Sally Mather
Chris Millard
Ian Sabroe
Sheffield, England
The experience of uncertainty has appeared as a frequent narrative in articles, autobiographies, and memoirs written by doctors over the last century. A persistent belief that better training, tests, evidence, and pathways will reduce uncertainty has not been borne out in the experience of contemporary clinicians. Beliefs about uncertainty in medicine 100 years ago persist today. The failure to find a way to work with the inherent slipperiness of uncertainty has created an associated stigma and fear that has amplified its power. The widespread perception of uncertainty as a solvable problem is problematic, and attempts to reduce it are likely to fail. A new and constructive approach to uncertainty is needed.
One of the most persistent constructs of the twentieth century has been the doctor as wise protector. While it has always been acknowledged that no one could expect to practice medicine with unfaltering certainty,1 doctors endeavored to keep this fact well-hidden from the public for fear of losing professional credibility2,3 and to protect the patient from the “mental effects of uncertainty”2 which were thought to be potentially “devastating.”4 These reasons continue to be cited as explanations for a reluctance to disclose uncertainty.5-7 Whether the spoken need to protect patients is a sublimation of an unspoken fear about personal credibility is unclear. In 1991 Arborelius et al8 examined how British primary care physicians kept their uncertainty hidden from patients. One doctor conducted unnecessary examinations “to keep [their] honour”; another made meaningless conversation in order to gain time, while another submitted to a patient’s “aggressive” demands despite knowing it would be of little use, “just to do something.” Maladaptive strategies of coping with uncertainty evolve early: many learn during medical school “that the best way to handle uncertainty is to disguise, deny, or deflect it.”9 Attempting to reduce uncertainty is another common strategy, but this can result in intolerance of uncertainty and, consequently, excessive testing.10 Doctors also have a tendency to resolve uncertainty by action rather than inaction,11 resulting in links between medical uncertainty and increased hospital admissions, greater expenditure, and over-treatment.11,12
There is one especially challenging area of uncertainty: clinicians’ own errors. Following a landmark article in the New England Journal of Medicine, Hilfiker wrote of the challenges in facing mistakes. Determining how choices have influenced shifting outcomes in difficult situations can be hard, so there may be uncertainty as to whether a mistake has been made at all.13 Living up to the wise protector role myth leaves physicians even less able to discuss mistakes with colleagues and patients and to analyze and accept responsibility for their own errors.
Overwhelmingly, uncertainty is described in negative terms in the literature (Figure 1). Intolerance to uncertainty has been repeatedly linked to burnout,14-16 which may explain why some doctors are observed to transfer negative emotions to patients.17,18 The Maslach Burnout Inventory measures depersonalization, which may include cynicism and negative attitudes towards patients, as one of three dimensions of burnout syndrome.16 Intolerance of uncertainty may be a factor in the shortage of doctors in branches of medicine characterized by high levels of uncertainty, such as psychiatry and primary care.19
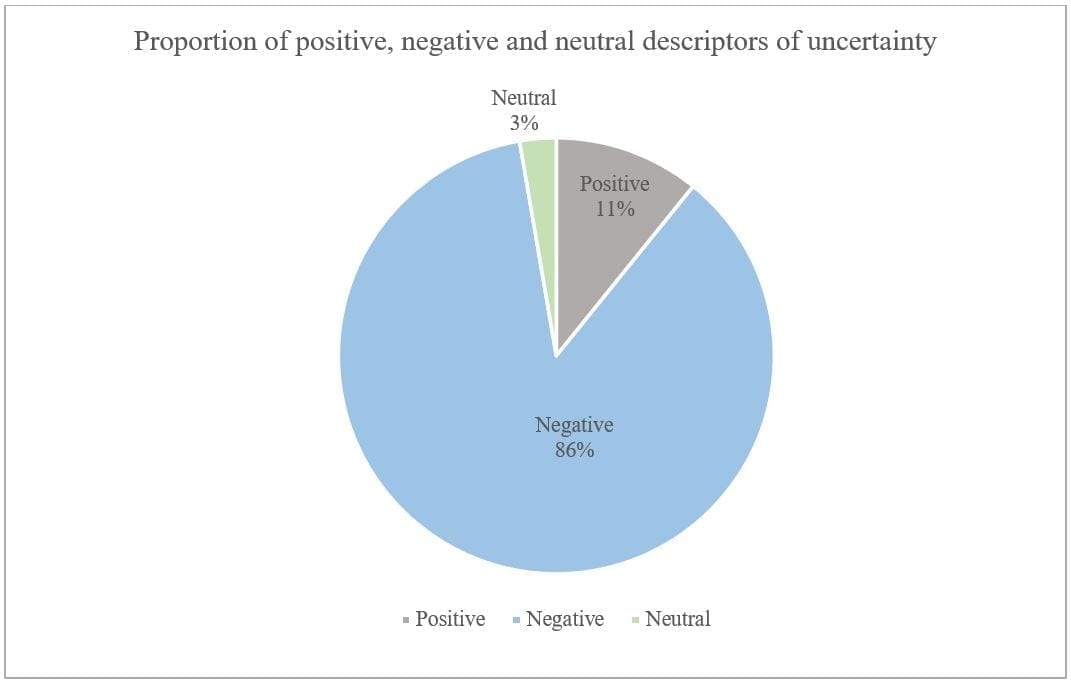 |
| Figure 1: 157 texts discussing medical uncertainty were analyzed for descriptors of how uncertainty feels. 37 different descriptors were found, which were compiled into a table charting the frequency of their use. Descriptors were categorized as expressing “positive”, “negative”, or “neutral” attitudes towards uncertainty; the frequency of descriptors is shown proportionally by category. Positive terms included: hope, optimism, stimulated, thrill. Neutral terms included: comfortable. Negative terms included: anxiety, fear, frustration, stress, helpless, inadequacy, threatened, insecure, doubt, self-doubt, dissatisfaction, concerned, uncomfortable, guilt, ignorant, unhappy, panic, confusion, worry, vulnerability, unrest, shortcoming, disquieting, unfulfilled, torment, awkward, lack of confidence, distress, angst, powerless, loss of control, resentment, annoyed. |
The simplistic view of medicine as a science is another remarkably persistent and unhelpful belief. Beresford20 points out that “the problem is not that clinical decision-making is an under-developed science, but that it has been confused with science.” Many elements of clinical medicine are distinctly “unscientific,” such as the patient narrative,21 doctors’ judgment,22 and intuition.23 The twentieth century has seen countless ground-breaking developments in medicine, leading to the attitude that “its secrets have yielded to logic with such success that time alone is needed to solve remaining problems.”24 Evidence-based medicine’s promise to fully rationalize the profession perpetuates the belief that medicine’s uncertainties and subjectivities are merely a “temporary flaw . . . that will disappear when the last biological puzzle has been solved.”22
Increases in knowledge have not resulted in decreases in the narrated experiences of uncertainty. Instead, the increasing complexity of medicine serves only to further heighten the doctors’ uncertainty.
One reason for this is that the advancement of knowledge may highlight more clearly what is not known,20-25 and in particular, that what we think we know is not necessarily true.26-27 As research alters our understandings, our current beliefs stand on ever shakier ground. As Murray Enkin, a professor emeritus of obstetrics told medical students on their first day: “Half of everything I am going to say here is very likely wrong. The problem is I do not know which half.”27
Additionally, this explosion of knowledge has caused “information overload” and the fear that one does not know enough to become common sources of uncertainty.28 Evidence and guidelines are frequently reappraised, resulting in uncertainty as to whether one still adheres to best practices. Discussions of prognosis are a particular challenge, as new therapies result in rapid reappraisals of survival estimates.6
With each uncertainty that is apparently resolved, a new set of uncertainties presents: “Uncertainty borders the edges of knowledge, so that the larger the territory known, the more extensive are the settings in which uncertainty is experienced.”29 For example, when laboratory tests were first becoming a routine part of care, many believed they would remove much of the diagnostic uncertainty of medicine.30,31 However, doctors now face uncertainty about poor specificities and dichotomous thresholds for interpretation.32 Psychiatry provides a further example of the slipperiness of uncertainty. The mid-twentieth century saw many lamenting the poor understanding of psychiatric principles,33,34 but when this improved, complaints evolved into how to apply this information to specific patients.35 Similarly, the blurred lines of psychiatry—such as when abnormal behavior becomes mental illness, or when to intervene—were sources of uncertainty in the twentieth century,35 but once clear diagnostic criteria and guidelines were established, uncertainty arose about their applicability to individual patients and the soundness of the evidence behind them.36,37
Thus, scientific advances relocate rather than reduce uncertainty.
Since uncertainty is here to stay, we must learn healthier ways of addressing it. Many attempts have been made to solve the “problem” of uncertainty; however, one hundred years and countless technological advances later, medical uncertainty has not diminished. The decades-long effort to produce a working taxonomy of uncertainty is a prime example of the endless loop we find ourselves in when uncertainty is regarded as a solvable problem. These attempts to pin down uncertainty and reconstruct it into something concrete and workable have continued since Fox produced her taxonomy of uncertainty in 1957.38 However, uncertainty is an experience as well as a theory of knowing, and its landscape is personal to those experiencing it.
Many doctors cope with uncertainty rather than thrive in it, but this can and should change. The stereotype of the wise protector is doomed to hurt doctor and patient alike. A great joy of medicine has always been its relational aspect, standing alongside those in times of need and navigating difficult journeys together. In this practice, uncertainty can be a source of hope,6,39 though we do not acknowledge it as such and we can be quick to judge those who choose a different path from our own.
It is easy to suggest that we educate doctors and patients about uncertainty, but it is harder to show how to deliver this education meaningfully, in ways clinicians carry forward without removing the striving for quality. Evidence and knowledge are vital, but uncertainty will never go away and must be examined in a more holistic way in order to understand the experience of delivering care. Too often we teach how to deliver care, but not how that experience feels. Clinicians must learn to assimilate uncertainty into their experience in order to thrive in it.
The literature regarding medical uncertainty appears to reflect progress in this, alongside twenty-first-century ideas like postmodern medicine and critical psychiatry, which reject the ideas of certainty40,41 and science as a solution.42 Simpkin and Schwartzstein argue that the ability to work within the blurred lines of uncertainty is what sets the doctor apart from the binary codes of the machines now capable of performing many of the doctor’s routine tasks.43 Admitting that uncertainty is insoluble is an important step in building our tolerance, paving the way for more constructive reactions than the “disguise, deny, or deflect” approach. Uncertainty has many benefits, including protection from biases, assistance in the search for the correct diagnosis, and the provision of hope—hope that the prognosis is wrong, that the situation may turn out better than anticipated, that cure may come when least expected. We can embrace our own uncertainties to share hope with those we care for.
References
- Hoffman FL. The Accuracy of American Cancer Mortality Statistics. Am J Public Health. 1914 Nov 30;5(6):526-527.
- Lazarus-Barlow WS. Cancer propaganda. Acta Radiol. 1926;7:142-146.
- Simpson JB. Surgery in General Practice: Its Difficulties and Limitations. Edinb Med J. 1936;43(7):426-437.
- Thomas HM. What is psychotherapy to the internist? JAMA. 1948 Nov 20;138(12):878-880.
- Braddock CH. Supporting shared decision making when clinical evidence is low. Med Care Res Rev. 2013 Nov 1;70(1):129-140.
- Dhawale T, Steuten LM, Deeg HJ. Uncertainty of Physicians and Patients in Medical Decision Making. Biol Blood Marrow Tr. 2017;23(6):865-869.
- Pickles K, Carter SM, Rychetnik L, et al. General practitioners’ experiences of, and responses to, uncertainty in prostate cancer screening: insights from a qualitative study. PLoS One. 2016 Apr 21;11(4):e0153299.
- Arborelius E, Bremberg S, Timpka T. What is going on when the general practitioner doesn’t grasp the situation? Fam Pract. 1991 Mar 1;8(1):3-9.
- Campbell JI. Art and the uncertainty of medicine. JAMA. 2014 Dec 10;312(22):2337-2339.
- Han PKJ, Schupack D, Daggett S, et al. Temporal changes in tolerance of uncertainty among medical students: insights from an exploratory study. Med Educ Online. 2015 Sep 8;20:1.
- Evans L, Trotter DRM, Jones BG, et al. Epistemology and uncertainty in primary care: an exploratory study. Fam Med. 2009 Jan;41(5):319-326.
- Martinez JM. Managing scientific uncertainty in medical decision making: the case of the advisory committee on immunisation practices. J Med Philos. 2012 Feb;37(1):6-27.
- Hilfiker D. Healing the Wounds. 2nd ed. New York: Creighton University Press, 1985:61-63
- Cooke GP, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med Educ. 2013 Jan 7;13(1):2.
- Gerrity MS, White KP, DeVellis RF, et al. Physicians’ Reactions to Uncertainty: Refining the constructs and scales. Motiv Emot. 1995 Sep;19(3):175-191.
- Kuhn G, Goldberg R, Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann Emerg Med. 2009 Jul;54(1):106-113.
- Chew-Graham CA, Heyland S, Kingstone T, et al. Medically unexplained symptoms: continuing challenges for primary care. BMJ. 2017 Feb 23;67(656):106-107.
- Longhurst MF. Angry patient, angry doctor. Can Med Assoc J. 1980 Oct 4;123(7):597-598.
- Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student – a qualitative study of their reflective learning diaries and writing on specific themes during the first clinical year. Patient Educ Couns. 2010 Feb;78(2):218-223.
- Beresford EB. Uncertainty and the shaping of medical decisions. The Hastings Centre Report 1991;21(4):6-11.
- Engebretsen E, Heggen K, Wieringa S, et al. Uncertainty and objectivity in clinical decision making: a clinical case in emergency medicine. Med Health Care Philos. 2016 Jun 3;19(4):595-603.
- Montgomery K. How Doctors Think: Clinical Judgment and the Practice of Medicine. 1st ed. New York: Oxford University Press, 2013:35-36.
- Mukherjee S. Laws of Medicine. 1st ed. London, England: Simon & Schuster, 2015
- Beaman GB. Psychiatry in General Practice – Some Aspects of Fear. N Engl Med J. 1950 Dec 14;243:949-952.
- Han PKJ, Klein WMP, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Mak. 2011;31(6):828-838.
- Fosdick RB. Public Health and the Future. Am J Pub. 1948 Jan 1;38(1):185-189.
- Cernadas JMC. Embracing uncertainty and ignorance in medical practice. Arch Argent Pediatr. 2016 Apr;114(2):98-99.
- Djulbegovic B, Hozo I, Greenland S. Uncertainty in clinical medicine. In: Gifford F, ed. Handbook of the Philosophy of Science: Philosophy of Medicine. Oxford, England: Elsevier, 2011:299-356.
- Gerrity MS, Earp JL, DeVellis RF, et al. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol. 1992 Jan;97(4):1022-1051.
- Van Amber Brown G. Problems of ureteral surgery in gynecology. The American Journal of Obstetrics and Diseases of Women and Children. 1919 Jan 1;79(1):19.
- Huggins C. Endocrine control of prostatic cancer. Science. 1943 Jun 18;97(2529):541-544.
- Shinkins B, Perera R. Diagnostic uncertainty: dichotomies are not the answer. Br J Gen Pract. 2013 Mar;63(608):122-123.
- Freyhan FA. Observations and comments on European psychiatry. Am J Psych. 1956 Mar;112(9):673-677.
- Cooper BS. Anxious Patient and Worried Doctor. BMJ. 1958 Mar 8;1(5070):583.
- Dass D. The general practitioner – how much psychiatric education? Med J Malaysia. 1981 Dec;36(4):263-267.
- Middleton H. Distinguishing mental illness in primary care. BMJ. 2000 May 27;320(7247):1420-1421.
- Mechanic D. Commentary: Managing time appropriately in primary care. BMJ. 2002 Sep 28;325:687.
- ox RC. Training for Uncertainty. In: Merton R, Reader G, Kendall P, eds. The Student-Physician. Cambridge, Mass.: Harvard University Press, 1957:207-241.
- Brashers DE. Communication and Uncertainty Management. J Commun. 2001 Jan 10;51(3):477-497.
- Buetow S. The virtue of uncertainty in health care. J Eval Clin Pract. 2011 Aug 16;17(5):873-876.
- Schlozman S. Face It, Doctor, All Medicine Is Postmodern [Internet]. 2013 [cited 2019 Jul. 23];Available from: https://www.wbur.org/commonhealth/2013/06/24/post-modern-medicine
- Double D. The limits of psychiatry. BMJ. 2002 Apr 13;324(7342):900-904.
- Simpkin AL, Schwartzstein RM. Tolerating Uncertainty – The Next Medical Revolution? N Engl J Med. 2016 Nov 3;375(18):1713-1715.
SALLY MATHER, BMedSci, is a medical student at the University of Sheffield.
CHRIS MILLARD, PHD, is a lecturer in the history of medicine and medical humanities at the University of Sheffield. ORCID: https://orcid.org/0000-0001-5517-492X
IAN SABROE, MB BS, PhD, is a consultant respiratory physician at Sheffield Teaching Hospitals NHS Foundation Trust and an honorary professor of medical humanities at the University of Sheffield. ORCID: https://orcid.org/0000-0001-9750-8975
Summer 2020 | Sections | Doctors, Patients, & Diseases

Leave a Reply