, a freedom from relentless pain: it is liberating. Moreover, like other liberties, it should be free from the interventions of others.
By now, any physician dealing with end-of-life issues should appreciate the beauty of such insights. The poem follows the clinical course of any patient suffering from an incurable malady. “The liberty to die” is a phrase that could have been used in multiple end-of-life cases, such as with Dr. Timothy Quill’s patient, Diane. As chronicled in his famous New England Journal of Medicine article, Diane, suffering from incurable leukemia, asks Quill to provide her with a supply of barbiturates, intending on physician-assisted suicide. This invocation of “the liberty to die” has been used by multiple patients requesting assistance from their physicians to accelerate their almost certain death (see Oregon’s Death with Dignity Act). This liberty is also echoed in the requests for hospice care, palliative care, and other forms of assistance for those faced with the need to “deaden suffering.”
The value of this poem for physicians lies in its gentle, yet logical, depiction of disease. Written from the viewpoint of the afflicted, its words force us to hear the inquisitor. No matter what philosophical view physicians might have on physician-assisted suicide or end-of-life care, Dickinson eloquently addresses the essential human need to deaden suffering. This poem does not end the discussion about how to care for the terminally ill—it begins it, with a compassionate and universal voice.
Palliative care and pain control
PAIN has an element of blank;
It cannot recollect
When it began, or if there were
A day when it was not.
It has no future but itself,
Its infinite realms contain
Its past, enlightened to perceive
New periods of pain.

Daguerreotype
This poem serves as a reminder of the difficulty in treating others’ pain. For patients with chronic, intractable pain syndromes, their lives are enveloped by their suffering. All too often, physicians turn a deaf ear, perhaps out of frustration or perhaps because treatments are often ineffective. What Dickinson does in this poem is startling. She gives pain a biography, or, better put, an anti-biography. She explains that pain (note “Pain” with a capital “P,” giving it the respect of a proper noun) cannot recollect its beginning, or if it had a beginning. Pain has neither a future nor an end; its realms are “infinite.” Portraying pain’s utter sense of hopelessness, she concludes with the foreboding observation that pain is “enlightened to perceive/New periods—of Pain.”
One of a physician’s major roles is the alleviation of pain, whether by medication, surgery, therapy, etc. Patients come to us, in pain, looking for relief. Although physicians can palpate or auscultate organs, we often cannot appreciate our patients’ pain. It is not measured or quantified objectively, like a blood pressure or a serum glucose. Pain is the ultimate subjective experience, as it were. As Elaine Scarry noted in The Body in Pain, pain “comes unsharably into our midst at once that which cannot be denied and that which cannot be confirmed” (pg. 4). This agonizing phantom, present yet unconfirmed, causes a gap between patient and physician.
For a physician to practice ethically and responsibly, a patient’s pain must be addressed, regardless of circumstance. Yet, many articles in recent medical literature have detailed what is described as “oligoanalgesia,” the lack of sufficient pain control. What is most distressing is the data showing certain cultural or ethnic biases in pain control. Several studies by Hoffman (1993) depicted inadequate pain medication for Hispanic patients with long leg fractures. It is crucial for physicians to recognize pain—as Dickinson did—as “Pain,” an all-encompassing agony for the body. It has no beginning, and seemingly no end, to the sufferer. It is the physician who must provide hope that there can be such an end, or at least improvement (the principle of beneficence guides such actions). What Dickinson provides in her poem is a sense of intimacy with pain, and by extension, an understanding of its pathology.
Truth-telling
TELL ALL the Truth but tell it slant—
Success in Circuit lies
Too bright for our infirm Delight
The Truth’s superb surprise
As Lightning to the Children eased
With explanation kind
The Truth must dazzle gradually
Or every man be blind—
In the United States, the emphasis on patient autonomy has led to an unshakable belief in telling the truth to patients. No longer using the cloak of paternalism, physicians now are telling patients the truth about diagnosis and prognosis in manners that were unheard of in earlier generations. As a sign of respect for the individual, doctors are expected to reveal what they know when they know it. Our society, for the most part, disdains the withholding of medical information. However, the art of medicine also includes the art of communication. The way information is shared is critical for any ethical interaction. As ethicist Howard Brody put it: “it is not enough to teach in an ethics course that the physician ought to tell the truth, for instance, to a patient recently diagnosed with a possibly terminal cancer. It is also necessary to teach aspiring physicians how to tell the patient this information” (Veatch, pg. 87).
Dickinson’s perspective on truth-telling correlates beautifully with contemporary medical ethical thought on the subject. She writes to “Tell all the truth,” advising not to withhold the truth, or segment it, but to tell all. But she also wisely advises “tell it slant,” a clever but ultimately compassionate method. Dickinson acknowledges that all the truth, told in one fell swoop, may be overwhelming (“Or every man be blind”). She gives the example of explaining lightening to children, “eased/With explanation kind.” Here, the virtue of kindness cannot be overemphasized. Telling all the truth, quickly and without subtlety, can be an act of cruelty. How many times have physicians blurted out a diagnosis or prognosis, without any careful measuring of their words? How many patients have heard words such as “You have a malignant tumor” or “He’s dead” told with heartless candor?
Dickinson suggests a better way to reveal what is known. “The Truth,” as she writes, “must dazzle gradually.” She unknowingly echoes Robert Buckman’s suggested six-step strategy for breaking bad news. In his 1992 book, Breaking Bad News, Dr. Buckman suggests a stepwise approach to breaking bad news, respectful of the patient’s willingness to know the truth. It is a gradual approach, very close to what Dickinson’s poem advises. The process emphasizes sensitivity to the patient—what they want to know and how to respond to their reactions.
When a doctor approaches a patient with bad news, it might be wise to recall Dickinson’s words. To tell the truth “slant” is not to lie, withhold information, disrespect the patient, or act paternalistic. To tell the truth “slant” is a method based on compassion—incorporating principles of patient autonomy, beneficence, and non-maleficence.
References
- Buckman, R. (1992). How to break bad news. Baltimore: The Johns Hopkins University Press.
- Dickinson, Emily. (2000). The complete poems. Part one: life, IX. Bartleby.com. Retrieved from: http://www.bartleby.com/113/1009.html.
- Dickinson, Emily. (2000). The complete poems. Part one: life, XIX. Bartleby.com. Retrieved from: http://www.bartleby.com/113/1019.html.
- Dickinson, Emily. (2003). Tell all the truth. Poemhunter.com. Retrieved from: http://www.poemhunter.com/poem/tell-all-the-truth/.
- Quill, T. E. (1991). Death and dignity—a case of individualized decision making. New England Journal of Medicine, 324, 691-694.
- Scarry, E. (1985). The body in pain. New York: Oxford University Press.
- Todd, K. H., Samaroo, N, & Hoffman, J. R. (1993). Ethnicity and emergency department analgesia. Journal of the American Medical Association, 269, 1537-1539.
- Veatch, R. M. (1997). Medical ethics, 2nd edition. Sudbury, Massachussetts: Jones and Burtlett Publishers.
Related article
Emily Dickinson’s mystifying in-sight
BONNIE SALOMON, MD, is an emergency physician in the Chicago area. She completed a fellowship in medical ethics at the University of Chicago and currently teaches medical ethics to undergraduates at Lake Forest College. Her poems and essays have appeared in both medical and public publications, including the Chicago Tribune and Annals of Internal Medicine.
Highlighted in Frontispiece Volume 4, Issue 3 – Summer 2012

Leave a Reply