Katrin Platzer
United Kingdom
Introduction
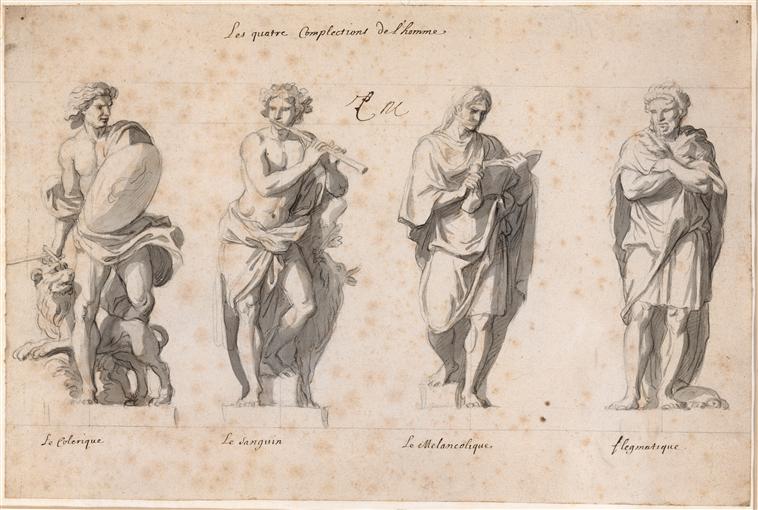 |
| Fig. 1 – The four humors, 17th century Centerpiece of Galen’s medical theory Charles Le Brun |
Over the past 200 years, the practice of medicine has changed dramatically. It can be said that until the end of the 18th century most of medicine was based on scant scientific evidence and often did more harm than good. Over the past two centuries, however, the ancient theories of disease have been replaced by modern scientific medicine. This change, though beneficial for the physical welfare of the patient, has somewhat removed him from his past position of power, to the extent that the persona and personal preferences seem to have disappeared from the picture.
Medical practice up to the end of the 18th century
Although hospitals existed from a very early point in history, their earlier functions were not necessarily medical. They were mostly religious institutions that included refuge of pilgrims or grouping together of sick slaves.1 They were not institution of clinical expertise and were avoided by anyone who could afford a private doctor.2 These private doctors also were not comparable to modern practioners. If trained at all, their knowledge consisted of ancient theories dating back to Hippocrates and Galen, and they were “not likely to be held legally accountable for their failures or mistakes.”3 Their most important skill was to come to good terms with their private patients, and act in accord with what the patient would expect. At that stage, the figure of the “sick man” was crucially important. Because of lack of true knowledge of causes of disease and the small amount of institutionalization, the power lay in the hands of the patients who could afford to pay a private doctor. The latter was in all ways dependent on the sick man and woman to approve of his practice.
Hospital medicine
Starting in France between the French revolutions of 1789 and 1848, medical education and medical practice underwent a major change. Acting in the spirit of the revolution, young French doctors abolished the ancient theories and established a new principle: “read little, see much, do much.” This was to happen in the newly founded hospitals, which were to be accessible to the ill of the wider public. Disease was now seen in terms of malfunctioning lesions, meaning pathological changes produced by disease. Doctors had a wider variety and larger number of patients, and could see links between symptoms and anatomy more clearly.5 In accord with this more localized concept of disease stands the introduction of diagnostic devices such as the stethoscope, which improved diagnosis and made examination more mechanical. During the early 19th century, statistical evidence was also first held to be relevant.6 Yet doctors could still not be of much help to their patients. They might have understood the causes of disease better, but still had no effective treatment. Because of the change in the power dynamic, making individual patients feel better was not always a doctor’s main concern. The sick man’s power had diminished, what mattered to doctors now was recognition amongst their fellow practitioners and respected superiors.7
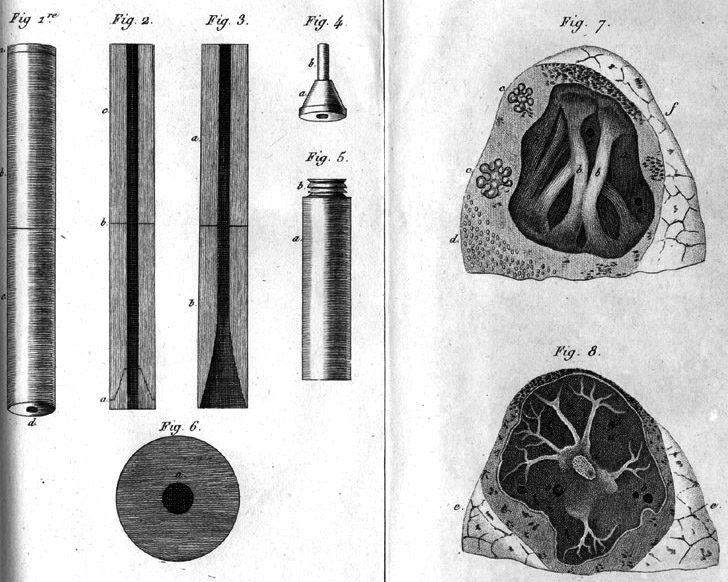 |
| Fig. 2 – De l’auscultation médiate Laennec’s first stethoscope René Théophile Hyacinthe Laennec |
Medicine in the laboratory
During the 19th and 20th century researchers began to understand the cellular processes underling various illnesses. This meant that medical understanding had to become all the more specialized, and the sick man in the classic sense disappeared from view. The patient’s diseases were still relevant, but only as a “material thing to be analyzed;”8 the persona behind the patient was now completely irrelevant. This was accompanied by a feeling of exclusivity within the medical world. Through the introduction of technical jargon and journals only accessible to a selected few, outsiders to the medical professionals, including most patients, were left defenseless in the medical professionals’ hands.9
The role of the doctor
Although medical practice changed dramatically, an ill person’s first point of contact remained a doctor. However, the concept of a good doctor underwent major transformation, as with the increase of specialized knowledge the general practitioners were largely replaced by specialists. The general practitioner, still the first line of contact for the patient, is excluded from the hospital setting and also from the specialist knowledge gained in those settings.10 His main function now is not necessarily to treat, but to refer to specialists. Consultations also changed location; home visits have become more and more infrequent, and patients are requested to go see the doctor. This removes the patients from their homes, and places them more anonymously into the doctors’ practice. Medical knowledge nowadays is specialized in so many aspects that one doctor simply cannot know it all. This is represented in the constant passing-up of patients. In 1970 a patient coming into hospital would be seen by an equivalent of two clinicians; now this number has gone up to more than fifteen,11 and an investigation into the background of any individual patient has become nearly impossible.
The doctor-patient relationship
In 1951 Talcott Parson described his account of an ideal doctor-patient relationship; the doctor was in the role of power, with a right to give medication and to make decisions. The patient was in the sick role, with the right to take medication and stop working, but was expected to want to get better.12 This can also be described as a paternalistic doctor-patient relationship, since the information is given solely from the doctor to the patient, and it was ultimately the doctor who decided on treatment. One could expect this kind of relationship to be practiced at the age of laboratory medicine; however it is largely discouraged nowadays. This is because we seem to have moved to another age in medicine, which some call “e-scaped medicine.”13 Through the internet and other information sources, medical knowledge (and knowledge that claims to be) is now more widely accessible, and patients, through the use of these resources are now taking more responsibility for their health.14 Indeed, medical professionals are often encouraged to involve the patient in discussions about their condition, making sure the patient understands the importance of their treatment and also giving patient’s choice in treatment options. This is to increase the patient’s compliance with the treatment plan, since an understanding of the disease and treatment often helps the patient understand why they have to take the medication they do. Thus, the “sick man and woman” has in many ways resurfaced, and doctors have acknowledged that. Promising as that might seem, with primary care physician consultations often targeted to as little as ten minutes, a truly mutualistic doctor-patient relationship seems unlikely to be established in the near future. Although the medical profession acknowledges the need for more personal doctor patient contact, the question whether they can offer it realistically at this time remains, and this is also represented in patients frequently seeking alternative therapies such as homeopathy, which although no more effective than a placebo, are practiced mostly by therapists who are generally able to spend more time with the patient.
Reference
- Bynum, William F. The history of medicine. Oxford: Oxford university press, 2008.
- Porter, Roy. The greatest benefit to mankind. London: HarperCollins, 1997.
- Porter, The greatest benefit to mankind. 675.
- Bynum, The history of medicine.
- Jewson, ND. “The disappearance of the sick-man from medical cosmology, 1770-1870.” International journal of epidemiology 38, no. 3 (2009): 622-633.
- Bynum, The history of medicine.
- Jewson, “The disappearance of the sick-man”, 627.
- Jewson, “The disappearance of the sick-man”, 629.
- Porter, The greatest benefit to mankind, 679.
- Porter, The greatest benefit to mankind, 684.
- Atul Gawande, TED. “How do we heal medicine.” Digital video, 2012. http://www.ted.com/talks/atul_gawande_how_do_we_heal_medicine.html (accessed 1 Mar 2014).
- Gallagher, Eugene B. “Lines of reconstruction and extension in the Parsonian sociology of illness.” Social Science \& Medicine (1967) 10, no. 5 (1976): 207-218.
- Nettleton, Sarah. “Commentary: The appearance of new medical cosmologies and the re-appearance of sick and healthy men and women: a comment on the merits of social theorizing.” International journal of epidemiology 38, no. 3 (2009): 633-636.
is a third year medical student at the University of Bristol. She has undergone a bachelor programme in Medical Humanities in 2012/13. Her main interests include the history of medicine and classical and modern literature in relation to medicine. Aside from her studies she works as a professional cemetery tour guide at her local cemetery, giving tours that focus on the medical history of Bristol.
Highlighted in Frontispiece Summer 2014 – Volume 6, Issue 3

Leave a Reply