George Dunea
James L. Franklin
Chicago, Illinois, United States

Crop of image by Jeff Kubina on Flickr via Wikimedia. CC BY-SA 2.0.
In 1806, Philipp Bozzini of Mainz invented an instrument designed to explore the interior of the human body that he called the “Lichtleiter” (light conductor). It had a candle or an oil lamp as a source of light, and he used it to look at the ears, nose, larynx, urethra, rectum, female bladder, and cervix, but it never gained wide acceptance. In 1826, the Parisian urologist Pierre Salomon Segalas added to the device two candles, a lens, and a conical mirror and was thus able to look inside the bladder. He is sometimes called the “co-inventor” of endoscopy.
In 1827, John Fisher of Boston invented a tubular speculum also lit by candlelight and a system of mirrors. He was followed in 1853 by the French physician Antonin Jean Desormeaux, who improved these early open-tube endoscopes and was the first to use them on patients for procedures such as cauterization. In 1865, Sir Francis Richard Cruise of Dublin further improved the lighting by replacing the gasoline mix of an earlier design and using a mixture of petroleum and camphor. This gave a more powerful light but also too much heat.
The first gastroscopy has been attributed to Adolf Kussmaul (1868). Using a rigid device based on that of Desormeaux, he passed it down to the stomach of a sword swallower and repeated the procedure several times on his housekeeper. As the light was inadequate, he found it difficult to see much detail.
Kussmaul was followed in short order by Max Nitze and Joseph Leiter (1876), Johann von Mikulicz-Radecki (1881), and several others, including Michael Hoffmann, whose 1911 instrument had movable lenses and prisms. These early instruments were rigid cylindrical tubes, equipped with a light source but difficult to use. Around 1878, Thomas Edison invented the incandescent lamp, which was later incorporated into endoscopes and made candles and mirrors obsolete.
In 1922, Rudolf Schindler brought to the United States from Germany a gastroscope with a flexible shaft that had a series of prisms, allowing the operator to bend the tip of the instrument and examine the distal part of the stomach. It was manufactured by Wolf, a fabricator of medical instruments, and, by being flexible, revolutionized gastroscopy.
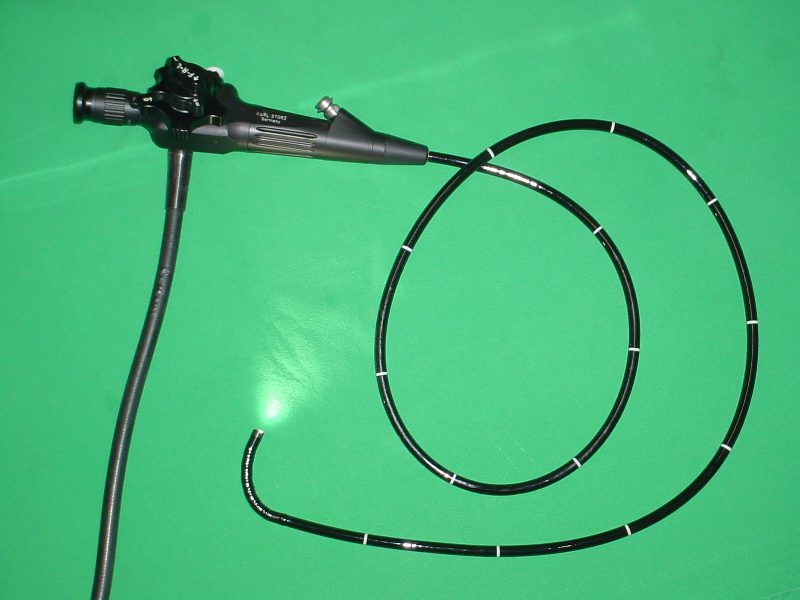
The first efforts to transmit images using flexible quartz fibers were made in the late 1920s. In 1954, Lawrence Hopkins built a flexible fiber imaging device, leading to the invention in 1958 of a flexible fiberoptic endoscope by Lawrence Curtiss, then a graduate student in physics, and Basil Hirschowitz, a South African trainee in gastroenterology. The advance that made it possible to extend the length of flexible glass fiber optic cables while still transmitting a cohesive image was coating each individual fiber with a glass of a different refractive index so as to prevent blurring the image.
During the six and a half decades since the advent of the fiber optic gastroscope, further advances have dramatically extended the scope of gastrointestinal endoscopy. Gastro-camera photography, first developed in Japan to screen for gastric cancer, was incorporated into the design of the first gastroscopes made by the Olympus Camera Company. Adding an instrument channel into the gastroscope allowed the examiner to take biopsies and cytologic samples of abnormal findings such as ulcers or tumors. The length of the fiber optic instrument was extended to reach the duodenum. It became possible to visualize with X-ray contrast media the ducts draining the pancreas and the bile ducts that drain the liver and to carry out invasive procedures such as sphincterotomy and extraction of bile duct stones. Therapeutic endoscopy evolved to techniques for controlling gastrointestinal bleeding by electrocautery, laser cautery, and the endoscopic placement of hemostatic clips. The injection of sclerosing agents into esophageal varices caused by cirrhosis of the liver has controlled the occurrence of gastrointestinal bleeding. Techniques for the percutaneous endoscopic placement of a gastric feeding tube into the stomach for extended feeding have obviated the need for invasive surgery. Mounting an ultrasonic endoscopic probe on the endoscope has allowed the detailed visualization of structures near the stomach and the duodenum such as the pancreas. The basic design of the fiberoptic gastroscope led to the development of the colonoscope. Colonoscopy was a great advance in that it allowed one to examine the entire colon and distal small intestine (the ilium). It became the standard diagnostic screening test for colon cancer. The evolution of targeted strategies for colon cancer screening and the removal of colon polyps has greatly reduced the mortality from colon cancer in the United States.
Further reading
- Chandrasekhara V, Khashab M, Elmunzer BJ, Raman V. Clinical Gastrointestinal Endoscopy, 3rd ed. Elsevier; 2019.
- Sivak MV. Gastrointestinal endoscopy: Past and future. Gut August 2006;55(8):1061.
- Sircus W. Milestones in the evolution of endoscopy: A short history. JR Coll Physicians Edinb 2003;33:124-34.
- Davis AB. Rudolf Schindler’s role in the development of gastroscopy. Bulletin of the History of Medicine March-April 1972;46:150.
GEORGE DUNEA, MD, Editor-in-Chief
JAMES L. FRANKLIN is a gastroenterologist and associate professor emeritus at Rush University Medical Center. He also serves on the editorial board of Hektoen International and as the president of Hektoen’s Society of Medical History & Humanities.

Leave a Reply