Shrestha Saraf
Sutton Coldfield, UK
Sudarshan Ramachandran
Birmingham, UK
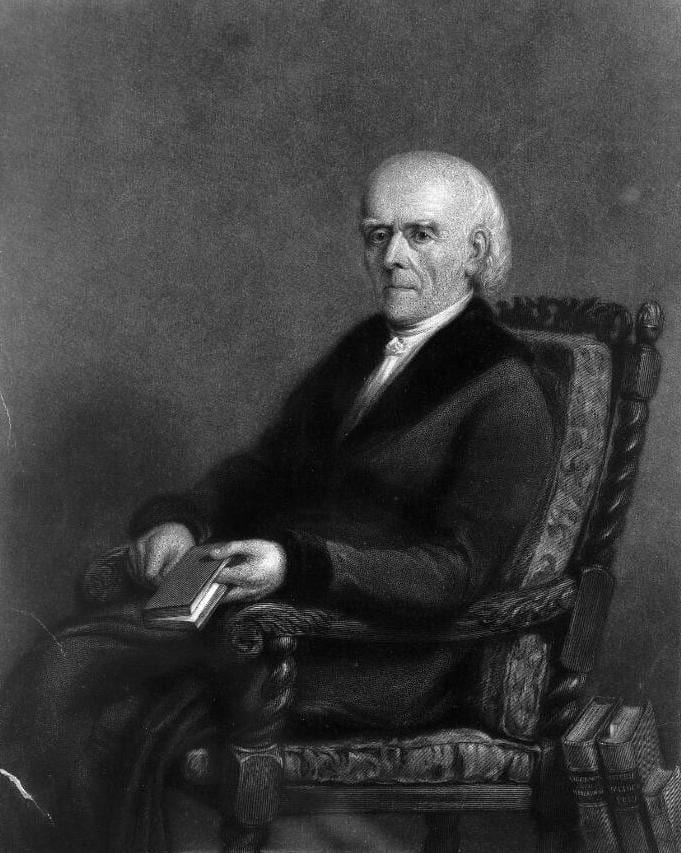 |
| Samuel Christian Friedrich Hahnemann. Mezzotint by R. Woodman after G. E. Hering. Wellcome Collection. Public Domain Mark |
Homeopathy, based on a pseudoscientific system of alternative medicine, was developed by German physician Samuel Hahnemann around 1790. The primary principle of homeopathy is “like cures like,” i.e., a substance that causes symptoms can also be used to remove those symptoms. The trigger for the development of this system was dissatisfaction with the medical practice at that time of prescribing of toxic substances like arsenic and lead. While investigating the harmful effects of these substances, Hahnemann posited that the use of small amounts of these compounds could treat the very illnesses that were caused by larger quantities. He spent the next several years studying the effects of a range of natural substances, experimenting on himself and a group of volunteers. He diluted the substances to the lowest level possible to produce a response and also avoid harmful side effects. These studies laid the foundations for homeopathic medicine.1
Homeopathy is also based on succession, a process of repeated dilution and mixing. Advocates of homeopathy believe that the more diluted a substance is, the greater the efficacy.2 This is in defiance of Avogadro’s number, defined as the number of elementary particles (molecules, atoms, compounds, etc.) per mole of a substance, which is equal to 6.022×1023 mol-1. Thus, in a dilution greater than 1023 there is a possibility of the sample not containing a single active molecule. The typical dilution in homeopathy is 30C, meaning that the original substance has been diluted by one drop in a hundred, thirty times. This means that it contains less than one part per million of the original substance (one in 1060).3 This then raises the question: if there is hardly any active ingredient present, how effective is the treatment?
In an attempt to reduce or eliminate ailments, some individuals prefer homeopathic remedies over conventional medicine, while for others, homeopathy occupies a position of last resort. Homeopathic treatments are most often used for asthma, ear infections, hay fever, high blood pressure, allergies, dermatitis, arthritis, and mental health conditions such as depression, stress, and anxiety.2
Regulation of medical practice is an integral part of healthcare governance in the United Kingdom. No such legal regulation exists for practitioners of homeopathy; there are no requirements for qualifications, accreditation, or revalidation.2 The nature of consultations varies but includes detailed case histories of patients’ medical history and symptoms. Attention is paid to the “modalities” of symptoms (whether they change according to the weather, the time of day, the season, etc). Detailed subjective information is gathered about mood and behavior, likes and dislikes, response to stress, personality, and reactions to food. The aim is to build a “symptom picture” of the patient. This subjective profile is then matched with a “drug picture” in the homeopathic Materia medica. Homeopathic treatments are then prescribed.4
Evidence has become the cornerstone of modern medicine and homeopathy should not be exempt from this rigorous examination. By the year 2014, there were 104 good-quality randomized controlled trials (RCTs) on homeopathic remedies:5 41% (43 trials) of these showed mainly positive outcomes, 5% (5 trials) showed mainly negative outcomes, and the remaining 54% (56 trials) were not conclusive.5 If the RCTs were stratified by outcome, the evidence could be evaluated by presenting symptoms, conditions, and population. Inconclusive results need to be evaluated as they are in conventional medicine, which may demonstrate pathologies and subgroups where outcomes for homeopathic remedies are clearer. Trials can be improved by having larger sample sizes and using more rigorous research methods.6
According to the House of Commons Science and Technology in the United Kingdom (UK), there is no evidence suggesting homeopathy to be an effective treatment for any health condition.2 This lack of evidence, in addition to the previously mentioned issues with dilution, leaves a fundamental question of efficacy. Apart from desensitization techniques used by immunologists and allergy specialists, the tenets of homeopathy are not accepted by mainstream science nor consistent with long-accepted principles about how the physical world works. A 2010 report on homeopathy by the committee stated that the idea that “like cures like” is “theoretically weak.”2
This raises questions as to whether homeopathy is a placebo, a view held by many scientists. The placebo effect can be extremely powerful, with individuals perceiving that receiving some form of treatment will transform their disease or symptoms for the better. A placebo may modify the neurological signals that lead to symptoms such as pain. Placebos have been shown to be most effective in treatments for pain management, stress-related insomnia, and cancer treatment side effects (e.g., fatigue, nausea).7
Interestingly, there have been many trials comparing homeopathic treatments to placebos. The majority of these trials have resulted in inconclusive outcomes because of poor design or biased research methodology.8 Less robust trials are more likely to favor homeopathy over placebo.3
National Health Service (NHS) England, following a review of the evidence, decided against the funding of homeopathic remedies. This decision was backed by a High Court judgment in 2018 after a challenge by the British Homeopathic Association.2 A document prepared by the Specialist Pharmacy Service of the NHS outlines the details of the evidence and the lack of demonstrable benefit.9
In light of these issues, homeopathy must perhaps be considered a placebo at present. However, it must be stated that the placebo effect can be useful in many subjective conditions such as pain and discomfort. It may be an adjunct to conventional treatments that address the underlying cause. Unless practitioners of homeopathy embrace the culture of evidence and carry out trials that are robust and well designed, homeopathy will not achieve front-line therapeutic status. Transparency, evidence-based practice, and regulation could move homeopathy into the mainstream, but failure to do so will keep it confined to the periphery.
References
- https://homeopathy-uk.org/homeopathy/the-history-of-homeopathy.
- https://www.nhs.uk/conditions/homeopathy/ – Accessed 11 March 2021.
- Bad Science – Ben Goldacre – 2009.
- Andrew Vickers, Catherine Zollman. Homeopathy. BMJ 1999 Oct 23; 319(7217): 1115–1118.
- https://homeopathy-uk.org/treatment/evidence-for-homeopathy – Accessed 11 March 2021.
- https://homeopathy-soh.org/resources/clinical-trials/ – Accessed 7 April 2021.
- https://www.health.harvard.edu/mental-health/the-power-of-the-placebo-effect – Accessed 7 April 2021.
- Robert T. Mathie, Nitish Ramparsad, Lynn A. Legg, Jürgen Clausen, Sian Moss, Jonathan R. T. Davidson, Claudia-Martina Messow, and Alex McConnachie. Randomised, double-blind, placebo-controlled trials of non-individualised homeopathic treatment: systematic review and meta-analysis. Syst Rev. 2017; 6: 63.
- https://www.england.nhs.uk/wp-content/uploads/2017/11/sps-homeopathy.pdf – Accessed 16 May 2021.
SHRESTHA SARAF is a current A level student who aspires to study Medicine at university. She is passionate about science and science-related topics.
SUDARSHAN RAMACHANDRAN is a Professor of Metabolic Medicine, working at University Hospitals Birmingham and University Hospitals of North Midlands.
Spring 2021 | Sections | Doctors, Patients, & Diseases

Leave a Reply