JMS Pearce
Hull, England, United Kingdom
 |
| Fig 1. Farmer George & his wife. Published by William Holland. 1786. © The Trustees of the British Museum. CC BY-NC-SA 4.0. |
The Hanoverian King George III (1738–1820) was a diligent man of wit and intelligence, a man who enhanced the reputation of the British monarchy until he was finally stricken by illness. When this drove him from regal duties, politicians realized they missed his calming effect on their squabbles.1 In many years of sanity, King George started a royal collection of books (65,000 were later given to the British Museum as the nucleus of a national library) and opened his library to scholars. He founded and paid the costs of the Royal Academy of Arts, was the first king to study science, and built his own astronomical observatory. He promoted agriculture on the crown estates at Richmond and Windsor and was known affectionately as “Farmer George” (Fig 1).
In 1966 Ida Macalpine and her son, Richard Hunter, both highly repected psychiatrists and historians, claimed that contemporary accounts of King George III’s illnesses showed that he suffered from acute intermittent porphyria (Fig 2).
They later changed the diagnosis to variegate porphyria. At first widely accepted, this assertion became the subject of heated polemics. Between January and July of 1765, King George III showed signs of madness. His Court kept it secret; happily, he recovered quickly. In June 1788 he had abdominal pain diagnosed as biliary concretions, and was sent by Sir George Baker, MD to take the waters in Cheltenham, where his health was restored. In October he was seized “by spasms of the stomach” of such severity that great alarm was felt in the royal household. He became erratic in his habits, disordered in dress, sexual in his behavior, and garrulous in speech.
This was noted by the royal favorite Sarah Siddons. According to Fanny Burney (Keeper of the Queen’s Robes), he was “gracious almost to kindness, but on the other hand the hoarseness of his voice, the volubility of his language, and the vehemence of his gestures, startled … beyond measure.” He exclaimed to the Duke of York, “I wish I might die, for I am going to be mad.” At the same time, he had leg pains, cramps, weakness, burning, and stiffness that were diagnosed as rheumatism and gout. Sweating, head pains, tremors, and foaming at the mouth were other observed symptoms.
Drs. Warren, Halford, Heberden, and Sir George Baker were summoned. They decided that his life was in danger, but in the event of recovery they feared for his sanity. The news of the King’s madness leaked, and his physicians were often criticized.
After much argument about his management, Dr. Francis Willis was called in by the Queen on December 5, 1788; he prescribed Peruvian bark (quinine), blistering, and calomel. His harsh treatments also included a strait-jacket, although he permitted some liberties.2 After confinement in Kew Palace, George was well enough to be seen walking with the Queen on February 14, 1789.
 |
| Fig 2. Macalpine and Hunter, British Medical Journal, 1966. |
Willis, vicar of Gretford near Stamford, kept a private madhouse. He had taken the Oxford DM in 1779 and was to become fellow and vice principal of Brasenose College. His services were generously rewarded and on March 10, 1789, the physicians left from Kew amidst celebrations—“the most magnificent illumination.” Lord Macaulay declared “the nation was wild with delight.”
Remission and relapse
After the 1788-9 episode, he remained well for twelve years until a relapse in February 1801; but he quickly recovered. Further relapses occurred in January 1804 and included an attack of painful paralysis, colicky abdominal pain, constipation, and vomiting. In October 1810, after the death of his daughter Amelia, he relapsed with maniacal behavior, which persisted episodically until his death in 1820. The Prince of Wales was appointed Regent in February 1811.
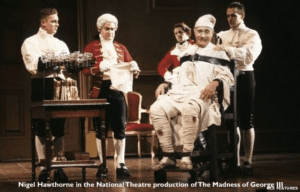 |
| Fig 3. Nigel Hawthorne in the National Theatre production of The Madness of George III. Rex Pictures via BBC News. |
Problems of diagnosis
Since the development of reddish-brown urine after standing is characteristic of acute porphyria, a tempting diagnostic clue was the observation of discolored urine on four occasions.3 Sir George Baker on Oct 18, 1788 wrote in his diary that the urine was bilious (green-brown). However, on Aug 26, 1819, Dr. Matthew Baillie and Dr. John Willis reported “bloody water.” Sir Henry Halford wrote:4 “The water is of a deeper colour—and leaves a pale blue ring upon the glass near the upper surface.” To Macalpine and Hunter this suggested acute intermittent porphyria.3 However, Arnold observed in The Lancet (1996) that “the doctors prescribed powdered Aloes socotrina (a cathartic) and extract of Taraxacum officinale (a laxative and diuretic). Thus, the King probably had a condition that would lead to overproduction of urinary indican, and with bacterial sulfatase would cause the curious blue rim described.”
Macalpine and Hunter wrote, “The symptomatology reads like a textbook case: painful paresis of arms and legs; vocal paresis, visual disturbances and other signs of bulbar involvement; radicular pain; autonomic disturbances with tachycardia and sweating attacks; and encephalopathy ranging from insomnia to excitement, raging delirium, stupor, and fits.”3 They subsequently modified their original diagnosis to porphyria variegata because of his skin wheals. 5,6,7 Their extensive research was based on the forty-seven volume Willis Manuscripts, ten boxes of Queen’s Council Papers, Sir Henry Halford’s daily record of the illness in 1811, and Sir George Baker’s diary. They identified nine episodes of major and minor attacks from 1765 to 1810.
His sanity fluctuated markedly over the ensuing years, and the ever popular King was further afflicted by loss of vision attributed to cataracts and by deafness. He held conversations with the ghosts of long departed statesmen, but curiously never forgot that he was King of England. His loyal Queen Charlotte died at Kew in November 1818. After a rule of sixty years, King George died aged eighty-one in 1820. The royal malady caused considerable consternation. His many physicians3 were handicapped by the prevailing ignorance about neuropsychiatric diseases. Public bulletins were phrased with discretion and that concealed their observations. Physicians used no stethoscopes, tendon hammers, or clinical thermometers. The distinctions between delirium and insanity were ill-defined.
The distinguished biochemists Claude Rimington8 and Hans Krebs, John Brooke, a leading Georgian historian, and Abraham Goldberg, a porphyria expert, all supported the conclusions of Macalpine and Hunter. By contrast, in 1997 Brownstein viewed the royal malady as “a unipolar mania of late onset, the sine qua non of bipolar disorder, in this instance complicated by the toxicity of quinine, antimony, and purgatives.” Professor CE Dent aptly noted that Macalpine and Hunter overstressed the varied urine colors, biochemistry, and genetics: “the urine in an acute attack of either form of porphyria is usually of normal colour when freshly passed…The essential and characteristic feature, not present in the descriptions of the royal malady, is the development of reddish or brownish coloration on standing.” He disputed porphyria as the diagnosis9 because of its rarity in cases not caused by drugs, but “while it is not possible to say that the cases in the Royal Family did not have a form of porphyria, it is possible that they could have had a lot of other things producing similar manifestations.” Much of his criticism related to the second paper5 that alleged porphyria in thirteen generations of the Royal Family.
Studies by Peters and colleagues have contested Macalpine and Hunter’s claim and conclude that he suffered from recurrent mania (four episodes), with chronic mania and possibly a degree of fatuity during the last decade of his life. 10,11 The opinion of Peters, a non-medical research fellow of the Institute for Archaeology and Antiquity at Birmingham, may not have been entirely objective. He accused the highly respected Macalpine and Hunter of being “misleading, and some interpretations were bordering on the fraudulent.”12 His comments appeared vituperative when he stated that Macalpine, formerly Hirschmann (née Wertheimer), had trained in medicine in various German universities, and that the research was colored by their philosophical agenda. He skeptically acknowledges: “It is not at all clear why so many eminent professional historians supported the porphyric claim,” but then blames editorial writers in the British Medical Journal. A computer analysis of the British monarch’s use of words lends indirect support to a diagnosis of manic psychosis.13
Comment
This polemic exposes the dilemmas of retrospective diagnosis. Can we reliably diagnose diseases of the past, especially mental disorders, in which objective criteria are sadly lacking? There is no doubt that the King was intermittently mad or psychotic, and that some of his symptoms were maniacal. Unfortunately, no objectively testable basis for manic or manic-depressive psychosis has so far established. Many have reasonably discounted porphyria,9,10,14 but uncertainties remain. His manic psychosis may have been symptomatic of porphyria, or indeed of other undiscovered neural or biochemical disorders. As Roy Porter observed: “Aetiology remains speculative, pathogenesis largely obscure, classifications predominantly symptomatic and hence arbitrary….”14 The nature of George III’s illness is likely to remain an insoluble mystery, though a source of fascinating discourse.
An Oscar nominated 1994 film based on Alan Bennett’s play, The Madness of King George III, (Fig 3) won three BAFTAs and grossed over $15 million in the US alone.
References
- Worsley, L. “What Was the Truth about the Madness of George III?” BBC. From the Section Magazine April 15, 2013. www.bbc.co.uk/news/magazine-22122407.
- Pearce, JMS. “The Role of Dr. Francis Willis in the Madness of George III.” Eur Neurol 2017;78:196–199.
- Macalpine, I, Hunter, R. “The “insanity” of King George III: a classic case of porphyria.” BMJ 1966; 1: 65-71.
- Halford, H. Essays and orations, read and delivered at the Royal College of Physicians. 2nd ed. London: John Murray, 1833.
- Macalpine, I, Hunter, R. “Porphyria in the royal Houses of Stuart, Hanover, and Prussia: A follow-up study of George III’s illness.” BMJ 1968;1:7-18.
- Macalpine, I, Hunter, R. George III and the mad business. London: Allen Lane, Penguin Press, 1969
- Dean, G. The porphyrias: a story of inheritance and environment. 2nd ed.pp.167 et seq. London: Pitman Medical, 1971.
- Neuberger, A, Goldberg A. Claude Rimington: Biogr Mem Fellows R Soc. 1996; 42:365-78.
- Dent, CE. “Royal malady.” Br Med J 1968:1:311–3.
- Peters, TJ, Beveridge, A. “The madness of King George III: a psychiatric re-assessment.” Hist Psychiatry 2010;21:20–37.
- Peters, TJ, Beveridge, A. “The blindness, deafness and madness of King George III: psychiatric interactions.” J R Coll Physicians Edinb 2010;40:81–5.
- Peters, T. “King George III, bipolar disorder, porphyria and lessons for historians.” Clin Med (Lond). 2011;11(3):261-264.
- Rentoumi, V, Peters, T, Conlin, J, Garrard, P (2017) “The acute mania of King George III: A computational linguistic analysis.” PLoS ONE 12(3): e0171626. https://doi.org/10.1371/journal.pone.0171626.
- Porter, R. Madness: A Brief History. Oxford, Oxford University Press 2003.
JMS PEARCE is a retired neurologist and author with a particular interest in the history of medicine and science.
Winter 2022 | Sections | History Essays

Leave a Reply