Anabelle S. Slingerland
Leiden, Netherlands

The discovery of insulin in 1921 by Banting, Best, Collip, and McLeod was heralded as the cure of diabetes (Figure 1). Press reports consigned earlier research to oblivion, suggesting that previous investigators had merely been groping in the dark. And yet this revolutionary discovery was preceded by legions of key figures and unsung heroes, lost observations, and non-acknowledged literature.
Early days
Tradition ascribes the first observations on diabetes to Aretaeus of Cappadocia (1st or 2nd century AD) with his famous description of the flesh wasting into the urine. He noted that it passed by the kidneys and the bladder as through a siphon, that the disease was chronic and death speedy. Even earlier, around 400 BC, Susruta in India had made a connection between diabetes and the role of glucose by referring to “honey urine.” Thomas Willis in 1674 noted that diabetic urine had a sweet taste; and Matthew Dobson (1776) evaporated urine and found it had the appearance and taste of “brown sugar.”
Over time several organs were thought to be the cause of diabetes: the kidneys at first, because of the sweet urine; and the liver, because it was enlarged. John Rollo and Cruickshank opted for the gastrointestinal tract as the culprit, speculating that it broke down food into glucose under the direction of the central nervous system.
Diabetes and the pancreas
In 1788, Cawley described stones and shrinkage of the pancreas in diabetics but did not yet make the causal connection. Claude Bernard in 1830 and Moritz Schiff in 1880 came closer to the mark. They discovered that blocking the pancreatic ducts in dogs induced atrophy, an important clue. They showed that glucose was derived from glycogen, but fell short of the target because the atrophy of the pancreas did not lead to diabetes.
Between 1835 and 1875, Bouchardet added muscular work-outs to Rollo’s diet and found that some subjects did not respond to diet and physical activity as much as others. Publishing his findings as “De la glycosuria ou diabète sucrée,” he and Lancereaux linked pathology to clinical findings and differentiated between “diabète maigre,” whose thin victims’ affliction was attributed to the pancreas, and “et gras” whose sufferers tended to be older and obese. By reexamining previously disregarded findings, Berthold (1849) and Brown-Sequard (1855) studied Addison’s disease and adrenal glands, discovering that some glands were ductless and secreted in the bloodstream. Paul Langerhans (1847-88), as part of his medical dissertation in Berlin, described “masses 0.12-0.24 millimeters in diameter” occurring “at regular intervals in the parenchyma” and unconnected to the excretory ducts.
Langerhans’ masses remained unattended and Langerhans himself died in 1888, but one year later von Mering, in Strasbourg, studied the role of the pancreas in fat absorption. Though not interested in diabetes itself, he used the surgical skill of Minkowsky to remove the pancreas of a dog. This latter assistant to Naunyn, the foremost European clinician in diabetes, did recognize the polyuria in the depancreatized dog as indicative of diabetes. In subsequent experiments subcutaneous implantation of pancreatic tissue made diabetes disappear. Thus in 1889, after a long odyssey through history and across cultures, Mering and Minkowski discovered what we today take for granted: the cause of diabetes lay in the pancreas.
The islets of Langerhans and insulin
Between 1891-94, Hedon in France repeated the 1889 findings of Mering and Minkowski, and Laugesse restudied the islets, baptizing the interacinar cell collections as the “islets of Langerhans.”
At the turn of the century, Liebig’s student, Max Rubner, had teamed up with Graham Lusk, Atwater, and Benedict to link clinical cases to energy metabolism. In 1902, Ernest Starling coined the term hormone to describe a chemical material secreted by ductless glands that would exert a specific functional change on target tissue elsewhere. Opie and contemporaries considered the islets endocrine glands, and Jean de Meyer considered the hormone secreted by the “insulae,” naming it “insulin.” Thus the genesis of insulin’s name.
Insulin as a tool to reverse pathology
Soon the islets and insulin were of interest as the key to reversing diabetes in the depancreatized dogs—paralleled by new histological and chemical techniques. However, unaware of insulin being a potent protein, scientists misinterpreted hypoglycemic convulsions as a side effect, and thus kept failing at oral administration. Many came close. Scott, Kleiner, Zuelzer, Paulesco had been very successful with animal subjects but not with humans. A fortunate coincidence occurred when Barron observed a patient’s stone that had blocked a pancreatic duct and caused atrophy of the acinar pancreas but not of the islets. A slight indication of Langerhans ductless islets.
Insulin as therapy – Toronto 1921
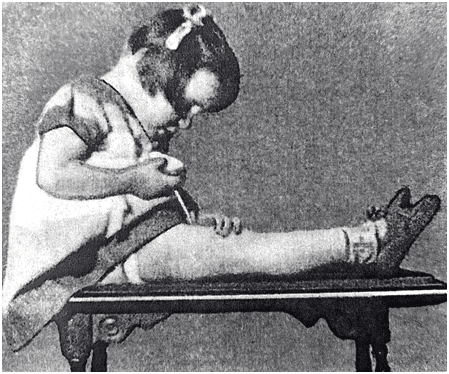
Success came in the summer of 1921 at the University of Toronto thanks to the perseverance of young Frederick Banting, working with Charles Best (a skilled medical student), Collip (the chemist who purified the insulin), and Professor Macleod (knowledgeable in basic science and first to suggest destroying the pancreatic enzymes in the extract with alcohol). They were able to show that a duct-ligated pancreas lost its function after atrophy. They also demonstrated that actively injecting insulin revived the patient. With the microanalytic techniques available at the time, they were able to measure glucose in small amounts of blood and trace reduction of glucose levels by insulin much more closely than had been possible by measuring glucose in urine. Leonard Thompson, age fourteen, became the team’s first patient in January 1922. They published their results in March. Newspapers spoke of a cure for diabetes and even children were taught to inject themselves (Figure 2). Michael Bliss later described this in The Discovery of Insulin (1982) as “one of the most dramatic events in the history of the treatment of disease.” And the microanalytic techniques that made measuring blood glucose possible would soon enable patients to monitor themselves.
Insulin’s implementation & Eli Lilly
Soon insulin was provided throughout the USA, but in unregulated, private production with spotty success. Immediate drawbacks were access, contamination, and overdosing. One injection a day could cause hypoglycemia and subsequent overeating. Insufficient supplies caused insulin-dependent patients to succumb to acidosis and die. The question was, who would win the insulin raffle?
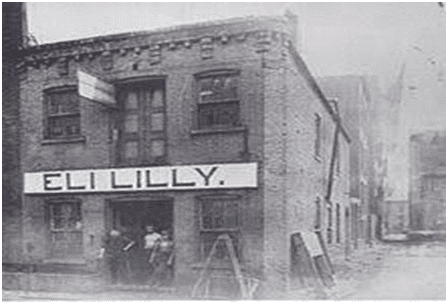
Eli Lilly and his company of Indianapolis were the first to tackle the problems of availability and contamination of this life-saving substance (Figure 3). He would supply the American market and refine insulin of higher potency from animal sources.
British patient R.D. Lawrence’s experience demonstrated the unmet need. Lawrence had started injecting insulin in early 1923. Shortly after he began, his month’s supply was diverted to a doctor’s daughter who had fallen into a diabetic coma. While his life was in jeopardy, an insulin bottle miraculously arrived from the USA just in time to save his life. He later became a leading physician in the field.
In summer 1923, almost two years after its discovery, Eli Lilly chose six physicians for the North American Insulin Committee to conduct the first clinical trials.
In Europe, the Nobel Laureate in Physiology of 1920, August Krogh of Copenhagen, learned about insulin when invited to give a talk at Yale University in the autumn of 1922. His own wife was diabetic. When she saw patients with type 1 diabetes in her own medical practice, she suggested that her husband contact Toronto to learn how to manufacture insulin. She herself contacted her colleague, Dr. Hans Christian Hagedorn, who was willing to experiment. Hagedorn in turn contacted the Danish pharmacist August Kongsted for financial aid. They started at Hagedorn’s house, and followed up at Krogh’s Institute, the Laboratory of Zoophysiology, to extract their first small quantity of insulin. They treated their first patients in spring 1923, and the Nordisk Insulin Laboratory opened in 1923.
Nobel Prize, 1923
On October 25, 1923, Banting and Macleod, the seniors, received the Nobel Prize, which they immediately shared with their junior colleagues. Minkowski appreciated the historic moment and attributed their success to parallel discoveries: the measurement of blood glucose, unlimited supply of pancreatic extract, their ignorance of the toxicity of their abstracts, which made them more daring, and relentless determination.
American Diabetes Association, 1937
The six doctors of the North American Insulin Committee collaborated over the next decades. Their cumulative work led to the founding of the American Diabetes Association (ADA) in 1937. Further refinement and purification of medical insulin would continue through the 1950s. The ADA has continued to evolve. On a yearly basis it still organizes the largest international conference on diabetes in various cities in the United States.
Spin-offs
The journey towards the discovery of insulin as a therapeutic agent led to discovering the role of hormones and their delivery mechanisms. This pioneering work set the stage for research on other diseases in related fields. In 1936, Fischer and Hagedorn added zinc to protamine insulin (PZI) for prolonged action. In 1942-45, sulfonamides were shown to release endogenous insulin. As a result, patients not dependent on insulin, later denoted as having type 2 diabetes, could be treated without injections. Hagedorn with Nordisk Company developed NPH Neutral-Protamine-Hagedorn insulin with controlled amounts of protamine in 1950. At the same time, the first sensitive bioassay for insulin became available. Dr. Chick cultured beta-cells and, collaborating with Harvard researchers, engineered the first human insulin gene in bacteria. In 1959, the whole protein’s amino acid sequence became known and in 1963, insulin was synthesized as the first protein. Another decade later, the first 3D structure became known in parallel developments in X-ray crystallography. In 1977 insulin was the very first protein cloned, and in 1979 insulin was the first (Lilly 1982) commercialized recombinant DNA product. In 1980 insulin was the first to be cloned as part of the human genome.
Insulin facilitated understanding the roles of the pituitary, thyroid, and adrenal glands (Houssey), intermediary metabolism (Cori, Krebs), and correction of acidosis (Atchley and Loeb). In 1980, correcting the insulin deficit became part of the American Diabetes Association guidelines.
Downturns
When diabetics began to live longer, this led to new challenges. In 1921 Joslin’s article “The Prevention of Diabetes” had fallen on deaf ears. The call for prevention of a disease that now had a “cure” was less urgent. Medical insulin’s abundance had paradoxically failed to eliminate the problem of determining which patients should receive it. Who should forgo insulin and treat the condition with strict diet and exercise instead, even though this course of treatment required more effort on the patient’s part?
From death sentence to chronic condition
The ever-evolving understanding of diabetes has resulted in many insulin refinements, products, and advanced tools. Thanks to insulin, diabetes no longer causes sudden death. Thanks to insulin, the stereotype of the diabetic has morphed from a debilitated, bedridden patient to that of a productive individual capable of living a full and productive life. Thanks to insulin, diabetics survive even though, regrettably, their disease endures. Instead of being almost always a death sentence, diabetes has become a manageable chronic condition.
Dr. Feutner describes the transformation of diabetes in his book Bittersweet. Clinicians now have a longer time frame to observe and treat patients over the course of many years, enabling them to focus on improving and refining treatment as they seek to improve patients’ lives. Insulin’s discovery was neither a magic bullet nor the perfect cure. Nevertheless, there is no dispute that it has enhanced and prolonged lives. Physicians and researchers hope to build on past discoveries to finally fulfill the American Diabetes Association’s mission to rid the world of this malady.
Note
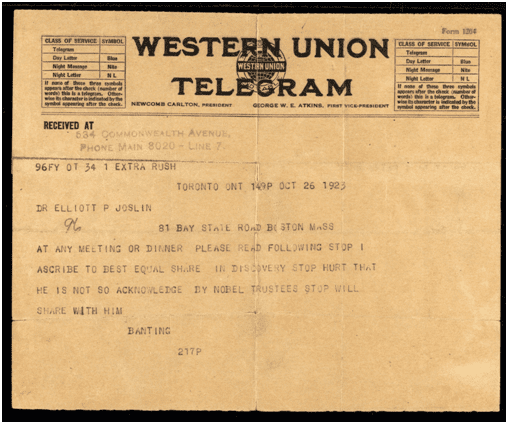
No history of the discovery and use of medical insulin would be complete without invoking the protagonist who was present in every scene of the script, Dr. Elliott P Joslin. He began by translating the work of Mering and Minkowski, and became the first diabetologist in the United States, as well as one of the initial six members of the Insulin Committee, and regarded Banting as his father figure. When he invited Best to give a speech at Harvard he read aloud to Best the telegram in which Banting announced that he would share the Nobel Prize with him (Figure 4). Please also see further information in the article on the Joslin Diabetes Center in the fall 2017 issue of this journal.
Literature
- A brief history of diabetes from 1891 to 1988 through the publications of the Joslin Diabetes Center, Dr Donald M. Barnett.
- Dr Joslin’s Magnificent Obsession, Dr Donald M. Barnett.
- Elliott P. Joslin, A Centennial Portrait, Dr Donald M. Barnett.
- Joslin’s Diabetes Mellitus, 13th Ed. Edited by Drs C. Ronald Kahn and Gordon C. Weir. Chapter 1.
- The history of Diabetes, Leo P. Krall, Rachmiel Levine, Donald Barnett. P1-14. Lea & Febiger. Malvern, Pennsylvania, USA, 1994.
- The Discovery of Insulin. Michael Bliss. McClelland & Stewart Inc. Toronto, Canada, 1982.
- Insulin: Molecular Biology to Pathology, Frances M. and Stephen JH Ashcroft, Oxford University Press, 1992.
- The Breakthrough, Elizabeth Hughes, the Discovery of Insulin and the Making of a Medical Miracle. Thea Cooper and Arthur Ainsberg. St. Martin’s Press, New York, USA, 2010.
- Diabetes, The Biography. Robert Tattersall. Oxford University Press Inc. , New York, 2009.
- The Personal Story of Dr. Charles Best, Co-Discoverer of Insulin. Best, Henry B.M. Margaret and Charley. Dundurn Press, Toronto, Canada, 2003.
- Selected Papers of Charles H. Best. Toronto: University of Toronto Press, 1963.
- Bittersweet: Diabetes, Insulin, and the Transformation of Illness. Chris Feudtner. The University of North Carolina Press, USA, 2003.
ANNABELLE S. SLINGERLAND, MD, DSc MPH, MScHSR, earned her medical degree from the University of Health Services Research and Genetics from Erasmus University in Rotterdam. She has worked and collaborated internationally, and (co-) authored research articles in high impact medical journals.

Leave a Reply