JMS Pearce
Hull, England, United Kingdom
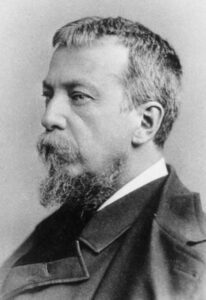 |
| Fig 1. Silas Weir Mitchell. Photo by Frederick Gutekunst, 1881. National Library of Medicine. Via Wikimedia. Public domain. |
Silas Weir Mitchell (1829 – 1914) (Fig 1) was born in Philadelphia, the seventh physician in three generations. Webb Haymaker gives an early clue to his unconventional personality when he recounts his smuggling of Frederick Marryat’s Midshipman Easy into a dark corner of a church pew to relieve the boredom of his puritanical upbringing.1 His early university performance in Philadelphia was poor. His preference for daydreaming, writing poetry and billiards prompted his father, Dr John Kearsley Mitchell, peremptorily to remark, “You are wanting in nearly all the qualities that go to make a success in medicine.”
Nevertheless, he enrolled at Jefferson Medical College in 1848, qualifying M.D. three years later. He proved to be a man of unusual imagination, breadth of vision, and eccentric curiosity who explored obscure areas of medicine including the complexities of social life, warfare, and psychogenic ailments. We can sense a prophetic Blakean vein in much of his work. A prolific writer, he also ventured into fiction and poetry with singular success.
After graduation, he traveled to Europe and fell under the spell of Claude Bernard, who probably sowed the seeds of his lifelong sense of scientific enquiry. Returning to Philadelphia, he became an experimental physiologist studying the effects of snake venom (after a near fatal personal encounter with a rattlesnake),2 the blood crystals of sturgeons, and the formation of uric acid. He described his visual hallucinosis (“resembling megrim”) after he had ingested mescal buttons.
Causalgia
A second phase of his life was principally clinical. During the American Civil War, he was seconded to a four-hundred bed U.S. Army Hospital in Philadelphia. With colleagues, he collected cartloads of wounded soldiers from the 1863 battle at Gettysburg, treated their wounds, and wrote voluminous notes on their injuries, culminating in several classic books and papers (Fig 2).3,4 At the suggestion of Professor Robley Dunglison he applied the term causalgia to the intractable pain that followed partial nerve injury, an entirely new concept.3,5 The essential points of his graphic depiction are worth recalling:
 |
| Fig 2. Injuries of Nerves and Their Consequences by Silas Weir Mitchell. 1872. |
Usually the pains from nerve hurts are either aching, shooting, or burning…principally burning.
Under such torments…the strongest man is scarcely less nervous than the most hysterical girl…
The men…described ‘mustard red hot,’ or ‘as a red hot file rasping the skin’…. this pain was an associate of the glossy skin.
… The burning arises …almost always during the healing of the wound. It never attacks the trunk, rarely the arm (upper) or thigh…Its favorite site is the foot or hand…a state of torture which can hardly be credited…
The part becomes exquisitely hyperaesthetic so that a touch or tap of the finger increases the pain. Exposure to the air is avoided…with a care which seems absurd, and most of the bad cases keep the hand constantly wet…Two carried a bottle of water and a sponge, and never permitted the part to become dry. The temper changes and grows irritable, the face becomes anxious and has a look of weariness and suffering. The sleep is restless…the rattling of a newspaper, a breath of air, the step of another across the ward, the vibrations of a military band or the shock of feet when walking, increase the pain. He walks carefully, carries the limb with the sound hand, is tremulous and nervous…in two cases the men found ease from pouring water into their boots…One wet the sound hand when obliged to touch the other.3
He rejected referred pain as the explanation:
If the burning were a referred sensation, it would sometimes be met with in cases of complete division of the nerves, and, therefore in parts devoid of tactile sensation. But, we have encountered no such cases…and the motion and touch may remain unaltered…the depraved nutrition, often so marked in the congested, denuded, and altered skin may give rise to a disease of the ultimate fibres of the sensitive nerves?
For treatment he used water dressings, “the one essential for comfort”.
He recognized phantom limb pain complicating causalgia in amputees. It was earlier portrayed by Ambroise Paré as “this false and deceitful sense” in 1551; in Aaron Lemos’s 1798 dissertation Dolorem membri amputati remanentem explicat; and by Johannes Müller in 1834. Weir Mitchell elaborated its features and mechanism in his fictional The Case of George Dedlow, published anonymously in 1866 in the Atlantic Monthly:
I found that the great mass of men who had undergone amputations for many months felt the usual consciousness that they still had the lost limb. It itched or pained, or was cramped, but never felt hot or cold… If they had painful sensations referred to it, the conviction of its existence continued unaltered for long periods; but where no pain was felt in it, then by degrees the sense of having that limb faded away entirely.… This change passes up the nerves towards the centres, and occasions a more or less constant irritation of the nerve-fibres, producing neuralgia, which is usually referred to that part of the lost limb to which the affected nerve belongs. This pain keeps the brain ever mindful of the missing part…that which he has not.
Unfortunately, causalgia is now confused with the chronic regional pain syndrome, an error related to lamentably imprecise nomenclature. Chronic regional pain often occurs with no evidence of primary nerve injury.
Other contributions
In Reflex Paralysis6 Weir Mitchell “described the sudden weakness of the limbs on the side opposite to forebrain injury, thus anticipating the lateralization of motor function by David Ferrier, Fritsch and Hitzig by several years.”7
He described “On a Rare Vasomotor Neurosis of the Extremities and on Maladies With Which it May Be Confounded,” which he named erythromelalgia (Weir Mitchell’s disease). He studied post-paralytic chorea, as well, and he deduced discovered that the cerebellum augments movement.7
But at times he was unorthodox. He developed his “rest cure” for patients with neurosis and hysteria based on “moral and physical components,” as described in his book Fat and blood. The title reflected that, in his experience, “women with depression and hysteria were often thin and anaemic. In addition to rest he removed the patient from their environment, askinged them to write their life history, and usinged exercise, electrical stimulation, and a nutritious diet.”7 It was often a lengthy, punishingly restrictive treatment. The famous story, The Yellow Wallpaper recounted by Charlotte Perkins Gilman told of her dreadful confinement when subjected to his rest cure.8 Another anecdote tells of Weir Mitchell “attending a lady sick unto death”; he dismissed his assistants from her room, then soon he too left her. When asked of her chances of survival, he replied, “Yes she will run out of the door in two minutes; I set her sheets on fire. A case of hysteria.” His melodramatic prediction proved accurate.7
In 1880, he founded the Philadelphia Neurological Society.9 He was awarded honorary degrees at Harvard, Princeton and Edinburgh, and was president in 1897 of the Association of American Physicians and in 1908 of the American Neurological Association.
In the last phase of an unusually varied career10 he turned to literature and published “nineteen novels, seven books of poetry, a scholarly and controversial biography of Washington, a children’s Christmas story (Mr. Kris-Kringle) that went through twelve editions, and a dissertation on William Harvey.”11
He died of influenza aged eighty-four. Harvey Cushing summed him up: “He was vain, but had much to be vain about.” Osler’s obituary more generously described him as:
A man of commanding presence and personality. He was a pioneer in neurology, and his influence of his work is writ large in the history of the development of that branch of medical science.
References
- Haymaker W. Weir Mitchell. In: The Founders of Neurology. 2nd edn, Springfield. Thomas, 1970: pp. 479-84.
- Walter RD. S. Weir Mitchell, MD-neurologist. Springfield, Ill: Charles C. Thomas, 1970.
- Mitchell SW, Morehouse GR, Keen WW. Gunshot wounds and other injuries of nerves. Philadelphia, Lippincott. 1864.
- Mitchell SW. Injuries of nerves and their consequences. Philadelphia Lippincott, 1872, chapter 8, pp. 195-201, 272, 292-5, 302 – 21.
- Pearce JMS. Silas Weir Mitchell (1829 – 1914) and causalgia. J Neurol Neurosurg Psychiatry 1990; 53: 763.
- Mitchell SW. Reflex paralysis, the result of gunshot wounds and other injuries of nerves. Philadelphia: Lippincott, 1864.
- Pearce JMS. Silas Weir Mitchell and the “rest cure”. J Neurol Neurosurg Psychiatry 2004, p. 381.
- Dunea G. Charlotte Perkins Gilman, apostle of women’s liberation. Hektoen Int. Winter 2019.
- Kline DG. A Centenary Tribute to Silas Weir Mitchell. World Neurology newsletter, August 4, 2014.
- Lovering JP. “Silas Weir Mitchell: His Life and Letters,” Twayne Pub. NY, 1929.
- McHenry LC, Jr. Silas Weir Mitchell. N Engl J Med, April 2, 1959.
JMS PEARCE is a retired neurologist and author with a particular interest in the history of science and medicine.

Leave a Reply