Adil Menon
Ali Mchaourab
Cleveland, Ohio, United States
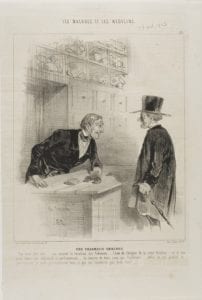 |
| A Pharmacy for Every Need (plate 24). Charles Émile Jacque. 1843. The Art Institute of Chicago. |
Within the past few decades, there has been a great change in how the pharmaceutical industry markets its products in the United States. Prices of medical drugs have skyrocketed as regulations have been eased by lawmakers. Granting more control to pharmaceutical companies has allowed the industry to bypass healthcare providers by going straight to the consumer. Pharmaceutical companies have increased their influence on the medical literature and been granted access and leverage in the political system.
Direct-to-consumer (DTC) marketing effectively exploits the concept of patient autonomy to undercut physician authority.1 It has been argued that only a country that strongly venerates rugged individualism and distrust for authority would allow direct marketing to flourish and allow the pharmaceutical industry to undercut physicians in order to advance their own interests. However, the stated purpose of such advertising is to “create an urgency to treat disease earlier and more aggressively” with the goal of producing a self-diagnosis that can be converted into a clinical one. Within this framework, doctors are presented not as medical experts capable of guiding the patient to the best decision, but rather “obligatory obstacles to be overcome.” Through policy shifts beginning in the 1980’s “clinical freedom became constrained by algorithms,” which compounded this diminution of physician authority relative to pharmaceutical companies.1 Through these policies, physicians fell prey to the DTC narrative: “the behavior of clinicians is… progressively less likely to be based on knowledge derived from direct clinical encounters.” Looking to these arguments regarding DTC marketing, it can readily be argued that these ad campaigns do little to truly empower patients while simultaneously serving to enervate physicians’ authority and the public’s perception of the profession. It is apparent that through this type of marketing and through the exploitation of the concept of patient autonomy, the pharmaceutical industry has assumed enormous power from physicians in almost every facet of practice. From education in their own field to decisions on diagnosis and treatment, the pharmaceutical industry seized much desired influence without the need to intervene directly.
The second dynamic of pharmaceutical interference relates to the medical literature. This is as much beholden to market pressures as any other industry and can create enormous conflict for journals as they make difficult choices, such as whether to “publish a trial that will bring US$100 000 of profit or meet the end-of-year budget by firing an editor.”2 The impacts of this tension are plain. In an analysis of 73 articles published in the New England Journal of Medicine, the Washington Post determined in its analysis that “60 were funded by a pharmaceutical company; 50 were co-written by drug company employees; and 37 had a lead author that had previously accepted outside compensation from the sponsoring drug company in the form of consultant pay, grants, or speaker fees.”3
This influence over the literature is compounded by direct authority over studies themselves. Here too, we see the consequences of the national faith in market forces, allowing industry pecuniary support for research to grow to such an extent that it now exceeds that of the National Institutes of Health (NIH). This in turn brings myriad opportunities for bias. For example, the structure of trials could be modified to present trial findings in a better light. Companies can hand pick researchers motivated to work for their interests, and perhaps most troubling, can effectively bury negative or hazardous results. These concerns have already borne empirical fruit. The odds of deriving results in favor of industry interests are 3.6 times greater in research sponsored by the industry than in research sponsored by government or nonprofit groups.4 As companies fund a larger share of research, they have shifted the job of conducting trials away from nonprofit academic hospitals towards for-profit “contract research organizations,” making pro-corporate bias even less likely to be challenged. As summarized by Joseph Ross, a professor at Yale Medical School, because of all these influences “the entire evidence base has been perverted.”5
Also making America distinctively vulnerable to pharmaceutical influence is its unique structure of election financing. In addition to raising money for their own campaigns, members of Congress are expected to raise funds for their party. This means their priorities and daily schedules become beholden to fundraising. This has allowed the pharmaceutical industry to deploy its enormous charm and financial resources to offer spectacular returns on investment by becoming a major player in the United States politics. Election records demonstrate that pharmaceutical manufacturers spent “a grand total of $21.3 million on federal elections in 2012, which is 407 percent more than the 1990 inflation-adjusted total.”6 This money has proven well spent given that its profits depend in large part on several industry-specific federal policies. Such policies include profitable patent protection and market exclusivity for new products, lack of price controls, and a selective suppression of competition.6 While the advantages granted to drug makers are nominally meant to promote the public good, the industry has influenced the system to an extent that these advantages no longer apply in a system of overly expensive and protracted elections.
These factors deserve consideration in the face of the seeming retreat of the pharmaceutical industry from marketing and education for physicians, as well as the reductions in the pharmaceutical representative workforce. In the place of these overt gestures have emerged far more influential methods of exerting the industry’s bidding: Influencing patients, legislation, and medical literature. Such tactics have proven uniquely effective in the American context by exploiting the central values and unique institutions of this nation. One can hope that wisdom will prevail and that appropriate reforms will counter the influence of the pharmaceutical industry and benefit the American public.
References
- Joseph Dumit. Drugs for life: how pharmaceutical companies define our health. Durham, NC: Duke University Press, 2012.
- Lexchin, & Light, D. W. (2006). Commercial influence and the content of medical journals. BMJ: British Medical Journal, 332(7555), 1444–1447.
- Peter Whoriskey. “As drug industry’s influence over research grows, so does the potential for bias.” The Washington Post. November 24, 2012. Accessed January 16, 2017. https://www.washingtonpost.com/business/economy/as-drug-industrys-influence-over-research-grows-so-does-the-potential-for-bias/2012/11/24/bb64d596-1264-11e2-be82-c3411b7680a9_story.html?utm_term=.c16ca6abb61e
- Daniela Drake, “Big Pharma Is America’s New Mafia.” The Daily Beast. February 21, 2015. Accessed January 16, 2017. http://www.thedailybeast.com/articles/2015/02/21/big-pharma-is-america-s-new-mafia.html
- Vera Sharav. “Can Medical Research be Trusted?” AHRP. November 21, 2014. Accessed January 17, 2017. http://ahrp.org/can-medical-research-be-trusted/.
- Paul D. Jorgensen, “Pharmaceuticals, Political Money, and Public Policy: A Theoretical and Empirical Agenda.” The Journal of Law, Medicine & Ethics 41, no. 3 (Sept. & oct. 2013): 561-70. Accessed January 15, 2017. doi:10.1111/jlme.12065
ADIL MENON, MBE, is a medical student at Case Western Reserve School of Medicine. Before medical school he received his Master of Bioethics degree from Harvard Medical School. His written work may be found in Hektoen International, HMS Bioethics Journal, and JAMA Cardiology.
ALI MCHAOURAB, MD, is Associate Professor of Anesthesiology at Case Western Reserve University School of Medicine. He was the Chief of Pain Medicine at the Cleveland VA Health Care System between 2003 and 2018. Dr. Mchaourab has championed a reduced reliance on opioids for well over a decade and has been recognized nationally for his work in this field.

Leave a Reply