Sherin Jose Chockattu
Bengaluru, India
His pole, with pewter basins hung,
Black, rotten teeth in order strung,
Rang’d cups that in the window stood,
Lin’d with red rags, to look like blood,
Did well his threefold trade explain,
Who shav’d, drew teeth, and breathd a vein
– John Gay (The Goat Without a Beard, 1727)
For over three millennia, self-taught physicians and barber-surgeons held the practice of bloodletting to a high regard and depended on it as the panacea for all maladies. It was not until the nineteenth century that this practice was phased out for more successful treatments. The history of the practice of bloodletting can be traced back to the ancient civilization of Egypt, 3000 years ago. The practice was continued by the Arabs, Indians, Greeks, and Romans. Centuries later, it was adopted by the Europeans in the Middle Ages and during the Renaissance.1
The most famous of ancient physicians, Hippocrates of Kos (c.460-c.370 BC), is credited with being the first person to believe that diseases were caused naturally, and argued that disease was not a punishment inflicted by the gods but rather the end-result of environmental factors, diet, and living habits. Unfortunately, with a societal prohibition on human dissections and the resultant rudimentary knowledge of anatomy and physiology, the philosophy of “Humorism” was widely accepted.2 Hippocrates surmised that the four basic elements of nature—earth, air, fire, and water— were complementary to the four basic humors in humans: blood, phlegm, black bile, yellow bile. He believed that menstruation functioned as a means to “purge women of bad humors.” Health was associated with a balance of humors (eucrasia). On the contrary, an imbalance (dyscrasia) or “corruption” of one or more of the humors, which could be caused by environmental circumstances, dietary changes, or many other factors was thought to be the direct cause of all diseases. Galen (129-200) advocated the teachings of Hippocrates, and promoted and practiced physician-initiated bloodletting. Believing that blood was the dominant humor, he surmised that it was the one in most need of control.3
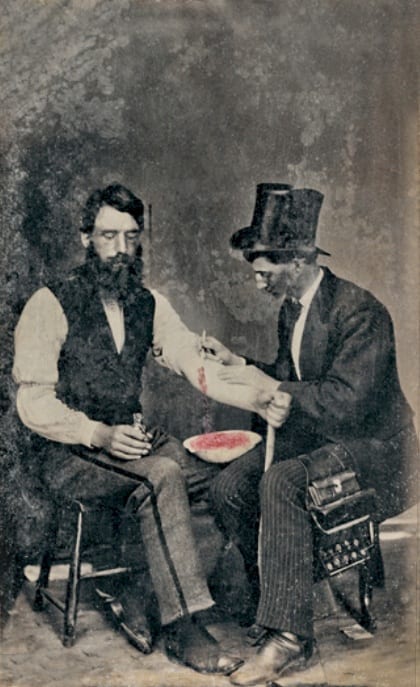
By the Middle Ages, Galen’s writings became the bible on bloodletting and this practice became accepted as the standard treatment for many conditions.4 Astrology was incorporated into the practice, whereby bleeding charts showed specific bleeding sites on the body in alignment with the planets. The barber-surgeon is one of those professions of antiquity that arose out of demand, as the early versions of the Hippocratic Oath discouraged physicians from practicing surgery.5 Barbers, whose trade inherently required the handling of sharps such as scissors and razors, were at the forefront in assisting monks who treated the sick by bloodletting. Their tools for superficial bloodletting were scarificator, vacuum cup, and hungry leeches. For venesection, fleams and lancets were used, and the blood collected into shaving bowls (“bleeding bowls”). In 1163, Pope Alexander III issued a decree that limited monks to caring for the soul, leaving bloodletting and dentistry for the barber-surgeons.6 Consequently, bloodletting became the craft and trade of barber-surgeons.7
The two trades were united by King Henry VIII, with the parliamentary act of 1540 that merged the Fellowship of Surgeons with the Company of Barbers to form the United Company of Barbers and Surgeons. At this point in time, surgeons could not perform barbery and barbers could not operate; the only exception being tooth extraction, which remained under the scope of both trades. It is no surprise that the dentist’s chair has an uncanny resemblance to that of a barber’s. For a time, barbers even received higher pay until surgeons gave their services aboard British war ships. Ambroise Paré (1510-1590), the best known of the barber-surgeons, is also the father of modern surgery.8
By 1745, the uncoupling was complete when King George II of England separated the two groups, with the surgeons forming the Company of Surgeons, later to be called the Royal College of Surgeons in 1800.8 Dentistry, which was still under the scope of the barber-surgeons’ ability, was also gradually relegated to its own specialty. Surgeon-dentists were practicing as early as the seventeenth century. Barbers, who had once performed an entire plethora of surgical procedures, were now primarily responsible for the care of hair and nails. Even so, the barber-surgeons’ skills remained in high demand as late as 1727, when John Gay penned his poem.9
The differences and cross-pollinations between the practices of surgeons and barber-surgeons play out across early modern literature and tell us about their cultural, civic, and occupational histories. The barber-surgeon is a trope in early modern literature because he had a tangible social impact and a historical meaning derived from his barbery and surgery roots.10 In modern times, the red and white “barber pole” is a stark reminder of the professions’ barber-surgeon ancestry. The barber-surgeon would wrap his bloody bandages (red) around the walking stick (white) that he carried for protection against highwaymen and used the stick also as a rest for the arm of his patient during phlebotomy.6,8
By the nineteenth century, bloodletting as a treatment modality was ubiquitous. Over one hundred diseases including acne, asthma, cancer, coma, convulsions, diabetes, epilepsy, gout, heart ailments, indigestion, insanity, jaundice, scurvy, stroke, bacterial and viral infections, and surprisingly even hemorrhage were indications. Before surgery, at the onset of childbirth, or before amputation, bloodletting was customary.11
As with the numerous staunch supporters of bloodletting through the millennia, there have been numerous detractors along the way. Erasistrateans disagreed with Galen and predicted dire outcomes from bloodletting, believing it was not blood but “pneuma” that flowed in the veins. Galen’s anatomical reports remained uncontested until 1543, when Andreas Vesalius published his seminal work De humani corporis fabrica with descriptions and illustrations of human dissections.12 In the year ca.1242, Ibn al-Nafis reported his discovery of the pulmonary circulation that challenged Galen’s theory of the physiology of the circulatory system.13 William Harvey’s discovery of the circulation of blood in 1628 proved to be a watershed moment in the field of hematology; human trials of blood transfusion were soon being performed in Paris and London.14 Meanwhile, bloodletting by venesection and leeching continued. The name of the most important bloodletting tool was adopted as the name of a respected medical journal today, The Lancet, founded in 1823.3
Pierre Charles Alexandre Louis demonstrated that phlebotomy was entirely ineffective in the treatment of pneumonia and various fevers in the 1830s. Some physicians resisted Louis’ work because their therapies were validated by both tradition and their own experience.15 Around the same period, van Helmont remarked that “A bloody Moloch presides in the chairs of medicine.” But his vigorous opposition to the use of bloodletting was based ironically on empirical claims—van Helmont believed that bloodletting concentrated the “impure” blood at the expense of the “pure” blood to the great detriment of the patient.16
A reason for the continued popularity of bloodletting was that while the knowledge of anatomy and surgical and diagnostic skills improved from the seventeenth century onwards, the means of curing most diseases remained elusive, and the underlying belief was that it was better to give any treatment than nothing at all. The placebo effect may have played a role. In the absence of other treatments, the simple act of reducing the blood volume in the body would have been beneficial in some circumstances such as hemochromatosis, the fluid overload of heart failure, and reduction of blood pressure. Bloodletting persisted into the twentieth century. It was recommended in the 1923 edition of the textbook The Principles and Practice of Medicine. By the 1920s bloodletting fell out of favor.3
In current times, bloodletting is in no way obsolete. Modern day bloodletting is amongst the noblest of deeds—every year, the Red Cross collaborates with thousands of sponsors worldwide to make blood donation easier for individuals.17 From being instituted on a purely empirical basis, to being associated with superstition and age-old scientific principles, the practice of bloodletting aimed at curing the self has finally metamorphosed into the noble act of blood donation aimed at healing one’s fellow human beings.
Bibliography
- Papavramidou N, Thomaidis, V, Fiska, A (2011). The ancient surgical bloodletting method of arteriotomy. Journal of Vascular Surgery. 54(6),1842-1844. doi: 10.1016/j.jvs.2011.05.100
- Garrison FH (1966). An Introduction to the History of Medicine. Philadelphia: W.B. Saunders Company.
- Thomas DP (2014). The demise of bloodletting. The Journal of the Royal College of Physicians Edinburg. 44(1),72–77. doi: 10.4997/JRCPE.2014.117.
- Brain P (1986). Galen on bloodletting: a study of the origins, development and validity of his opinions, with a translation of the three works. Cambridge: Cambridge University Press.
- Aggarwal A (2010). The evolving relationship between surgery and medicine. Virtual Mentor. 12(2)119-123. doi: 10.1001/virtualmentor.2010.12.2.mhst1-1002.
- Schmidt PJ, Ness PM (2006). Hemotherapy: from bloodletting magic to transfusion medicine. Transfusion. 46(2),166-168. doi: 10.1111/j.1537-2995.2006.00697.x
- Pang W (2016), William. Bloody history of barber surgeons. Medical Dialogue Review. Retrieved from https://www.mdrnyu.org/fall-2015-bloody-history-of-barber-surgeons/.
- Friedman SG (2018). Ambroise Pare: Barber vascular surgeon. Journal of Vascular Surgery. 68(2),646-649. doi: 10.1016/j.jvs.2018.04.053.
- Andrews W (2008). At the Sign of the Barber’s Pole: A Study in Hirsute History. NJ: Lethe Press. p.21.
- Decamp ES (2011). Performing Barbers, Surgeons and Barber-Surgeons in Early Modern English Literature. Pembroke College: University of Oxford.
- Kang L, Pederson N (2017). Quackery: A Brief History of the Worst Ways to Cure Everything. New York: Workman Publishing Company
- Siraisi NG (1991). Girolamo Cardano and the Art of Medical Narrative. Journal of the History of Ideas. 52(4),587-588. PMID: 11623014
- Majeed A (2005). How Islam changed medicine. British Medical Journal.331(7531),1486–1487. doi: 10.1136/bmj.331.7531.1486
- Magner LN (2020). The Beginnings of Blood Transfusion. encyclopedia.com, Retrieved from https://www.encyclopedia.com/science/encyclopedias-almanacs-transcripts-and-maps/beginnings-blood-transfusion/.
- Rangachari PK (1997). Evidence-based medicine: old French wine with a new Canadian label? Journal of the Royal Society of Medicine. 90(5)280–284. doi: 10.1177/014107689709000516
- Donaldson IM (2017).The ‘bloody Moloch’: Osler and van Helmont on bloodletting. The Journal of the Royal College of Physicians Edinburg. 47(2),196–204. doi: 10.4997/JRCPE.2017.221.
- Harris(2018). Power in the blood: local lifesaving partnerships between churches and the American Red Cross. Journal of Christian Nursing, 35(2), 120-123. doi: 10.1097/CNJ.0000000000000476.
SHERIN JOSE CHOCKATTU, MDS, is an Endodontist with 3 years of experience as a Clinical Lecturer. Sherin enjoys writing and has 12 scientific publications, out of which 6 are cited in PubMed Central.
Submitted for the 2019–2020 Blood Writing Contest and Highlighted in Frontispiece Volume 15, Issue 3 – Summer 2023

Leave a Reply