 |
| Figure 1. Baron Dominique-Jean Larrey Stipple engraving by A. Tardie – Public Domain via Wikimedia Commons |
Stavros Gourgiotis
Athens, Greece
Hippocrates stated that “war is the only proper school for surgeons.” War inevitably gives an impetus to surgical innovations and many advances in surgery have been made in the historic training ground for surgeons: the armed conflict. During past centuries the management of the numerous and serious battlefield wounds was not effective because facilities were lacking on the field, hygiene was ignored, and surgeons had no interest or knowledge in preventing post-operative infections.
A new dimension to the military surgery and trauma care that embodied sanitation, epidemiology, evacuation of the injured, and training of medical personnel was given by Baron Dominique-Jean Larrey, Chief Surgeon of the French Army (Figure 1). Larrey was one of the principal surgeons of Napoleon’s massive army that engaged in battle across Europe and the Middle East for almost twenty years. He participated in twenty-five campaigns, sixty battles, and 400 engagements.1 His innovative practical research have had a positive impact on today’s military surgery and trauma care. From the American Civil War to the Iraq and Afghanistan wars, the organization system introduced by Larrey has saved thousands of lives.
His contribution in surgery and battlefield medicine consisted of the creation of flying ambulances, the first description of triage, the amputation at the shoulder joint known as Larrey’s amputation, the first successful pericardiocentesis for trauma, the ligation of the femoral artery immediately below Poupart’s ligament, a muscular defect in the diaphragm (Larrey’s cleft), and a sign of sacroileitis (Larrey’s sign).2
He was among the first to use positive pressure breathing to treat people with chest wounds and to drain pus from wounds. He used snow and ice to anesthetize injured limbs before amputation and to preserve injured limbs. He initiated, organized, and built military hospitals in Egypt, Sudan, Syria, and Palestine while publishing articles about typhus, bubonic plague, leprosy, and trachoma. Dr. Larrey was a humanitarian who urged doctors to treat the soldiers of enemy armies with dignity and compassion.
The introduction of the field ambulance
Until Larrey’s day, army hospitals were placed at least three miles behind the front line. Wounded soldiers were often abandoned or carried by comrades or slow moving vehicles called “fourgons” that could take up to three days to reach the field. Such delays meant that the injured often succumbed to their wounds. Larrey recognized that traumatic injuries were time dependent, and that it was essential to deliver the most appropriate definitive surgical care without delay.
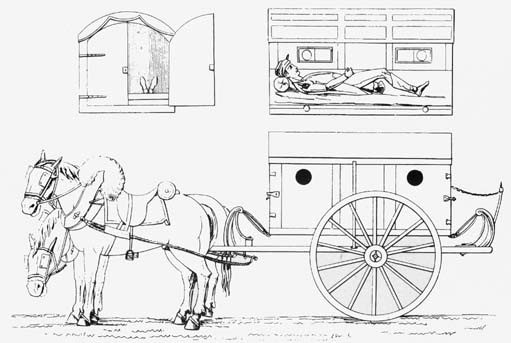 |
| Figure 2. Baron Larrey’s flying ambulance Public Domain via Wikimedia Commons |
In 1792 Larrey insisted on getting his special surgical teams near the front line to ensure early surgery and rapid evacuation of wounded men. He emulated the mobility of the “flying artillery” (ambulances volantes), which involved units of horse-drawn guns that kept pace with the advanced columns of troops (Figure 2). This required adapting a sprung lightweight chassis to create a horse-drawn vehicle that could both deliver surgical staff and remove the wounded in a degree of relative comfort.
Each unit consisted of three ambulance divisions, utilizing fifteen surgeons and 100 soldiers who were equipped with twelve flying ambulances and four fourgons which acted as mobile depots. They collected the dead as well as the wounded so that no one should be neglected. The flying ambulances could collect the wounded in less than fifteen minutes. Larrey and other surgeons could operate on the wounded either where they fell or have them carried to a sheltered spot nearby.3 In later iterations, Larrey grouped his ambulances into small units of about 300 personnel, thereby creating the forerunner of a modern military field ambulance, medical battalion, or close support medical regiments. Larrey in his memoir wrote: “The function of the organization is to rescue the wounded on the field of battle and, having given first aid, to transport them to the first line of hospitals”.4 Field ambulances have remained a basic division of all army medical services to this day.
The first description of triage
Larrey adopted a new way of treating the wounded. Previously surgeons treated the officers according to their class – upper class treated first, lower ranks next, and enemy prisoners last. Larrey believed “those who are dangerously wounded must be tended first entirely without regard to rank and distinction.” He knew that those with critical injuries would stand a good chance of surviving if operated on within the first hour of being injured. Those with minor injuries were made to wait, while the more seriously injured were put aside, often with alcohol to comfort them until they passed away. This process of systematic evaluation became known as “triage,” a French word meaning to separate or choose.5
The amputation
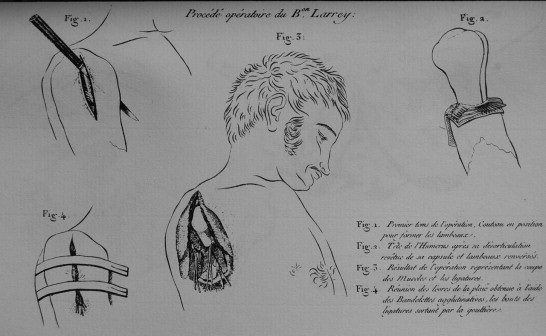 |
| Figure 3. Baron Larrey’s surgical procedure for shoulder disarticulation Public Domain via Wikimedia Commons |
Most wounds during the Napoleonic era were either from musket balls or canons. The latter was associated with a high rate of amputation. Most surgeons believed that postponing amputation, even for as long as twenty days, allowed the patient to recover from the shock of their wounds while becoming reconciled to the inevitable loss of their affected limb. After that period of time the standard approach was to cut the limb circumferentially and stretch the skin over the raw stump. This inevitably led to infected wounds, breakdown of the closure, and death from gangrene. However, Larrey discovered that mortality was much higher in delayed amputation, and at the very least a long and painful recovery for those who did survive the wait. He preferred to operate as early as possible, frequently in the field arguing that the wounds could be kept cleaner if closed early. Larrey adopted Henri Francois Le Dran’s technique of cutting the muscle and bone well above the wound and leaving a cuff of skin for a tension-free closure.3
Larrey also invented his own technique of rapid disarticulating the arm at the shoulder joint by splitting the deltoid and capsule, disarticulating the humerus outwards by carrying the arm transversally across the body, either forwards or backwards, sliding the knife down under the bone, dividing the tissues containing the axillary vessels, tying the arteries, and bringing the edges of the wound together with straps and sutures (Figure 3).4
The treatment of gunshot wounds of the abdomen
Larrey advocated leaving the wound wide open and removing the foreign object. When the omentum protruded from the abdominal wound Larrey insisted on its being left until the portion outside the abdomen separated by necrotic tissue unless it could be reduced at the time of injury and before the swelling had supervened in the protruding part. He protected the omentum from the air and prevented it from adhering to the edge of the wound by using a dry dusting powder. When the slough separated the stump retracted into the abdomen and the wound gradually healed. Up until this time, he records, the usual practice was to tie off the omentum and cut away the protruding portion, with resulting secondary hemorrhage, inflammation, and gangrene or death.6
For the first time, bullets were extracted from wounds by making a counteropening instead of probing the torn entry path of the bullet, and prophylactic incisions were made near bayonet wounds to let the pus flow out. The system of care he introduced was so successful that of 1,200 guardsmen wounded in the battle of Aspern-Essling in 1809 only forty-five died after treatment.7
For wound care Larrey substituted wet dressings for the dry lint mainly used at that time. He dipped his lint in hot wine to which he added camphor and irrigated the wound with an antiseptic solution. He also noticed the beneficial role of maggots on trauma.8 Larrey reported successful treatment of a transected ileum by exteriorization, the healing of sigmoid colon injuries without fecal fistula formation, and the successful treatment of lacerations of the bladder.9
The first successful pericardiocentesis for trauma
In March 1810, during the Napoleonic Wars, Baron Larrey encountered a situation which made him aware that blood under pressure from a heart wound could fill the unyielding covering of the heart and compress normal dilation of the chambers within. Larrey was the first to perform a pericardiotomy on a thirty-year-old soldier in the Imperial Guard with tamponade following a knife wound of the chest. Operating forty-five days after the injury, Larrey evacuated a serous fluid mixed with old blood clots and the patient’s condition first improved. Although he died three weeks later from an inevitable post-operative infection, the clear message was received.10
Not only a gifted surgeon but also a great man
There is no question about Baron Larrey’s character. He often faced the inherent dangers of enemy fire on the battlefield and did not receive any special exemption by the enemy despite the fact that they were on a humane mission – the Red Cross insignia and Geneva Convention had not yet been developed at that time. Larrey was often forced to engage in direct combat, armed only with a light sabre and pistol to defend himself and his patients.
He is best described in his own words: “To perform a task as difficult as that of a military surgeon, I am convinced one must often sacrifice oneself, perhaps entirely, to others, must scorn fortune, and must maintain an absolute integrity.”4
References
- Burris DG, Welling DR, Rich NM. Dominique Jean Larrey and the principles of humanity in warfare. J Am Coll Surg. 2004;198(5): 831-835.
- Ellis H. A history of surgery. Cambridge: Cambridge University Press; 2001.
- Skandalakis PN, Lainas P, Zoras O, Skandalakis JE, Mirilas P. To afford the wounded speedy assistance: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8): 1392-1399.
- Larrey DJ. Memoirs of military surgery and campaigns of the French armies. Hall RW, trans. Baltimore: Joseph Cushing; 1814.
- Hogan DE, Burstein J. Disaster medicine. Philadelphia: Lippincott, Williams and Wilkins; 2002, pp. 12.
- Munroe AR. Baron Larrey. Surgeon general to Napoleon’s army. Can Med Assoc J. 1943;48(2): 145-148.
- Robertson-Steel I. Evolution of triage systems. Emerg Med J. 2006;23(2): 154-155.
- Keegan J, Wheatcroft A. Who’s who in military history. 2nd Century Hutchinson Ltd; 1987, pp. 188-189.
- Hatzinger M, Ameijenda C, Lent V, Sohn M. Baron Dominique-Jean Larrey: the founder of urological traumatology. Aktuelle Urol. 2012;43(6): 389-391.
- Tóth I, Rami-Porta R, Rendeki S, Molnár TF. First steps in the management of pericardial effusion: who was first to relieve the pericardial sac – Larrey or Romero? World J Surg. 2013;37(9): 2242-2245.
STAVROS GOURGIOTIS graduated from the Medical School of Aristotelian University of Thessaloniki, Greece. He served in Special Forces of the Hellenic Army, completed surgical training in 2003 and was employed in the Army Health Service as Consultant Surgeon. He developed a special interest in HPB surgery as clinical fellow in UK. In 2007, he started employed in the ICU with special interest in trauma and emergency surgery. In 2009, he was the deputy of the chief of the surgical department in a military hospital in Kunduz-Afghanistan. He completed his PhD in 2013 and became FACS in 2014. He is now the head of the A&E Department at the 417 NIMTS Hospital.
Spring 2016 | Sections | War & Veterans

Leave a Reply