Fergus Shanahan
Dublin, Ireland
“You live and breathe paradox and contradiction, but you can no more
see the beauty of them than the fish can see the beauty of the water.”
– Michael Frayn (Bohr to Heisenberg), Copenhagen1
The language of medicine is loaded with misnomers, inaccuracies, and ambiguities, and is in need of reform.2 Paradoxes, on the other hand, deserve a different kind of attention. These seeming self-contradictions are set apart from other inconsistencies because of the truths they tell. The veracity of a paradox is at once appealing and vexing. Anyone who has tried to suppress a thought knows that trying not to think of white polar bears is a sure way to think of white polar bears!3 The comic impact of a paradox was famously explored in Joseph Heller’s Catch 224 and in Groucho Marx’s reluctance to be a member of any club that would accept him. However, the provocative nature of a paradox is its capacity to express familiar wisdom and this is particularly evident in medical science.
The more we learn, the more we learn how much we still have to learn; whereas, “what gets us into trouble is not what we don’t know, it’s what we know for sure that just ain’t so.”5 On the significance of the knowledge paradox in biology, Lewis Thomas regarded ignorance as the only scientific truth of which he was confident, and discovering “the depth and scope of ignorance” as the greatest contribution of modern science.6
Paradox appears in the title of thousands of medical science reports annually. An arresting title tends to be repeated and enhances the citation count, but many are not true paradoxes; they are instead a loose use of the word for unexpected observations or apparent inconsistencies awaiting resolution with clarification and context. Paradoxes aplenty have been linked with most major healthcare issues, including obesity, exercise, antibiotic development and resistance, productivity, and even burnout—wired from doing too much and tired from doing too little of what invigorates us.8-14 The paradox of precision medicine seems to be that it may not be precise and may not work any better than old-fashioned, low-tech approaches,15 whereas the paradox of modern science is its progression despite the problem of irreproducibility.16 Many of these seeming paradoxes will dissipate with research, whereas persistent paradoxes are more informative.
The enduring paradoxes of medicine are conceptual. For example, paradox is central to the pursuit of health; the more rigorously we try to define health and normality, the rarer they become. Illness, on the other hand, is universal. It is part of normal life, but society seems to hide it and hide from it. Other paradoxes present a dark perspective on the progress of healthcare. For example, fifty years ago the inverse care law was proposed by Julian Tudor Hart, a family practitioner working in the UK National Health Service (NHS): “The availability of good medical care tends to vary inversely with the need for it in the population served.”17 This remains valid and has global relevance. Doctors working in areas with the highest prevalence of sickness and mortality have fewer resources and less support than in the healthiest areas. Disadvantaged populations need more healthcare than advantaged populations but still receive less. This inequity may persist because of yet another paradoxical truism—the patient paradox. The “patient paradox” is described by Margaret McCartney, another NHS family practitioner, as follows: “if you are ill, you have to be persistent and determined to get help.…Yet if you are well, you are at risk of being checked and screened into patienthood, given preventive medication for something you’ll never get, or treated for something you haven’t got.”18
Pandemics remind us that the health of the population is dependent on the behavior of individuals. Paradoxically, public health interventions may benefit those at lower risk of disease rather than those at greatest risk, and thereby increase inequality in health.
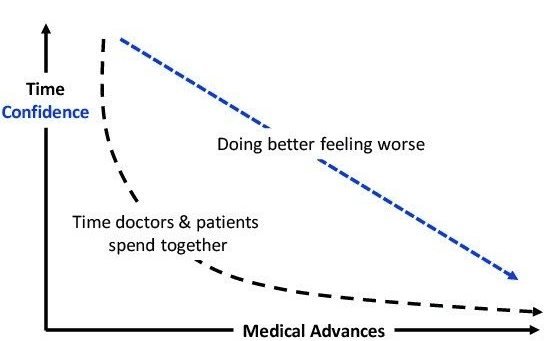
Advantaged populations are doing better but feeling worse. Described by the late Roy Porter in the opening lines of his medical history of humanity: “These are strange times, when we are healthier than ever but more anxious about our health.”19 Among the complexities of modern healthcare that may account for this, are more paradoxes. Despite an abundance of health messaging from professionals, commercial outlets, awareness campaigns, and health gurus in traditional and social media, even the most informed and educated patient may become distracted and confused. “The paradox is that people are awash in knowledge they may be unable to use.”20 Technology has also changed the doctor-patient relationship. Almost every diagnostic and therapeutic advance has shortened—not enhanced—the time patients and doctors spend together. Most disappointing but resolvable is the paradox of caregiving. Caregiving is core to the identity and values of all health professionals, and is vigorously upheld by medical schools; yet, they invest little time and resources in the education and practice of caregiving.21
Those who despair for the future of medicine may be heartened by one enduring paradox. Testimony from patients, including doctors, who are sick with incurable diseases confirms that carers have their greatest influence when it appears that there is nothing left to be done. “The fewer the therapeutic options available, the greater your involvement should be. When there is no cure, there is still much to be done to alleviate suffering.”22
Mathematical and semantic paradoxes may be curiosities to challenge the preciseness of human thought, but medicine’s mayhem of paradoxes are a mirror on progress. The true paradoxes embody a valuable insight and a lesson to teach. Others are perplexing and should be resolved so that progress means that less is more rather than plus ça change…
References
- Frayn, Michael. Copenhagen. Methuen Drama, London 1998.
- Shanahan F. The Language of Medicine. Liberties Press, Dublin, 2020.
- D M Wegner, D J Schneider, S R Carter 3rd, T L White. Paradoxical effects of thought suppression. J Pers Soc Psychol 1987;53:5-13.
- Heller J. Catch 22. Simon & Schuster, 1961.
- The Quote Investigator. It Is Better to Know Nothing than to Know What Ain’t So. Josh Billings? Artemus Ward? Will Rogers? Abraham Lincoln? Mark Twain? Friedrich Nietzsche? Anonymous? https://quoteinvestigator.com/2015/05/30/better-know/ accessed May 8th, 2021.
- Thomas L. Notes of a biology-watcher. The hazards of science. N Engl J Med 1977;296:324-328.
- Ades PA, Savage PD. The obesity paradox: perceptions vs knowledge. Mayo Clin Proc 2010;85:112-114.
- Banack HR, Stokes A. The ‘obesity paradox’ may not be a paradox at all. Int J Obesity 2017;41:1162-1163.
- Pontzer H. The exercise paradox. Sci Am 2017;316:26-31.
- de Vries JD, Bakker AB. The physical activity paradox: a longitudinal study of the implications for burnout. Int Arch Occup Environ Health. 2021 Oct 6. doi: 10.1007/s00420-021-01759-y.
- McKenna M. The antibiotic gamble. Nature 2020;584:338-341.
- Kaplan LJ. The pandemic paradox. Critical Care Medicine 2021;49:527-529.
- Wachter WM, Howell MD. Resolving the productivity paradox of health information technology. A time for optimism. JAMA 2018; 320:25-26.
- Jones SS, Heaton PS, Rudin RS, Schneider EC. Unravelling the IT productivity paradox – lessons for health care. N Engl J Med 2012;366:2243-2245.
- Interlandi J. The paradox of precision medicine. Sci Am 2016; April 1:16-18.
- Shiffrin RM, Börner K, Stigler SM. Scientific progress despite irreproducibility: a seeming paradox. Proc Natl Acad Sci USA 2018;115:2632-2639.
- Hart JT. The inverse care law. Lancet 1971;1:405-12.
- McCartney, M. The Patient Paradox. London: Pinter & Martin Ltd, 2012. Print.
- Porter R. The Greatest Benefit to Mankind. A medical history of humanity. WW Norton & Company, New York, London, 1997.
- Koh HK, Rudd RE. The arc of health literacy. JAMA 2015;314:1225-6.
- Kleinman A. Caregiving as moral experience. Lancet 2012;380:1550-1551.
- Aoun, Hacib. ‘From the eye of the storm, with the eyes of a physician.’ Ann Intern Medicine, 1992;16:335-38.
FERGUS SHANAHAN, MD, DSc, is emeritus professor of medicine at University College Cork, National University of Ireland. He loves people, words, and microbes. His most recent book, The Language of Illness, was published in 2020 by Liberties Press, Dublin.
Highlighted in Frontispiece Volume 14, Issue 4 – Fall 2022

Leave a Reply