Rebecca Shulman
Philadelphia, Pennsylvania, United States
“…the primitive organ of smell, the basest of the senses” – Patrick Suskind, Perfume
 |
| Paul Broca, who mapped the parts of the human brain involved in olfaction and argued that they had been supplanted by free will. |
For the past two centuries, the medical profession has had a deeply-held but wholly unconscious ambivalence about the sense of smell, including the myriad ways in which it can become disordered. The same ambivalence does not infect the medical view of the other senses. Generations of medical students have absorbed the sequence “Inspection, palpation, auscultation” with the understanding that their senses are indispensable tools of physical diagnosis. The omission of olfaction, a sense which so often comes intrusively and involuntarily into play at the bedside, passes without comment. It is therefore unsurprising that olfactory testing is not routinely performed by primary care physicians.1 Disturbances of the sense of smell must be identified by the patients themselves, even though three-quarters of those with an olfactory dysfunction do not recognize it.2 Elder statesman of the medical profession have codified the neglect. McGann3 notes the paradox that an authoritative 1958 textbook devoted to the nose and sinuses begins summarily: “in Man the sense of smell is relatively feeble and not of great significance.”3, 4 Occasionally the case for the sense of smell is taken up by an author who reminds us that uremia, ketosis, and alcohol are all associated with distinctive exhalations providing invaluable diagnostic clues, but this is usually in the context of a lament that the sense of smell in the medical literature is not “given much attention.”5
This derogation of the sense of smell seems odder still after considering the demographic data. A recent survey reported that anosmia—the total loss of the sense of smell—affects about 3.4 million adults over the age of forty in the United States. That number does not include the millions suffering related pathological conditions—disorders giving rise to phantom or bizarrely abnormal smells, for example.6,7 The American Medical Association has determined that in a pragmatic accounting, anosmia is equivalent to the loss of only 3% of normal function.8 Total deafness, by comparison, represents a loss of 35%. These figures contrast starkly with the lessons of the legal database, where the consequences of injury to the olfactory sense are translated into strictly monetary terms. As of 2001, there have been at least twenty cases in which the court was asked to award damages to patients who lost their sense of smell due to medical misadventure. Forty percent of the suits produced out-of-court settlements or jury verdicts in favor of the plaintiff, with a median payment of $575,000.9 Small wonder that otorhinolaryngologists have admonished the medical profession for treating olfactory impairment as a “mere inconvenience” rather than a serious illness.8 The professional litigants, fine-tuned to the non-specialist’s pecuniary point-of-view, have not been similarly misled.
The demotion of the sense of smell in the hierarchy of the five senses does not believe that its potency and adaptive function are well-established. Humans possess more scent-producing glands than any other primate,10 and it is claimed that we can identify a trillion distinct odors or more.11 Human subjects on all fours are capable of tracking scents across natural terrain, instantaneously comparing the inputs of both nostrils in the same manner as bloodhounds.12 The adaptive functions of the sense of smell are at least three-fold. Most conspicuously, olfaction plays a role in guiding dietary choices throughout life. Breast-feeding infants are led to the breast by maternal odors, and elderly women with disordered olfaction are predisposed to weight loss and malnutrition.13, 14 Secondly, olfaction serves as an alarm system against environmental hazards, including physical threats (fire, leaking gas) and ingestible toxins (spoiled meat, sewage, excrement). Patients with congenital anosmia demonstrate an abnormally acute ability to recognize expressions of fear and disgust in others, suggesting that heightened attention to menacing visual cues is a necessary compensation for the loss of olfaction.15
Thirdly, the ability of humans to detect signals emitted by our odor-producing glands has made possible a form of rudimentary social networking that anticipated Match.com by 200,000 years. Odor aversion may have a special role in the selection of mates, where it acts to prevent inbreeding. This conclusion is supported by a study which showed that women perceived the odor of men’s soiled T-shirts to be more “pleasant” (perhaps a euphemism, in consideration of the male volunteers) if the wearers were of a different genetic (HLA) subtype.16 Evolution has in effect imposed a kind of incest taboo that transforms consanguineous sweat into an amatory turn-off.17
Other survival benefits of the sense of smell, beyond its proven role in regulating diet, unmasking environmental hazards, and guiding social interactions, are only now being discovered. For example, odors may stimulate and suppress immune responses both directly and by shaping conditioned responses.18
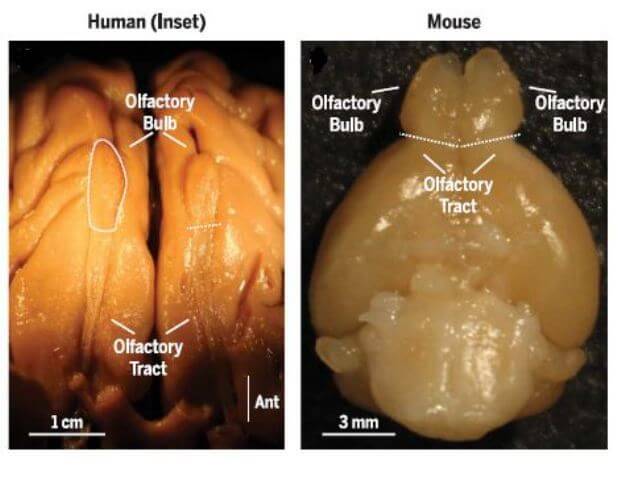 |
| The relatively small olfactory bulb of humans was interpreted by Paul Broca as evidence of its minor importance. Retrevied from Poor human olfaction is a 19th-century myth by McGann JP. |
Why then, given this catalog illustrating the biological importance of the sense of smell, does the medical profession tend to depreciate it? An examination of intellectual history suggests that there are subliminal influences at work, forces more obscure and less rational than a profession founded on analytic skill might care to acknowledge. McGann3 traces the prevailing myth that the human sense of smell is weak and inconsequential to Paul Broca, the nineteenth century neuroanatomist. Broca meticulously unraveled the physical basis of the sense of smell, discovering its origins in the olfactory epithelium lining the nasal passages where millions of neurons bearing the odor receptors are located. Sensory neurons in the nasal epithelium project their axons into the olfactory bulb on the underside of the human forebrain. From there, information is transferred to the primary olfactory regions in the prefrontal cortex. The prefrontal regions are connected in turn to the hippocampus, the thalamus, and the hypothalamus, structures belonging to the limbic system. The functional unity of the limbic system has since been questioned, but for Broca the limbic system represented the residuum of the primitive mammalian brain—a kind of foundry in which was forged a complex alloy of memory, emotion, pleasure, and smell. Critically, human brains, in contrast with animal brains, possess a small olfactory bulb and a large forebrain, an anatomical fact that in the fashion of nineteenth century science, Broca chose to read as allegory. With its evolutionary ascendance (Broca surmised), the human species conquered the animal-like inducements associated with scent and pleasure (symbolized by the shrinking olfactory bulb) and replaced them with free will (symbolized by the massive forebrain). Neuroanatomy could be made to prove that the sense of smell is a dwindling legacy of our amoral ancestors.
As Broca discovered an anatomical basis for depreciation of the sense of smell, so Freud found a basis in psychosexual development. Excessive dependence on olfaction in orthodox psychoanalytic theory is a trait that belongs to animals, children, and neurotics. Atrophy of the sense of smell, in contrast, is one hallmark of mature sexuality:
The diminution of the olfactory seems itself to be a consequence of man’s raising himself from the ground, of his assumption of an upright gait; this made his genitals, which were previously concealed, visible . . . and so provoked shame.19
 |
| William Wordsworth, who celebrated the scent of blossoms in his Lyrical Ballads despite being completely anosmic from birth. |
What Broca and Freud have in common is the impulse to dismantle the more unpalatable implications of evolution by turning them into a story of moral progress—i.e. an ascent that is either metaphysical or psychosexual, but in either case a repudiation of our animal roots. In addition to these philosophical influences on the medical profession, there are social forces that promote a dismissive attitude toward the sense of smell. For example, research suggests that a dependence on olfactory cues is allied to social conformity, a trait that is discouraged during medical training to the extent that it interferes with candid speech and independent thought.20 It is also instructive to recall that the greatest anxiety facing anosmics is not spoiled food or undetected house fires. Far more terrifying is the prospect of becoming the unwitting source of crowd-dispersing smells.5 Physicians, like other non-anosmics, have learned the taboos that attach to normal human effluvia and know that even to notice the odor of strangers is a breach of decorum. To turn one’s nose into a scanning device, and then use it to probe a stranger’s odors, is an escalation into pure gaucherie.
And then, finally, there is a link between the sense of smell and medical practice that is indelible because it carries the odor of the grave. It has been observed that sick people give off a disagreeable odor, and it is axiomatic among clinical practitioners that there is such a thing as “the stench of death.”9, 21 But if there is a universal animal recoil from diseased flesh, the recoil is many times worse in the physician, for whom the smell of human mortality signifies the limitation of healing powers. Perhaps the turning against the sense of smell in medicine is not, after all, just a repudiation of animal instinct and unfiltered emotion or, worse, a politesse born of middle class sensibility. Thousands of years of evolution have turned the odor of decay into a memento mori, an odor as unwelcome to the physician as if it were personified with a black cowl and a scythe. There is a paradox, but no mystery, if the sense of smell has acquired dire associations because it alerts us to the process by which the senses are extinguished. Smells are intricately interwoven with memory, and a single experience of “the stench of death” is never erased. Knowing this, how easy it is to imagine the sense of smell falling in the esteem of physicians, suffering an inevitable if only semi-conscious neglect, precisely because its aftershocks elicit a mild form of the abhorrence felt for the specter of death itself.
Reference List
- Boesveldt S, Postma EM, Boak D, et al. Anosmia–A critical review. Chem Senses. 2017;42:513-523.
- Adams DR, Wroblewski KE, Kern DW, et al. Factors associated with inaccurate self-reporting of olfactory dysfunction in older US adults. Chem Senses. 2016;42(3):223-231.
- McGann, JP. Poor human olfaction is a 19th-century myth. Science. 2017; 356, 1-6.
- Negus VE. The Comparative Anatomy and Physiology of the Nose and Paranasal Sinuses. Livingstone, Edinburgh,1958.
- Kelly M. Scent of a patient:an underestimated role in clinical practice? Br J Gen Pract. 2012;62(600):378.
- Keller A and Malaspina D. Hidden consequences of olfactory dysfunction: a patient series. BMC Ear, Nose and Throat Disorders. 2013;13(11):8.
- Landis BN, Konnerth CG, Hummel T. A study in the frequency of olfactory dysfunction. Laryngoscope. 2004;114(10):1764-1769.
- American Medical Association [AMA]. 1993. Guides to the evaluation of permanent impairment. 4th ed. Chicago (IL): AMA.
- Miwa T, Furukawa M, Tsukatani T, et.al. Impact of olfactory impairment of quality of life and disability. Arch Otolaryngol Head Neck Surg. 2001;127:497-503.
- Stevenson RJ. An initial evaluation of the functions of human olfaction. Chem Senses. 2010;35:3-20.
- Bushdid C, Magnasco MO, Vosshall LB and Keller A. Humans can discriminate more than 1 million olfactory stimuli. Science. 21 Mar 2014; 343:1370–1372.
- Porter J, Craven B, Khan R, et al. Mechanisms of scent tracking in humans. Nat Neurosci. 2007;10:27-29.
- Varendi H, Porter R. 2001. Breast odor as the only maternal stimulus elicits crawling towards the odour source. Acta Paediatr. 90:372–375.
- Duffy VB, Backstrant, JR and Ferris AM. Olfactory dysfunction and related nutritional risk in free-living, elderly women. J Am Diet Assoc. 1995;95:, 879–884.
- Lemogne C, Smadja J, Zerdazi E-H, et al. Congenital anosmia and emotion recognition: A case-control study. Neuropsychologia. 2015;72:52–58.
- Wedekind C, Seebeck T, Bettens F and Paepke AJ. MHC-dependent mate preferences in humans. 22 Jun 1995;1359:245-249.
- Chen D and Haviland-Jones. Human olfactory communication of emotion. Percep Motor Skills. 2000;91:771-781.
- Ramirez-Amaya V, Bermudez-Rattoni F. 1999. Conditioned enhancement of antibody production is disrupted by insular cortex and amygdala, but not hippocampal lesions. Brain Behav Immun.199;13:46–60.
- Freud S. Civilization and Its Discontents. 1962. New York, NY: WW Norton & Company; 1962, 46.
- Seo H-S, Lee S and Cho S. relationships between personality traits and attitudes toward the sense of smell. Frontiers of Psychology. 2013;4:1-8.
- Bomback A. The physical exam and the sense of smell. New England Journal of Medicine. 2006;354(4):327-329.
REBECCA M. SHULMAN, BA, is an MD candidate in the Class of 2018 Lewis Katz School of Medicine at Temple University in Philadelphia, PA. She was born and raised in Bucks County, Pennsylvania. Much of her extended family lives in rural Puerto Rico, a region she regards as a second home. She has a degree in psychology from New York University and plans to be a radiation oncologist.
Highlighted in Frontispiece Volume 10, Issue 2 – Spring 2018
Winter 2018 | Sections | Doctors, Patients, & Diseases

Leave a Reply