Edward McSweegen
Kingston, Rhode Island, United States
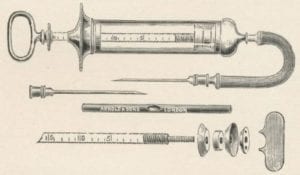 |
| Roux’s syringe for delivering antitoxin, The College of Physicians of Philadelphia. Source |
In March 2020, a research group in China reported the use of convalescent plasma to treat ten patients suffering from coronavirus COVID-19 infections.1 This type of therapy—passive immunization—dates back to 1891 when the German bacteriologist Emil von Behring used horse serum containing diphtheria antitoxin antibodies to treat a patient infected with Corynebacterium diphtheriae. It was a great success, and for decades antiserum therapy was the standard method for treating various bacterial infections.
Given the enormous morbidity and mortality associated with recurring epidemics of yellow fever (YF) in the Americas, it is not surprising that nineteenth-century bacteriologists searched for the etiological agent of the disease and then for specific curative or preventive therapies. When the Italian physician G. Sanarelli announced he had discovered the YF agent in 1897, he quickly set out to develop an antiserum to treat patients. Hearing about his YF antiserum, the Spanish government requested a quantity of it for use in Cuba in June 1898.2 One of America’s best YF experts, Henry Rose Carter, declared, “. . . even without pinning one’s faith to its efficiency it would seem unwise not to avail ourselves of what is probably a valuable prophylactic. . . .”3 In New York in the summer of 1899 a health officer named Alvah H. Doty produced an antiserum similar to Sanarelli’s and used it to treat several YF patients arriving in the city.4
 |
| Aristides Agramonte, MD, Wikipedia Source |
But Sanarelli’s bacterium was not the cause of YF and therefore his antiserum was ineffective. Still, even in the absence of a specific agent of infection, there were other avenues of treatment and prevention to explore. One was suggested in the pages of the Journal of the American Medical Association. A physician named C.C. Stockard wrote, “. . . the thought occurred to me that the blood of a person having had the disease should answer all the purposes as well as the serum prepared by the tedious process through animals. It would be a simple matter to take blood from the vein of an immune, preferably one recently recovered from the disease, and immediately inject it into the patient affected or one to be protected.”5
Aristides Agramonte, a Cuban-American investigating YF outbreaks among U.S. troops in Cuba, may have taken note of Stockard’s suggestion. In 1899 he treated five patients with serum collected from carefully selected YF patients. “The serum was obtained of convalescents from uncomplicated yellow fever; a careful scrutiny of their previous history was made so as to avoid bleeding men who had any syphilitic or tubercular antecedents . . .”6 In his report to the Army, Agramonte provided extraordinary details about his laboratory procedures, including the clinical details of his ten blood donors and the five YF patients receiving subcutaneous injections of convalescent sera. (Patient privacy was then an unknown concept and “informed consent” a vague idea).
Agramonte acknowledged “. . . four cases can hardly be considered as sufficient evidence upon which to base and final opinion . . .”6 Yet he had shown the importance of donor selection and that disease severity could be modulated by specific antisera. Timing was also important. One of his patients died because he received antiserum on the fifth day of his illness. (By then, the virus would have disappeared from the bloodstream, leaving little for donor antibodies to bind.) “Further investigation is necessary,” concluded Dr. Charles Fitzpatrick at New York’s quarantine station.7
But the U.S. Army may have inadvertently stopped further investigations in Cuba. A letter from the Army’s Adjutant General dated October 23, 1901 prohibited “any further experimentation among United States troops or civilian employees with yellow fever serum . . .”8 At the time, James Carroll, one of the members of Walter Reed’s YF Board, was using serum from acute YF patients to induce YF in naïve recipients. The resulting cases may have surprised Carroll because the serum was first passed through a Berkefeld filter, which held back bacteria.9 The agent of YF, whatever it was, was clearly smaller than common bacteria. But the October 23 order regarding “yellow fever serum” may have been interpreted so broadly as to preclude more of Agramonte’s passive immunization studies. In any case, by early 1901, Reed, Agramonte, Carroll and other public health physicians in Cuba were focusing on patient isolation and mosquito elimination as the most effective means of reducing the numbers of new YF cases.
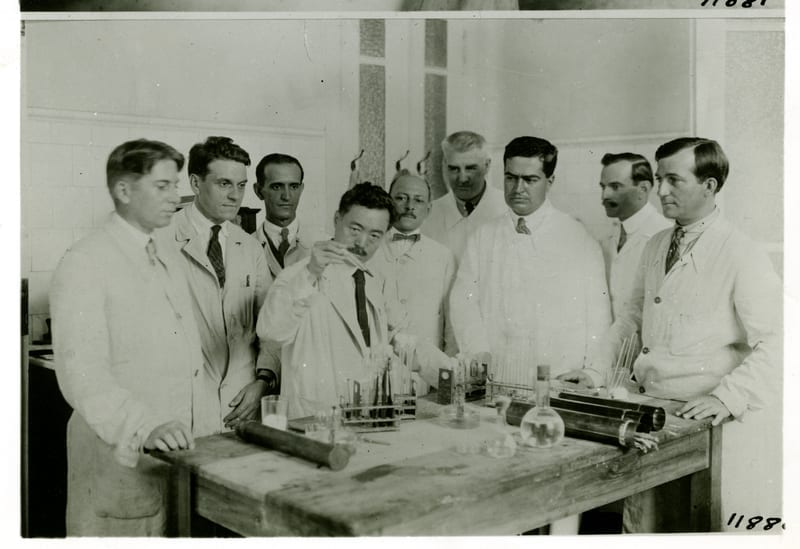 |
| Hideyo Noguchi in his laboratory, Rockefeller Foundation. Source |
The quest for a YF antiserum was thrown off track again in 1918. That year, the Rockefeller Foundation sent a research team to Ecuador to study YF. The team included Hideyo Noguchi, a well-regarded Japanese bacteriologist. There Noguchi identified a new spirochete, Leptospira icteroides, which he thought was the YF agent. Like Sanarelli before, he developed a vaccine and an antiserum, both of which failed to protect against YF.10
Despite such setbacks, there still was a need for effective passive immunization for treatment and preexposure prophylaxis. In 1931, for example, the Rockefeller Foundation reported thirty-two cases of laboratory-acquired YF and five deaths.10 Accidental exposures in the lab continued, and post-exposure treatment was not always beneficial owing to antiserum antibody levels and therapy timing. Primate studies demonstrated that immune serum given before exposure was protective. Immune serum given twenty-four hours after exposure protected only 55% of primates. Passive antibody given after clinical onset of disease was ineffective.11
The struggle for protection against exposure to the YF virus continued until Max Theiler developed an effective vaccine in 1937. Since then, over 400 million doses of the 17D vaccine have been administered worldwide.12
References
- Duan, K., et al. “Effectiveness of convalescent plasma therapy in severe COVID-19 patients.” PNAS, 2020, Apr. 6. DOI: 10.1073/pnas.2004168117.
- “Sanarelli Serum for Yellow Fever.” NYT, June 29, 1898. pp. 2. Available at: https://www.nytimes.com/1898/06/29/archives/sanarelli-serum-for-yellow-fever.html. Accessed: April 18, 20202.
- United States Marine Hospital Service. “Yellow Fever: Its Nature, Diagnosis, Treatment, and Prophylaxis.” Government Printing Office, Pp.52. June 15, 1898. Available at: https://bit.ly/2V08J9i. Accessed: April 18, 2020.
- Kotar, SL and Gessler JE. Yellow Fever: A Worldwide History. Jefferson, North Carolina: McFarland & Co., Inc. Publishers, 2017.
- Stockard, CC. “Human Serum in Yellow Fever.” JAMA, 1898;XXXI(5):252.
- Agramonte A. “Report of Bacteriological Investigations Upon Yellow Fever.” Medical News. 1900;76(7):249-256. Available at: https://bit.ly/2xENwZz. Accessed: April 18, 2020.
- Fitzpatrick, CB. “Remarks on the Bacterial Therapy of Yellow Fever.” JAMA, 1900;34 (14):905.
- James Carroll to Adjutant General on October 24, 1901. University of Maryland Baltimore. Available at: http://hdl.handle.net/10713/8314. Accessed: April 16, 2020.
- Pierce JR. “In the Interest of Humanity and the Cause of Science: The Yellow Fever Volunteers.” Mil. Med. 2003;168(11):857-863.
- Frierson, JG. “The Yellow Fever Vaccine: A History.” Yale J. Biol. Med. 2010;83:77-85.
- Plotkin, SA, et al. Plotkin’s Vaccines. Alpharetta, Georgia: Elsevier, Inc. 2018.
- Tan, SY and Pettigrew K. “Max Theiler (1899-1972): Creator of the yellow fever vaccine.” Singapore Med J. 2017;58(4):223–224.
EDWARD MCSWEEGEN, PhD, is a microbiologist in Rhode Island. He worked at the National Institute of Allergy and Infectious Diseases, and later at the Global Virus Network in Baltimore. He writes frequently about infectious diseases and history.
Spring 2020 | Sections | Infectious Diseases

Leave a Reply