Göran Wettrell
Lund University, Sweden

Clarence Crafoord
Clarence Crafoord (1899–1984) was one of the most outstanding surgeons in Sweden during the twentieth century (Figure 1). He started his surgical training in the early 1920s. Postoperative complications such as obstructing pulmonary thrombosis were a frequent cause of death. In 1927, Crafoord performed two successful acute pulmonary embolectomies.1 However, because of the difficult nature of this operation, Crafoord focused on the use of purified heparin to prevent venous thromboembolism, as well as its use later in heart-lung machines. In the 1930s and 1940s, he pioneered the use of rhythmic mechanical positive-pressure ventilation during thoracic operations. The ventilator prototype was called a spiropulsator and was developed in cooperation with a Swedish technical company.
In 1934, Crafoord successfully performed a pulmectomy on a patient with bronchial cancer. In 1938, he presented his medical thesis on the procedure, describing the ventilator, technique, and clinical course of sixteen patients.2 His chief, Knut Harald Giertz, had an important network of surgical connections in Europe and the US and distributed Crafoord’s thesis widely.

In 1939, Crafoord toured centers of thoracic surgery in United States, partly funded by the Rockefeller Institute. He later reported that he was astonished and impressed by the many American doctors who had read his medical thesis. He met well-known American surgeons and became a close friend of John H. Gibbon in Philadelphia, the pioneer of the heart-lung machine. He also met Robert Gross in Boston and attended an operation on a seven-year-old girl to ligate a patent ductus arteriosus (PDA). Gross had improved this technique in the lab and successfully performed it for the first time in August 1938.3 Crafoord also presented a lecture at the annual meeting of the American Association of Thoracic Surgery titled “Pulmonary ventilation and anesthesia in major chest surgery,” for which he was awarded an honorary membership in the organization.
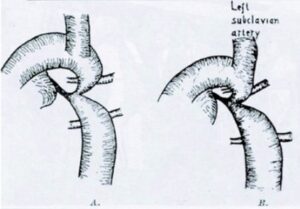
Based on knowledge gained from this trip, along with ongoing experimental work on animal and pathological specimens, in 1941 Crafoord performed the first operation in Sweden on a patient with patent ductus arteriosus.4 The duct was “unsually large and short” and he chose to divide the duct between vascular clamps and suture both ends. During a later operation for PDA, he had to stop severe bleeding by clamping the aorta above and below the ductus for twenty-six minutes. There was no resulting signs of ischemia in the lower part of the body, however. Thus, he hypothesized that an occlusion of the aorta for a longer period of time was possible. On October 19, 1944, Crafoord operated on an eleven-year-old-boy with a severe coarctation of the aorta.5 There were technical problems and the duration of the occlusion was two hours, but the lower part of the body was well perfused by collateral circulation. The patient recovered, and thirty-two years later, the outcome was excellent, as shown by aortic angiography (Figure 2). It was the first successful repair of coarctation of the aorta. Two weeks later, Crafoord successfully operated on another patient, a twenty-seven-year-old farmer. Crafoord included a schematic drawing of these two operations in the published article in 1945 (Figure 3) in the Journal of Thoracic Surgery.5 Robert Gross first performed this operation on July 6, 1945 and published in the New England Journal of Medicine.6 The achievements of the two research groups of Crafoord and Gross have been shown to be fully independent.7
In the late 1940s, Crafoord worked with Viking-Olof Björk on a pump oxygenator. It had a limited capacity to sustain circulation in dogs for thirty minutes. In 1948, Crafoord introduced a young doctor, Åke Senning, to the field of thoracic surgery. Senning would begin to work on a heart-lung machine for open-heart surgery in humans the same year Crafoord was appointed professor in thoracic surgery.
Åke Senning

Åke Senning (1915–2000) continued to develop the heart-lung machine, first based on a disc oxygenator, and later using rollers instead of discs (Figure 1). In 1951, after many animal experiments, he presented a paper on the limited use of the heart-lung machine at a congress in Paris. John H. Gibbon, the close friend of Crafoord and “father” of early heart-lung machines, was attending the presentation and decided to follow Senning and Crafoord back to Stockholm to take part in further experiments. In 1953, a heart-lung machine with flow control and heat-exchanger for hypothermia performed well in experiments with adult dogs. In February 1954, Senning traveled to the US and Canada. He visited John Gibbon and met John Kirklin at the Mayo Clinic and Bill Mustard in Toronto. After his return to Stockholm, the heart-lung machine was prepared for use with a suitable patient.
A forty-two-year-old woman with a presumptive diagnosis of mitral stenosis was considered for surgery in 1953. Later, there were clinical and radiological suspicions of myxoma. On July 16, 1954, Crafoord and Senning used the updated heart-lung machine to succesfully removed the myxoma from the left atrium.8,9 The patient made a full recovery and died many years later at the age of ninety-one. It was the second successful operation with a heart-lung machine in the world, and the first in Europe. Gibbon had performed the first operation by heart-lung machine the previous year.10
Senning introduced a temporary fibrillator in 1952. The application was based on results that he defended in his medical thesis the same year. It opened the way for temporary heart arrest to prevent air embolism. He cooperated with a Swedish medical equipment company and constructed a machine to generate ventricular fibrillation; then, if needed, he could produce defibrillation and also rhythmic pacing of the heart. Decades later, Senning was asked about his most important invention. His reply was: “Electrically induced ventricular fibrillation to prevent air embolism; that saved the most lives.”8
Senning was the major driving force behind the successful start of open heart surgery in Stockholm. A new thoracic clinic at Karolinska Hospital was opened in 1957. Crafoord was recovering from a subdural hematoma but soon resumed his leading duties. Senning, now professor in surgery, became chief of the new Department of Experimental Surgery financed by the Rockerfeller Foundation. He was also a consultant surgeon. Cooperation with cardiologists and radiologists in Stockholm exposed Senning to patients with various congenital heart defects. Total anomalous pulmonary venous drainage (TAPVD) of the supracardaic type was corrected.11 It is said that a neighbor child of Senning died of a transposition of the great arteries (TGA), which inspired him to propose a surgical method for correction on the atrial level, relying on the right ventricle to generate systemic pressure. In October 1958, a nine-year-old boy with simple transposition was successfully operated on by the new method of switching the venous return using flaps of autologous atrial tissue. This atrial switch procedure become known as a Senning operation.12,13 It was a breakthrough to perform this kind of “total correction” where the oxygenated blood was directed to aorta. Mustard, the cardiac thoracic surgeon in Toronto, in 1964 reported on a less complex operation for atrial switch.13 Mustard himself referred to Senning’s operation as a “complicated procedure” that “although genius, is technically extremely difficult in the infant or small child.”13 Senning had in 1955 attempted an arterial switch (of the great arteries) procedure without success. One obstacle was the difficulty in transferring the origin of the coronary arteries.

Senning had also been experimentally and clinically involved in coronary artery surgery. In 1958, he performed the first coronary operation worldwide using strip-graft technique. The treatment was an endarterectomy of coronary arteries completed with a vena saphena graft.
Between 1957 and 1962, when Crafoord was head of the department, 353 patients were operated upon with the support of the heart-lung machine. The mortality rate remained high, on average 30%.9 Senning referred to this period in a lecture in 2000: “In our first series of 200 open heart operations with the heart-lung machine there were 52 patients with Tetralogy of Fallot. Ten of the first twenty-five patients died and seven of the next twenty-five. Five of the first thirty-five patents died after closure of VSD, two of them were in Eisenmenger situation.”8 Continuous improvements in surgical technique decreased surgical mortality in the 1980s to less than 1%.8 The surviving patients also had good long-term results.
Senning, together with Rune Elmquist of the Elema-Schonander Company, had performed extensive studies of cardiac stimulation in animal experiments and in patients with complete atrioventricular (AV) block using transcutaneous pacing electrodes.8 In autumn 1958, they were approached by a woman on behalf of her husband who had developed a total AV block after having myocarditis. The patient, a forty-three-year-old man had been hospitalized for some months with multiple daily fainting episodes. On October 8, 1958, a small fixed-rate pacemaker was implanted in the abdominal wall and the electrodes sutured to the myocardium through a left thoracotomy.14 The first pacemaker failed after eight hours and had to be exchanged for a back-up system, which worked for several months (Figure 4). The patient received several new pacemakers over the years and lived until the age of eighty-six (Figure 5).
From 1961 to 1985, Senning was full professor and chairman of the department of surgery at the University of Zurich and established Zurich as one of the leading cardio-surgical centers in the world. He continued his clinical surgical work according to his conviction: “Don’t give up, try again, try harder.”15
Clarence Crafoord and Åke Senning were pioneers and pathfinders in thoracic and open heart surgery. They improved clinical surgical practice and provided hope for many patients and their families.
References
- Crafoord, C. Two cases of obstructive pulmonary embolism successfully operated upon. Acta Chirurgica Scandinavica. 1928; LXIV:172-86.
- Crafoord, C. Pulmonary ventilation and pulmectomy in man. Acta Chirurgica Scandinavica. 1938; 81: supplement 54.
- Gross, RE and Hubbard, JP. Surgical ligation of a patent ductus arteriosus. Report of the first successful case. J Am Med Assoc. 1939; 112: 719—731..
- Crafoord, C. Opererat fall av öppetstående ductus Botalli. Nord Med. 1942; 13: 285-9.
- Crafoord, C and Nyhlin, G. Congenital coarctation of the aorta, and its surgical treatment. J Thoracic Surgery. 1945; 14: 347-61.
- Gross, RE and Hufnagel, CA. Coarctation of the aorta. Experimental studies regarding its surgical correction. N Engl J Med. 1945; 233(10): 287-293.
- Naef, AP. The Story of Thoracic Surgery: Milestones and pioneers. Toronto, Lewiston, NY: Hogrefe and Huber, 1990, 86-87.
- Geronlanos, S. Åke Senning: in memoriam. Int J Artificial Organs. 2001; 24(2): 57-62.
- Rådegran, K. The Early History of Cardiac Surgery in Stockholm. J Card Surg. 2003; 18: 564-572.
- Kurusz, M. May 6, 1953: the untold story. ASAIO J. 2012; 58(1): 2-5.
- Senning, Å. Complete correction of total anomalous pulmonary venous return. Annals of Surgery 1958; 148: 99-103.
- Senning, Å. Surgical correction of transposition of the great vessels. Surgery 1959; 45(6): 966-980.
- Konstantinov, IE et al. Atrial switch operation: Past, Present, and Future. Ann Thorac Surg. 2004;77: 2250-8.
- Elmquist, R and Senning, Å. Implantable pacemaker for the heart. Proceedings of the Second International Conference on Medical Electronics, Paris, France, June 24-27, 1959. London, IIiffe and Son, 1960.
- “Åke Senning.” Wikipedia, September 27, 2022. https://en.wikipedia.org/wiki/Åke_Senning. Accessed January 2, 2023.
- Berggren, H and Olin, C. Från djärva pionjärinsatser till operationsresultat i världsklass. Läkartidningen 2005;102 (34): 2310.
GÖRAN WETTRELL, MD, PhD, FLS, is an associate professor and senior consultant in pediatric cardiology and pediatrics at Lund University, Sweden. His work focuses on pediatric pharmacology, cardiac molecular genetics, and primary arrhythmias. Other interests include male choir singing, travel, and medical history.

Leave a Reply