Paul Kettl
Philadelphia, Pennsylvania, USA
 |
|
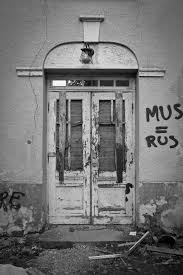
An abandoned mental hospital. |
I’m not sure I’m so ethical.
Don’t get me wrong. I think I’m a good doctor, and I don’t do bad things like sleep with my patients, beat my wife, or kick the dog. But I’m just not sure anymore I’m as ethical in my practice as I should be.
It used to be easy. I used to think bad people did bad things, and I simply shouldn’t be bad, or do those bad things. The Nazis pursued awful medical experiments on Jews, prisoners, and other ethnic groups they considered beneath them. But they were Nazis and we saved the world from them. The problem is, at the same time, the United States Public Health Service also was experimenting on African American men in Tuskegee, Alabama because they were curious about the course of syphilis. Those experiments continued until 1972, without the knowledge or consent of those involved, on an illness about which they were curious, perhaps on those they felt were beneath them.
It seems that not only bad people do unethical things. My father, who was a decorated Normandy World War II Veteran who served in Germany at the end of the war said he did not think the average German citizen knew about all of the Nazi atrocities. “People back then thought they were pretty smart, too,” he said. It was easier to ignore things that didn’t seem right.
As a geriatric psychiatrist, I am confronted constantly by the vexing behavioral problems of Alzheimer’s disease that gradually steal humanity from its victims while family members desperately try to provide care. For years, I readily prescribed the older antipsychotic medications and then the newer atypical antipsychotics to try to help the misbehaviors and delusions that occur so commonly as the brain fails. I also joined research teams investigating the use of these medications in those with Alzheimer’s disease in nursing homes. We were careful to obtain proper consent from relatives, and to carefully monitor our patients in the studies. But it turns out that these medications led to a slightly higher death rate in the frail elderly who took them. At the time, I thought it was a good thing to use these medications to decrease delusions and treat agitation in those whose lives were being drained one step at a time. Now I’m not so sure.
Dr. William Osler, who invented modern internal medicine is quoted as saying, “When a new medicine comes out, use it while it still works.” As the knowledge of these illnesses and the medicines used to treat them advanced, we as a profession learned more about the effects and side effects of these medicines. Some of the studies in which I took part contributed to this growth of knowledge, and also to the knowledge that these same medications carried with them an increased risk of death.
Throughout the course of these studies, I was bothered by a nagging concern. It wasn’t simply the lack of knowledge that bothered me, but rather the profession’s rapid acceptance of the new drugs. Even then, I felt that these medications were being marketed too aggressively and were perhaps being oversold. I wasn’t sure, but I had a gnawing feeling in my gut. I went to work, did my best, and dismissed the feeling as uncertainty. More research was needed. Back then, I thought I was pretty smart too, as my Dad pointed out.
Now I’m not so sure. I’m not so sure I’m so smart or always so ethical. It is not that I deliberately do things that are bad or deliberately do things that are unethical. It is just that I do things without thinking enough about them. It is too easy to slide into complacency.
I have that same uneasy feeling sometimes now. In psychiatry, for many years Medicare paid less for psychiatric services than for other medical specialties. Was that right? Was that ethical? Insurance companies now often “carve out” psychiatric care to a separate, often “for profit,” business that “manages” (i.e. limits) psychiatric coverage. These companies, to no one’s surprise, are interested in making profits from people’s suffering. Is that right? Is that ethical?
Today, psychiatric inpatient hospital units are often closed, not because they are not “evidence-based,” but because they don’t make as much money for hospitals as orthopedics or cardiology. You see, non-profit institutions need money, too.
Is any of this ethical? Have I done enough, indeed anything, to investigate this? Am I ethical enough? I am beginning to think that I should not simply assume that I am an ethical provider just because I am not a bad guy. Examining ethics takes thought and reflection. I do not blame myself for not knowing enough about medications or diseases, or not knowing what will be discovered in the future. I blame myself for not taking enough time to evaluate that uneasy feeling I get. I’m just not sure I’m right.
I have also come to the conclusion that my doubt probably is not a bad thing. Assuming or “knowing” you’re right usually closes the door to further examination and leaves no room for questions or exploration. Simply believing you are “pretty smart” can stymie closer investigation. Under these circumstances, that uneasy feeling can stay buried.
Of course, these problems are not unique to psychiatry. Should we perform so many Caesarian sections, coronary artery bypass graft (CABG) surgeries, or surgeries for low back pain? Do we overuse antibiotics because the patient, or the little patient’s mother, asks for them? Do we gloss over a physical exam because we can always CT scan the area? There are a lot of situations that cause many of us to have that gnawing uneasy feeling we try to ignore. But as I get older, I find it harder to ignore that gnawing feeling. I used to think I was smart. I used to think I was ethical.
I’m not so sure any more I’m all that ethical, that I always do what I should. That feeling doesn’t go away. And I hope that maybe after reading this piece, you’re less ethical than you thought you were.
The opinions expressed are those of the author, and not necessarily those of the Department of Veterans Affairs or the federal government.
PAUL KETTL, MD, MHA, is clinical professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania and serves as education director for behavioral health for the Philadelphia VA Medical Center. A geriatric psychiatrist, he is interested in ethical issues in his practice, and continues to learn from the medical students and residents he teaches. He is the author of numerous essays and a novel, The President’s Secret, which explores the interface between psychiatry and politics.
Highlighted in Frontispiece Winter 2014 – Volume 6, Issue 1

Leave a Reply