Charles Paccione
Oslo, Norway
The global burden of chronic pain is large and growing. About 25% of patients treated at primary care settings throughout Asia, Africa, Europe, and the Americas report persistent pain and as many as 1 in 10 adults are newly diagnosed with chronic pain each year.1 Nearly half of those being treated receive inadequate pain relief, report a myriad of treatment-related adverse side effects, and suffer from a variety of psychosocial issues.2 Due to the complex cross-cultural and biopsychosocial nature of pain, healthcare professionals need to understand pain as it is defined culturally and socially by those who suffer from it. Medical anthropology may aid in conceptualizing pain as a social and cultural phenomenon, offer effective approaches to communicating with families, and assist them in coping with the difficult challenges they face during pain treatment.
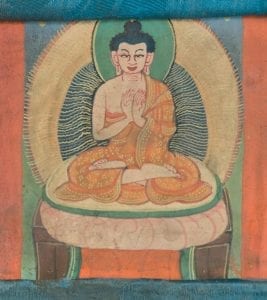
The anthropological approach to pain treatment and management can aid health care professionals and patients by embodying what Dr. Sienna Craig refers to as bricoleur: “. . . engaging in the creative and resourceful practice of using whatever resources [are] available, sometimes despite their initial or intended purpose, to effect change.”3 In her book Healing Elements: Efficacy and the Social Ecologies of Tibetan Medicine, Dr. Craig describes how medical anthropology can serve as a vital tool for the exploration of the ways pain and suffering can be both expressed and addressed within the clinical encounter. She investigates what it means for a medicine to “work” and how this efficacy is determined. Through her close work with the amchi she determines that efficacy is not only dependent on clinical and pharmaceutical interventions but also on environmental, political, economic, and historical factors.
In order to unearth and negotiate how pain is conceptualized culturally, politically, and socially, Dr. Craig follows healers, students, and administrators of Tibetan medicine throughout the land, from patients’ homes to established clinics, and produces what McGranahan refers to as “thick descriptions”: descriptive research that “. . . is not simply to watch people or interview someone or assemble a focus group or ‘shadow’ someone, but a much more all-encompassing and demanding way of knowing.”4 Dr. Craig’s work with Dr. Namlha Khr, a Tibetan doctor who specializes in gastrointestinal disorders and internal medicine, offers many such descriptions. During one encounter, Dr. Namlha listens to a patient and his father express both pain and suffering: “I have pain on this side. . . .His stomach is swollen and has noises in it. After he eats cold foods or drinks anything, the pain gets worse.”3 Dr. Craig is not a passive observer of such an encounter—she becomes an active witness to how Dr. Namhla transforms listening into the art of touch. Dr. Namlha decides to listen more to the pulse than to the words of his patients, “. . . concentrating through his fingers, through touch . . .” 3
The act of touch utilized by the traditional healers of Tibet can be viewed as a technology—a method of investigation with a particular degree of sensitivity. In Western medicine, touch is also used as a method to evaluate discomfort and pain, yet the mission differs: mainstream medicine may utilize touch to discover a degree of pain sensitivity, whereas touch can be used in Tibetan medicine to go beyond the pain and toward the pulse. Recent research investigating the effectiveness of therapeutic touch on pain severity, depression self-assessment scores, and sleep quality seems to be promising for those with chronic non-oncological pain.5 One commonality between the medicine of the East and West with regard to pain is an understanding that the pain felt in the moment is defined and characterized by the pain felt in the past.
Dr. Craig describes how the suffering and pain of the patients she encounters is based on what is happening in the present, but also what has happened in the past. A patient she meets describes how his pain transcends time: “I have a lot of pain, but I can’t be free of it. I am thinking about the problems from my previous life. . . . It is also a lu and sap dak problem because of the work that I have done in the earth, in my younger years . . .”3 A past history of childhood trauma, bouts of depression, and anxiety are all known to contribute to the current severity and expression of pain within an adult.6 Yet Dr. Craig’s patient describes not only his karmic inheritance, but also his possible disturbance of serpent and earth spirits in relation to his suffering. This speaks to the bio-historical quality of pain, but also to the quality of certainty for the patient.
In Improvising Medicine: An African Oncology Ward in an Emerging Cancer Epidemic, author Julie Livingston refers to Elaine Scarry’s proposition that pain is an individually held experience that can “shatter language.”7 Patients who suffer from long-term pain often have difficulty describing their pain and its multidimensionality in words. Therefore, in order to “know” their pain, some patients tend to seek the spiritual and energetic realms of its character. However, as a clinical research within the field of pain medicine, I must disagree with Scarry’s notion that pain simultaneously produces certainty in the person who experiences it and doubt in the onlooker.
Certainty and uncertainty are shared bidirectionally and simultaneously between caregiver and patient. The illness uncertainty theory proposes that patients with a chronic illness, such as chronic pain, have difficulty adjusting to the illness if there is significant diagnostic or prognostic uncertainty. Two dimensions of illness uncertainty theory are: lack of information about diagnoses or severity of the illness; and complexity regarding the health care system.8 I do resonate with Scarry’s notion that the dynamic of the clinical encounter gives way to a series of ethical problems around what to do about pain as an object located in an individually bounded body. If we were to explore, rather than simply disregard, Scarry’s notion of “certainty within the onlooker,” pain research has produced a wide array of findings that seem to produce some degree of certainty regarding the biochemistry of pain.
Livingston’s notion that ethnography may be a valuable means of providing a visceral, intimate, and sensorial awareness of suffering is important to consider when exploring the capacity to communicate pain with clarity: “. . . what it would be like to be in extreme and serious bodily distress, groping for some communicative possibility that will bring relief to you . . .”8 But this is not only applicable to exploring the psychophysiological states of patients in pain. Livingston shares how ethnography can also help describe what it would be like to work as a professional healthcare provider in a chronically overwhelmed hospital. In particular, Livingston questions the absence of numerical pain rating charts, which are widely used within both American and European healthcare institutions.
The subjective nature of pain makes objective measurements very difficult to perform. Acute pain can be reliably assessed, both at rest and during movement with one-dimensional tools such as numeric rating scales or visual analogue scales. Both of these methods are in fact more powerful in detecting changes in pain intensity than verbal categorical rating scales. However chronic pain assessment and its impact on physical, emotional, and social functioning requires multidimensional qualitative tools and health-related quality of life instruments with a much more complicated format.9 Numerical pain rating charts are not sufficient to describe the character and quality of a patient’s experience of pain. An anthropological approach to understanding the influence of coping strategies, pain acceptance, pain tolerance, anxiety of pain, and fear-avoidance behavior is useful in evaluating the patient’s experience.
A paradigm shift, from mainstream medicine to integrative medicine, may help with navigating the psychosomatic complexities of chronic pain. Tibetan medicine acknowledges the psychophysiological and spiritual domains of pain foundationally, yet Western medicine is still on its way to adopting such an approach. Current research in placebo, treatment expectations, and psychoneuroimmunology have been producing groundbreaking work on the mind-body connection and how this connection may be modulated in the face of pain. Instead of thinking that there is something “wrong with the patient,” healthcare providers may begin to see that there is something wrong with the systems within that person. This shifts the responsibility from the suffering person and reconfigures treatment expectations and goals.
Agony and suffering in the face of pain is created out of a complex political, economic, technocratic, and cultural history. In order to meet that suffering with effective approaches to treatment and management, healthcare providers must build treatments based on the values and desires of the target population. Livingston notes that while the chemical tools of palliation may be standard, the circulation, distribution, and application of drugs, as well as the politics and logistics surrounding them, vary tremendously across clinical contexts. Therefore, ethnography may aid in sharpening and contextualizing the complexities of drug policy while also “. . . reminding us that biomedicine is localised practice as much as it is a global system of thought and technology.”8 If we are to successfully and holistically treat patients in pain, we must understand that pain is influenced by culture, language, politics, and history. Medical anthropology offers caregivers new tools to redefine what it means to treat pain and help patients successfully navigate a life in the face of illness.
References
- International Association for the Study of Pain: Unrelieved pain is a major global healthcare problem. [http://www.iasp-pain.org/AM/Template.cfm?Section=Home&Template=/CM/ContentDisplay.cfm&ContentID=2908]
- Breivik, Harald, et al. “Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment.” European journal of pain 10.4 (2006): 287-287.
- Craig, Sienna R. Healing elements: efficacy and the social ecologies of Tibetan medicine. Univ of California Press, 2012.
- McGranahan, Carole. “What is ethnography? Teaching ethnographic sensibilities without fieldwork.” Teaching Anthropology 4.1 (2014): 23-36.
- Marta, Ilda Estefani Ribeiro, et al. “The effectiveness of therapeutic touch on pain, depression and sleep in patients with chronic pain: clinical trial.” Revista da Escola de Enfermagem da USP 44.4 (2010): 1100-1106.
- Sansone, Randy A., Daron A. Watts, and Michael W. Wiederman. “Childhood Trauma and Pain and Pain Catastrophizing in Adulthood: A Cross-Sectional Survey Study.” The Primary Care Companion for CNS Disorders 15.4 (2013): PCC.13m01506. PMC. Web. 11 Jan. 2018.
- Livingston, Julie. Improvising medicine: an African oncology ward in an emerging cancer epidemic. Duke University Press, 2012.
- Fishbain, David A., et al. “Exploration of the illness uncertainty concept in acute and chronic pain patients vs community patients.” Pain Medicine 11.5 (2010): 658-669.
- Haefeli, Mathias, and Achim Elfering. “Pain Assessment.” European Spine JournalSuppl 1 (2006): S17–S24. PMC. Web. 11 Jan. 2018.
CHARLES ETHAN PACCIONE is a Ph.D. Fellow in Medicine and Health Sciences at the Department of Pain Management and Research at Oslo University Hospital in Oslo, Norway. He holds his M.S. in Narrative Medicine from Columbia University’s School of Professional Studies and his M.A. in Psychology in Education from the Spirituality Mind-Body Institute, Teachers College, Columbia University. He currently specializes in developing innovative psychophysiological treatments for patients suffering from chronic widespread pain. is author bio.

Leave a Reply