 |
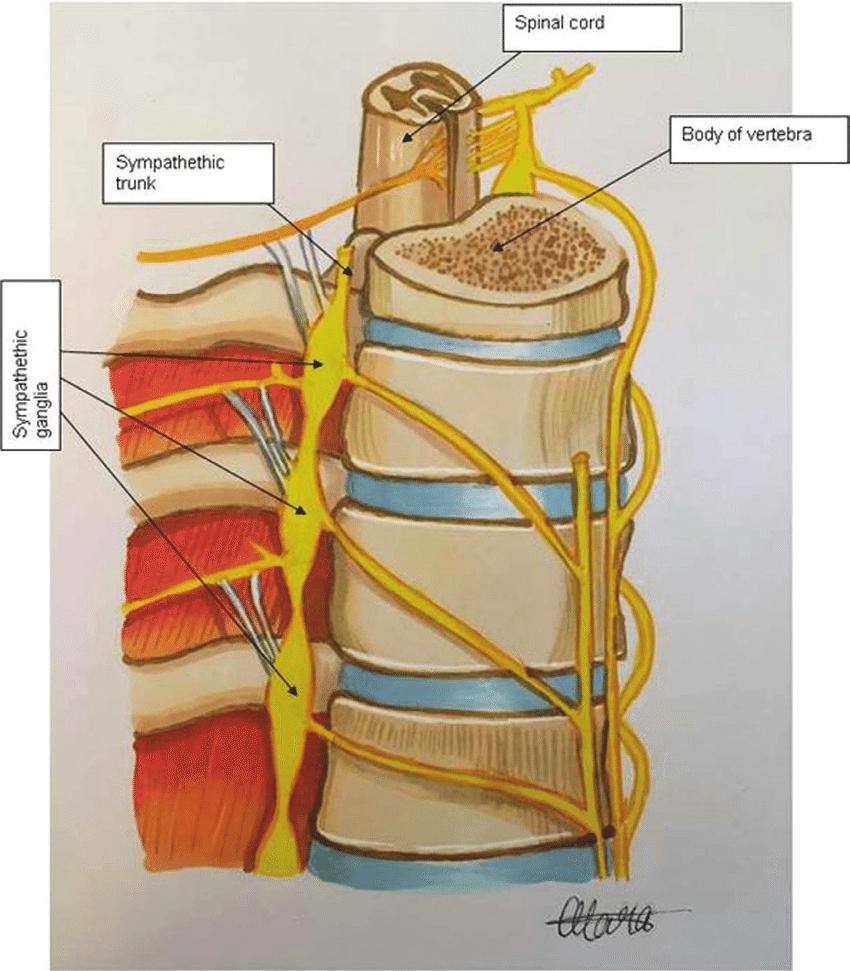
| Components of the sympathetic trunk. Redrawn from Wolf-Heidegger’s Atlas of Human Anatomy. From Anatomic Origin and Molecular Genetics in Neuroblastoma. CC BY 3.0. |
Sympathectomy for essential hypertension was introduced in the late 1920s at a time when no effective medical treatment was available. It consisted of resecting several sympathetic neurons that exit the spinal cord from the mid to lower spinal cord and are arranged in two columns of nodules called ganglia on either side of it. Sympathetic neurons are part of the involuntary nervous system that, among other functions, regulates blood pressure by determining the state of relaxation or constriction of the blood vessels.
During the first half of the twentieth century, thousands of hypertensive subjects underwent the operation. Thoracic or lumbar sympathectomy was usually combined with removing part of the celiac ganglion and of the splanchnic nerves supplying the abdominal and pelvic viscera. Some surgical approaches were limited to sectioning only the second, third, and fourth lumbar ganglia; others were more extensive. In the classic thoracolumbar sympathectomy carried out by Smithwick on 2,000 patients, the lower five thoracic and the upper three lumbar ganglia were excised.
From the outset, and certainly by 1950, sympathectomy was a subject of controversy. Lack of uniformity in case selection, operative procedures, and analysis of results contributed to this uncertainty. In general, more extensive surgery was carried out in younger people with severe disease. Overall operative mortality was 4%. Postoperative pain was more frequent with the thoracic surgery, which could also cause collapse of the lung and pleural effusions. Postural hypotension was common during the first few months. Some patients developed Raynaud’s phenomenon, others had paralysis of the abdominal wall, constipation, and occasionally hematemesis. All patients having their lumbar ganglia removed became impotent.
Following surgery headache was often relieved. Grade three or four hypertensive retinopathy was impressively improved, but only in very few patients. A reduction in diastolic blood pressure of some 15 mmHg was maintained in about 25% of patients, and some studies reported statistical prolongation of the five-year survival rate. As late as 1959 one group justified sympathectomy by its sustained blood pressure lowering and the high rate of symptomatic relief, writing that “the majority of patients returned to work after the operation, kept their jobs, and were able to forget about themselves and their disease for many years.”1
But by 1954 Fishberg had concluded in his book that sympathectomy was only palliative and not curative, and recommended its avoidance in asymptomatic patients no matter how high the blood pressure.2 It was not indicated in patients over fifty, nor in patients with predominant systolic pressure, nor in renal insufficiency. A high degree of cerebral or coronary arterial sclerosis was also a contraindication, and the procedure was not recommended if rest, low-salt diet, and sedation had been effective. With the advent of potent drugs, beginning with the ganglion blocking agents in the 1950s, the procedure was abandoned and is now only of historic interest. It reflects a time, not so long ago, when severe hypertension was a killer and anything likely to help seemed worth trying.
References
- Arthur M Fishberg. Hypertension and Nephritis, Lea & Febiger, Philadelphia, 1954 (first edition 1930)
- Newcombe CP, Shucksmith HS, Suffern WS. Sympathectomy for hypertension. BMJ 1959; 1:142 (January 17)
GEORGE DUNEA, MD, Editor-in-Chief
Fall 2020 | Sections | Nephrology & Hypertension

Leave a Reply