Ohakpougwu Emmanuel
Accra, Ghana
The year is 1279 BC, the beginning of the reign of Ramesses II. There are cries and incantations as the priests mumble words and family stand by my bedside alongside pots of medicines for my ailment. I lie on my death bed and drift through the memories of our achievements. If I die, I will die a proud Egyptian doctor because our medicine has now become a foreign export. This began when Ramses II, in response to a request, dispatched a doctor, Pariamakhu, to the Hittite court to prepare herbs for Karunta, King of the land of Tarhuntas.1
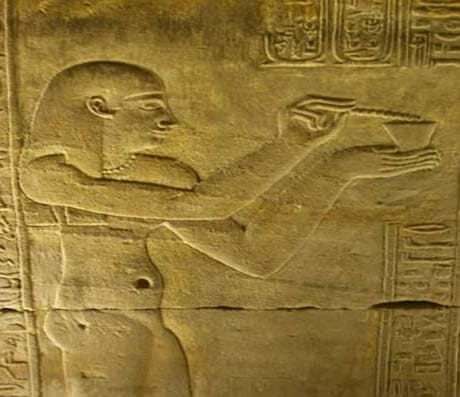
The temple
I am an ordinary physician. The House of Life (Per Ankh) was the medical study center where doctors like myself were taught at major temples. There were magnificent temples at Dendera, Deir el-Bahri, and Philae.1 They had herb gardens in which many of the ingredients for the physicians’ remedies and prescriptions were grown. Large collections of writings on papyri were kept at the temples. Sick people seeking help at the temples made offerings to the gods before being treated.
On hearing patients’ complaints we would carry out medical maneuvers, looking, feeling, and listening in order to obtain information about the patient’s body. We used the concept of syndromes, a group of signs and symptoms that delineate a recognizable pattern. We also identified signs such as trismus, neck stiffness, and weak pulse as markers of severe physical compromise. When a patient visited the temple with an infected wound, I would use a mixture of ibex fat, fir oil, and crushed peas in an ointment to clean the infected wound.1 Our teaching and practice distinguished between sterile wounds and infected wounds. If a worker presented with excessive bleeding, I would immediately proceed with cauterization to stop it. When a worker at the pyramid at Giza presented with a fractured humerus, I set the fracture with bark splints, bandages, and plaster made of acacia mixed with gum and water. But when a woman brought her son with lockjaw, it was sad because we were specifically instructed by the papyrus not to treat this ailment.
Patients often came with periodontal disease.1 This was provoked by the stresses and strains applied to the teeth because of contamination of their cereals and bread with fragments of sand and grit. For periodontal disease I gave a mixture of cumin, frankincense, and carob-pod pulp ground to a powder and applied to the tooth.
Almost every day we attended to women in labor. They adopted a squatting position on a birthing stool. Some of our maneuvers during birth were deleterious. Some women did not survive, like Princess Hehenhit (Eleventh Dynasty) who died soon after giving birth. She had a vesicovaginal fistula which must have caused a severe postpartum infection.2 Unfortunately the Kahun Papyrus had no cure or treatment for such an ailment: “Prescription for a woman whose urine is in an irksome place; if the urine keeps coming . . . , and she distinguishes it, she will be like this forever.” If a woman wanted a pregnancy test, I would tell her to moisten barley and emmer with her urine every day “. . . if both grow, she will give birth. If the barley grows, it means a male child. If the emmer grows, it means a female child. If neither grows, she will not give birth.”2
Pharmacopeia and discoveries
Medications were weighed and measured carefully. Fractions were expressed by dissecting the eye of the god Horus, the son of Isis and Osiris,2 which had been torn out and ripped to pieces by his evil brother, Seth. The character Rx designating the word “prescription” is a direct descendant of the symbol for the “Eye of Horus”.2
In my prescriptions I used much honey; it is highly resistant to bacterial growth. Many drugs were given in beer, which the people of Egypt drank in large quantities. They knew and used the benefits of yeast, applying it raw to boils and ulcers and swallowing it to soothe digestive disorders.
Our remedy for a crying baby was “spn,” which translates as “poppy,” the plant whose alkaloids produce opium and morphine. The prescription was “spn” seeds and fly dung from the wall, made into a paste, which was strained and drunk for four days. The crying always ceased instantly. The belief was that it cured ailments not visible to man. I recall advising patients to apply chrysocolla, copper silicate, to their skin. Copper often prevents the penetration of bacteria, particularly staphylococci. The day before I took ill, I had fitted a wooden prosthesis on a fifty-year-old woman after her big toe had been amputated because of gangrene.
We were the first to use the word “brain” in any written language . . . “the membrane enveloping his brain, so that it breaks open his fluid in the interior of his head.”3 We noted the connection between the heart and pulse rate. We felt the infant’s fontanelle “fluttering under the fingers like the weak place of an infant’s crown before it becomes whole.”3
Time travel
As the sun sank I felt light. I was having an out of body experience and saw future achievements in African medicine. I saw a Hausa test for impotence described thus: “An individual is stripped and placed on a mat lying on his back. A pin or thorn is lightly rubbed over the inside of his thigh. If the scrotum or testicles do not move, the individual is considered impotent.”3 Did they understand the cremasteric reflex?
In Liberia, the Mano developed an admirable quarantine system for smallpox, setting aside a “sick bush” for affected patients, which they burned when the illness ran its course. During an epidemic, material from the pustule of a sick person would be scratched into the skin of unaffected persons with a thorn. There would be no reaction and the persons inoculated now were protected against smallpox. Sometimes the inoculation produced a mild form of the disease, which also conferred permanent immunity.
I saw Mano midwives pulling repeatedly at the breasts of women in labor, a maneuver which released oxytocin—a stimulator of uterine contractions—from the pituitary gland. They sometimes walked around with laboring mothers, causing the cervix to dilate and the head to engage, thus facilitating labor.3
Some Bantu midwives would use Indian hemp during labor for its sedative properties. Newborn babes and infants were taken and exposed to the sun for a period each day “to make them strong.” Were they treating neonatal jaundice?
In my next vision, a Caesarean section was performed in 1879 by a Banyoro surgeon in Uganda, witnessed by a missionary doctor named Felkin.4 Not only did the surgeon understand the sophisticated concepts of anesthesia and antisepsis, but also demonstrated advanced surgical technique. In his sparing use of the cautery iron, he showed that he knew tissue damage could result from its overuse.
My sojourn through time revealed the abundant materia medica of traditional African cultures. The Zulus know the medicinal uses of some 700 plants.4 “Fever-leaf” is used all over Africa to treat recurring malarial fevers. Certain Bantu-speaking peoples used the bark of Salix capensis (willow), the active ingredient of aspirin, to treat rheumatism. In Mali kaolin is used to treat diarrhea. Caffeine-containing kola nuts are chewed all over Africa for their stimulating and fatigue-combating properties. Plants containing ouabain and strichnine are used for snakebite; the former a heart stimulant and therefore useful against cardiotoxic venoms, and the latter a nerve tonic, useful against neurotoxic venoms.
Can’t beat that headache? Aspirin has failed? Why not try an incantation to falcon-headed Horus, or a soothing poultice of “Ass’s grease”? It works with a little faith.
I am beginning to feel light hearted, maybe a little bit better. The sun’s rays filter through the window at daybreak and I am back on my feet. I guess the god Sekhmet spared me this time. It is 1279 BC, the beginning of the reign of Ramesses II. I am still a proud Egyptian doctor,—proud of our immense strides and contributions to medicine. Will this papyrus ever be found?
References
- Carlo Reeves. Egyptian Medicine .United Kingdom: Shire Publications; 1992.
- Ancient Egyptian Medicine. http://www.crystalinks.com/egyptmedicine.html. Accessed January 24, 2017.
- http://www.reshafim.org.il/ad/egypt/timelines/topics/medicine.html. Accessed January 24, 2017.
- http://raceandhistory.com/selfnews/viewnews.cgi?newsid995545990,4925,.shtml, published Thursday, July 19, 2001. Accessed January 25, 2017.
OHAKPOUGWU CHUKWUEBUKA EMMANUEL is a second year medical student at Family Health Medical School. He sees writing as a means of social change and paradigm shifts in the medical community. He writes to enlighten, amuse, and to learn.
Highlighted Vignette Volume 14, Issue 2 – Spring 2022

Leave a Reply