Sophia Newman
Chicago, Illinois, United States
The shot against sleeping sickness brought me so many problems
The shot against sleeping sickness hurt me so…
They pricked me in the back…
And still, they want to send me to draw water
If I try to slow my step
The policeman hits me on the head with a stick.1
This song, originally sung in the Eton language of Lekié, central Cameroon, in the 1950s, refers to a public health campaign against a disease called African trypanosomiasis. The disease, which is spread by the tsetse fly, is characterized by fever, aches, and then a slow neurological breakdown that involves sleeping difficulties. Without treatment it is invariably fatal – but as the song suggests, the difficult experience of being injected with a preventive drug might have provoked collective anxiety on a par with public fear of the disease itself.
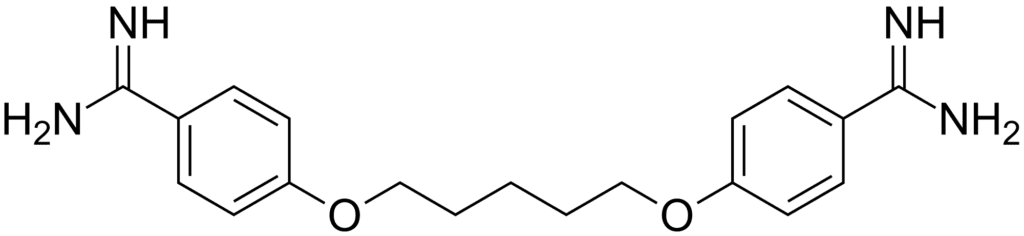
This is part of the story that anthropologist and University Paris-Diderot lecturer Guillame Lachenal tells in his newly translated book, The Lomidine Files: The Untold Story of a Medical Disaster in Colonial Africa. The book recounts a long-standing but eventually discontinued public health outreach program in which small bands of European clinicians, often assisted by African colleagues, traveled through West and Central Africa to vaccinate whole villages against the Trypanosoma brucei parasite. The program was meant not only to treat existing cases but to prevent new ones, thus helping to eradicate the then-endemic disease. According to Lachenal, the process did much to justify the strongest doubts of those who sang about sleeping sickness shots.
His book, which he terms “a biography of Lomidine,”1(p2) describes its impact on colonial sub-Saharan Africa. As with many circumstances in global health history, it is a story that contains congruences and contrasts to the dramas that have played out with the exact same drug – now better known by its current name, pentamidine – in the modern era.
The trypanosomiasis vaccination program was based on the belief that providing whole villages with intramuscular injections of Lomidine would act as an effective prophylaxis against spread of the disease. What it would take to achieve eradication was not easy, however. The drug was known to cause immediate adverse effects in anyone who received it, with symptoms ranging from hypoglycemia to nausea, vomiting, and fainting. It was not rare, Lachenal says, for clinicians to line up supine patients on the ground outside the immunization tent as they waited to outlast the disabling effects of the injection. Understandably, the colonial demand that everyone living in a district drop what they were doing to come receive the drug every three months was often unpopular – so much so that the colonial governments found it necessary to use everything from ad campaigns (“Those who refuse to receive this shot… are bad brothers and bad Cameroonians!”1(p105)) to, as the Eton-language song suggests, armed guards.
What was worse, says Lachenal, was the deadly outcome of the injection campaigns. The Lomidine Files recounts incidents in which the immunization process caused multiple fatalities. On November 12, 1954, for instance, a vaccination team near Yokadouma, a town in eastern Cameroon, injected over five hundred people. Of these, more than 300 soon experienced gas gangrene that began in the muscles of their buttocks, where the drug had been injected. Thirty-two swiftly died.
As that incident unfolded, a crowd gathered at the hospital. “The population has crowded in front of the dispensary – dispersion is delicate and difficult,” a report to the French ministry would later describe.2 Other local peoples converged on the house of the foreign team’s lead physician, a man named Ansellem. “Threats – screams – rocks thrown,” the report tersely noted.2 Although antibiotics had already begun to heal many of the gangrene-afflicted individuals, Ansellem was overwhelmingly unwelcome. Indeed, he would soon leave Africa altogether.
Lachenal cites documents from Belgian and French colonial ministries to explain that these outcomes arose not from Lomidine per se, but rather from the use of poorly filtered water to prepare the drug for injection. In Europe, the drug was already available as a sterilized solution; in Africa, supplies had been prepared and shipped in powder form, in a colonial judgment that had valued lower costs over safety.
The nonharmful status of the pharmaceutical itself meant little to those who had lost loved ones to fatal injections – and what was worse, the incident in Yomadouka was not the first time that the use of Lomidine had resulted in deaths. Relying on the brief comments that remain in official reports, The Lomidine Files notes that fatalities were reported in the early 1950s in Abong-Mbang, Bafia, and among the Eton people, all in Cameroon; and in Nkoltang, Gabon, where fourteen people had died from the same cause in December 1952.
In some ways, November 1954 was an inflection point in the history of the drug. “In Cameroon, the shock of the accident of Yokadouma had led to an interruption of campaigns across most of the territory,” Lachenal writes.1(p168) Most other countries were doing the same, albeit for other reasons. By the late 1950s, several more countries had begun to slow vaccination or narrow the territory in which it occurred, because research had shown that the number of sleeping sicknesses cases was in rapid decline. In 1958, Belgian physician Georges Neujean wound an acknowledgment of Lomidine’s lethality together with that epidemiological success when he wrote that immunization campaigns were only valuable “as long as we are guaranteed to be able to see them through, because we knowingly sacrifice individuals” – by which he meant end their lives – “in the aim of solving a collective problem.”3
Seeing them through was no longer guaranteed, though; Neujean’s call to eradication would remain in vain. Postcolonial independence dawned across West and Central Africa in the late 1950s through the 1960s, bringing with it a vast renegotiation of the programs colonial powers had once brought to the continent. The countries that European powers had once ruled had aims of their own and with memories of painful, coercive, and sometimes fatal injections fresh in mind, their populations typically preferred other goals to trypanosomiasis control. Fourteen deaths by injection of contaminated water in Goro, Chad, in 1965, were the final nails in the coffin for immunization, not least of all because researchers had begun to admit that the preventive power of Lomidine was in serious doubt.
In fact, the drug now called pentamidine is understood to only treat active cases of trypanosomiasis and, because it cannot cross the blood-brain barrier, it is effective only in early stages of the disease.4 The Centers for Disease Control and Prevention website states it bluntly: “There is no vaccine or drug for prophylaxis against African trypanosomiasis.”5
The uses of pentamidine have since expanded, however. In the mid-1980s, the dawn of the AIDS crisis brought with it a surfeit of men and women affected by Pneumocystis jirovecii pneumonia. The parasitic infection was often lethal in people with weakened immune systems, and the quest for an effective drug brought AIDS researchers to pentamidine isethionate. “Pentamidine is clearly effective in the treatment of PCP [Pneumocystis carinii pneumonia, another name for Pneumocystis jirovecii],” Drake et al concluded in a 1985 study published in Clinical Pharmacology.6
Its role in medical history was more complicated than the simple provision of treatment. Like other medications, pentamidine became a flashpoint in the political struggles of people with HIV and AIDS. In 1987, AIDS activists protested a tripling of the price for doses of the drug by its sole American supplier, a Chicago firm called Lyphomed. That year, the AIDS Coalition to Unleash Power (ACT UP) declared the “Pentamidine Wars,”7 and engaged in actions ranging from chaining themselves to Lyphomed’s gates to importing the drug from Mexico to seeking out interventions from the federal government. But unlike other, similarly conflicted drugs (such as the ultimately abandoned experimental substance Compound Q), pentamidine was effective – and therefore one of the first such medications used for the opportunistic infections common to people with AIDS.
It was arguably also a drug that changed the relationship of AIDS activists and the pre-eminent institutions that worked to treat their disease from adversaries to collaborators. By June 1989, pentamidine was once again being advanced as a preventive drug. A task force of researchers from the US National Institutes of Health proposed in a publication from the Centers for Disease Control that some people with HIV should receive pentamidine for pneumonia even if they were well, setting the US Food and Drug Administration off on a scramble to approve the drug despite a lack of empiric evidence – in part to please people living with HIV and AIDS who wanted it.8
While this new status as a preventive agent was short-lived, pentamidine use continues today. In fact, it has returned to Africa, where nearly 20 million people now live with HIV/AIDS. Sanofi, the company that bought and subsumed Rhone-Poulenc, the corporation that once made Lomidine, has partnered with the World Health Organization to provide medications for HIV/AIDS, including drugs used to treat opportunistic infections.1(p188) On the list is pentamidine.
Sanofi is also providing the drug for another purpose. Although the mass immunization campaigns are now understood as dangerous folly, the steady treatment of cases has real value for reducing endemic levels of trypanosomiasis in sub-Saharan Africa. Tragically, when immunization stopped, treatment did, too; by the 1970s, the disease Europeans had once harmed people in order to stop had instead resurged. Since then, though, deaths have fallen from 34,000 in 1990 to just 3,500 in 2015,9 and geographic areas of transmission have narrowed. The African Union is now working on eradication. The aim is to wipe sleeping sickness from the map by 2020.9
References
- Lechanel G; Tousignant N, trans. The Lomidine Files: The Untold Story of a Medical Disaster in Colonial Africa. Baltimore, MD: Johns Hopkins University Press. p. 96.
- Gilbrin, “Rapport du chef de region de la Boumba-Ngoko a M. le haut-commissaire de la Republique francaise au Cameroun. Accidents mortels suite passage GMT 15,” November 19, 1954.
- Neujean, Georges. “Chimiotherapie et chimioprophylaxie de la maladie du sommeil a T. gambiense. Rapport presente au 6eCongres international de medicine tropicale,” Lisbon, September 5-13, 1958, p. 9-10.
- Babokhov P, Sanyaolu AO, Oyibo WA, Fagbenro-Beyioku AF, Iriemenam NC. A current analysis of chemotherapy strategies for the treatment of human African trypanosomiasis. Pathog Glob Health. 2013; 107(5): 242–252.
- Centers for Disease Control and Prevention. “Parasites—African trypanosomiasis (also known as Sleeping Sickness): transmission and control.” https://www.cdc.gov/parasites/sleepingsickness/prevent.html. Accessed January 14, 2018.
- Drake S, Lampasona V, Nicks HL, Schwarzmann SW. Pentamidine isethionate in the treatment of Pneumocystis carinii pneumonia. Clin Pharm. 1985;4(5):507-16.
- Steinbrook R. “Firm’s sharp price increase for AIDS drug attacked.” Los Angeles Times; 1987, October 31. http://articles.latimes.com/1987-10-31/news/mn-4490_1_aids-patients. Accessed January 14, 2018.
- Specter M. “Pressure from AIDS activists has transformed Drug testing.” The Washington Post; 1989, July 2. https://www.washingtonpost.com/archive/politics/1989/07/02/pressure-from-aids-activists-has-transformed-drug-testing/6856df63-9879-45f9-95b5-beb689bd6246/. Accessed January 14, 2018.
- World Health Organization, Fact sheet: trypanosomiasis, human African (sleeping sickness). http://www.who.int/mediacentre/factsheets/fs259/en/. Accessed January 14, 2018.
M. SOPHIA NEWMAN, MPH, is a writer, editor, and public health professional. She has worked as a global health journalist, reporting extensively from Asia, Africa, and the United States; a public health researcher via a Fulbright research grant to Bangladesh (2012–2013); and a technical writer at the Illinois Department of Healthcare and Family Services (Medicaid) (2011-2012). She currently works as a medical editor for the JAMA Network, editing manuscripts for the Journal of the American Medical Association family of journals. She also enjoys autodidactic language-learning and writing creative nonfiction. See more at msophianewman.com.

Leave a Reply