Vigneshwar Subramanian
Nivetha Subramanian
Cleveland, Ohio, United States
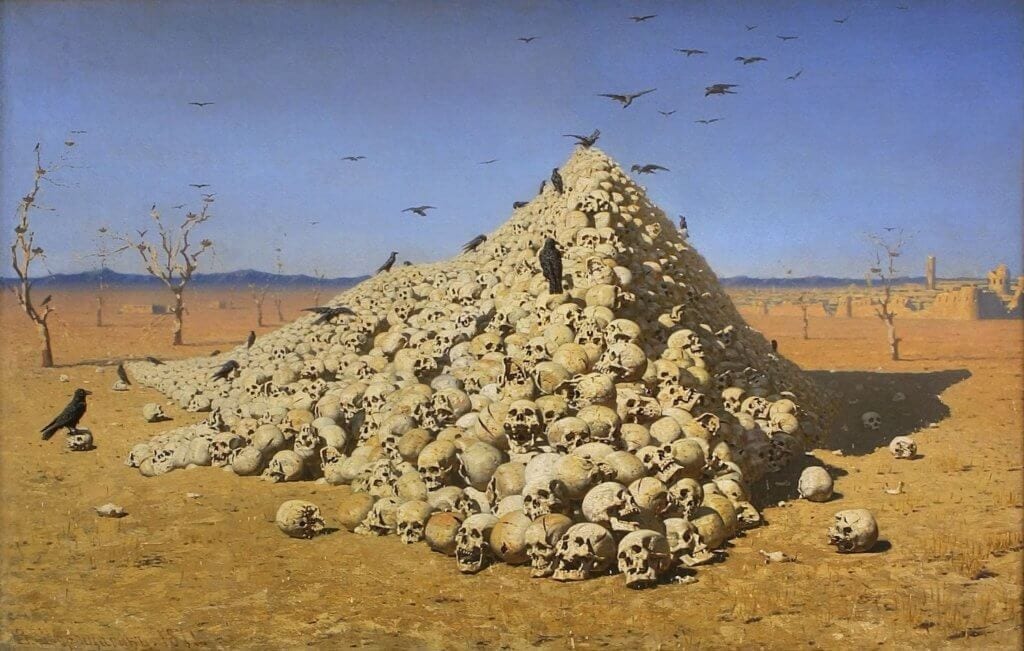 |
| The Apotheosis of War, Vasily Vereshchagin (1871) |
In April 1994, one of the largest genocides since the Holocaust erupted in Rwanda as the Hutu ethnic majority conducted a targeted slaughter of the Tutsi people.1 In a span of just over 100 days, over 800,000 people were killed.2 Infectious diseases such as HIV ran rampant, a consequence of sexual violence carried out predominantly against women.3 The already decimated population was further reduced after an estimated additional 30,000 to 80,000 individuals were incarcerated for directly participating in the killings.4 At the end of the genocide, an estimated 70% of the remaining population were women.5
The terms Tutsi and Hutu originated from the migration of two separate waves of people to pre-colonial Rwanda. For centuries the communities lived on the same land, sharing language and religion.6 In 1918 the Treaty of Versailles established Rwanda as a colony of Belgium.7 Belgian physicians propagated the belief that the Tutsi ethnicity was superior to the Hutu, which colonizers furthered by providing economic and political privileges to the Tutsis.8 Later this myth was used by Hutu political leaders to justify the decimation of the Tutsi “cockroaches.”9
Towards the end of the 1990s, French author and journalist Jean Hatzfeld conducted interviews with fourteen survivors. Like many people who lived through the genocide, they generally suffered from post-traumatic stress disorder, anxiety, and depression, in addition to socioeconomic displacement.10 In his 2006 book Life Laid Bare, he reports their first-hand accounts of the conflict and its aftermath.11 Their somber and evocative memoirs bear witness to both horrific atrocities and the incredible resilience of the human spirit. Among the narratives is the story of Sylvie Umubyeyi, who became a social worker to help displaced individuals following the genocide. In the course of her work, Sylvie connects with people whose world has been shattered and helps them begin to heal. Her account is one of profound loss and courage, but also a testament to the healing power of empathy.
Sylvie’s extended family once numbered two hundred people living together in a single neighborhood, but after the genocide only twenty survived. Pregnant at the time, she fled with her husband and children to the town of Nyamata to start anew. Even after the killing had ceased, Sylvie could not imagine returning to her hometown “because the things and people I once longed for there are gone.” In Nyamata, a town of refugees and strangers, “no one is where he or she belonged anymore.” Later she landed a job with a Canadian organization as a social worker. Working in the hills, she tracked down survivors, predominantly orphaned children, and attempted to bring them back to society.
A major theme of Sylvie’s recollection is the enormous trauma caused by the genocide. She states that it is unlike any other torment, a film projected every day before the eyes of the survivors. The experience has inflicted “buried in the survivor’s mind, a wound that can never show itself in broad daylight, before the eyes of others . . . if [those who haven’t experienced the genocide] make a real effort, they will one day accept the fact of this secret wound inside us.” This underscores both the difficulty and the importance of attempting to understand the perspective of genocide survivors, and by extension other patients who have experienced much mental or emotional trauma.
By recounting her social work, Sylvie allows us to witness a fraction of the grief and pain experienced by survivors over their loss. She describes children and the elderly alike as broken people who have lost all hope. Youth who once spoke of the slaughter as terrible and extraordinary eventually stop talking “because they understand no one will ever replace those they’ve lost, and they shut themselves up inside a silent bad dream.” Elders “are inconsolable over their losses. They had raised children who gave them food, clothing, sweet comfort in their old age, and now they are left without a soul around them.”
Sylvie’s genuine, empathetic efforts to connect with each of her unique patients are of particular note. She varies her approach based on each individual’s age and the nature of their trauma. The youngest children are the quickest to improve, as “when they begin to taste life again, they recover themselves more spontaneously. Their pleasure is still lively.” Adolescents struggle with their inability to explain “why [the genocide] happened,” but benefit from conversing with each other: “when they speak about this among themselves, they do listen to one another, sharing their feelings, and that helps ease their anxieties.” The elderly “now see only loneliness and poverty ahead for company. It’s really so hard for them not to drown their thoughts in the abyss of memory.” Although most of the violence was perpetrated against the Tutsis, Hutu children were also victims, forced to flee into the bush during the conflict. These children were left without “a soul [to] take care of them anymore, they felt rejected by everyone, and returned like the lowest of the low.” Furthermore, they are terrified that they will be mistreated and “as the years go by, they feel more and more guilty for their parents’ evil deeds.” Sylvie acknowledges that “it is such hard work, encouraging them to speak […] but [one] must be very patient and gentle with them, and visit them regularly, entrusting time with the birth of friendship.”
Medical encounters are fundamentally social interactions. Since time immemorial, patients have brought their fear, anxiety, and pain to examinations. The caregiver must calm their fears and instill hope. In recent years, however, the overwhelming focus on good medical science has eroded the importance of establishing a strong patient-provider relationship. Often, physicians may perceive patients as collections of parts and lists of diseases, without acknowledging their humanity or relating to their experiences. Sylvie’s account is a reminder of the crucial importance of empathy in the care of patients, especially those burdened with trauma.
References
- Fergal Keane, Season of Blood: A Rwandan Journey (London: Penguin, 1996).
- Binaifer Nowrojee, “Shattered Lives: Sexual Violence during the Rwandan Genocide and Its Aftermath” (Human Rights Watch, 1996).
- Ibid.
- Philip Gourevitch, We Wish to Inform You That Tomorrow We Will Be Killed with Our Families: Stories from Rwanda (New York: Picador/Farrar, Straus, and Giroux : Distributed by Holtzbrinck Publishers, 2004); Binaifer Nowrojee, “Shattered Lives: Sexual Violence during the Rwandan Genocide and Its Aftermath.”
- World Health Organization, “Success Factors for Women’s and Children’s Health: Rwanda,” 2015.
- Gourevitch, We Wish to Inform You That Tomorrow We Will Be Killed with Our Families.
- Keane, Season of Blood.
- Mahmood Mamdani, When Victims Become Killers: Colonialism, Nativism, and the Genocide in Rwanda, 3. print., and 1. paperback print (Princeton: Princeton Univ. Press, 2002).
- Ibid.
- Heide Rieder and Thomas Elbert, “Rwanda – Lasting Imprints of a Genocide: Trauma, Mental Health and Psychosocial Conditions in Survivors, Former Prisoners and Their Children,” Conflict and Health 7 (March 26, 2013): 6, https://doi.org/10.1186/1752-1505-7-6.
- Jean Hatzfeld, Life Laid Bare: The Survivors in Rwanda Speak (New York: Other Press, 2006).
VIGNESHWAR SUBRAMANIAN is a first-year medical student at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. He studied chemistry and economics at Cornell University. His current interests in medical humanities lie at the intersection of conflict and health.
NIVETHA SUBRAMANIAN is a third-year medical student at Case Western Reserve University School of Medicine. She is a member of the Humanities Pathway at Case, where she participates in discussions about various topics in the medical humanities. Since her undergraduate years, she has been very interested in genocide and its effects on individuals and nations.
Winter 2018 | Sections | Doctors, Patients, & Diseases

Leave a Reply