Laura Kaplan
New York, New York, United States

Gustave Joseph Witkowski Wood print From Histoire des accouchements chez tous les peuples
For most of American history, pregnancy, labor and delivery, and post-partum have been dangerous periods for mother and child. However, starting slowly in the late 18th century and accelerating into the late 19th century, labor and delivery radically changed. Initially new medical interventions, such as forceps and anesthesia, caused as many issues as they seemed to resolve as they emerged in burgeoning medical school obstetric programs. But the introduction of standard physician training accompanied by an emphasis on infection control eventually led to substantially decreased morbidity and mortality in the mid-20th century. From a home-based event managed by female midwives and other birth attendants without formal training to a hospital-based, standardized encounter managed by formally trained male and female physicians and other healthcare practitioners, this complete paradigm shift resulted from women’s determination to have a safe and painless delivery, a new scientific foundation, innovations in medicine, and changes in the social landscape. (Fig 1)
Until the 20th century, the majority of US births occurred in the home, attended by female midwives and numerous female family and friends. As no formal training programs, curricula, licensing processes, or other official standards for birth attendants existed until the 18th century, women learned to help and support their loved ones through their own and others’ birth experiences. Historically, midwives—a diverse group of female community members who were usually married with children of their own—learned their skills by delivering their neighbors’ children or through loose apprenticeships with more established midwives. Only after the 1860s did some midwives begin attending midwifery schools. Midwives tended to intervene as minimally as possible and worked to assist labor along its natural course. Yet childbirth and the postpartum period long remained times of high morbidity and mortality.1,2
As American women in the 18th and 19th centuries had on average seven live births during their lifetimes—and potentially a number of undocumented early terminations—women’s diaries and letters reveal the considerable time women spent preparing for the pain and the realistic possibility of dying in childbirth. One 19th century woman wrote to her family late in her pregnancy: “If I live and regain my health, I will surely write to [all the people to whom she owed letters].”1 In 1885, another wrote about her third birth, “Between oceans of pain, there stretched continents of fear; fear of death and a dread of suffering beyond bearing.”1 In addition, women who survived childbirth and the postpartum period frequently suffered from lifelong morbidities, such as vesicovaginal and rectovaginal fistulas from unrepaired lacerations. The resulting lifelong incontinence and vaginal, cervical, and perineal prolapses of these fistulas caused painful sexual intercourse and difficulties with future pregnancies. A physician noted in 1897, “the wide-spread mutilation . . . is so common, indeed, that we scarcely find a normal perineum after childbirth.”1 Despite numerous uncertainties inherent in childbearing into the 20th century, American women persevered to control the process through the selection of childbirth attendants, preferring to deliver in a comfortable, safe setting (sometimes traveling back to their childhood home).1
American women first invited male physicians to assist in birthing rooms in the 1760s.1 Previously, physicians, who were exclusively male, were rarely called except in extreme emergencies, and men were excluded from attendance unless women were unavailable. In 1762, Dr. William Shippen, Jr. of Philadelphia, after training in midwifery in London and Edinburgh, became the first American male physician to establish a normal obstetrics practice in the US. Shippen also pioneered formal midwifery education through a lecture series initially taught to both male physicians and female midwives, but later limited to male physicians. Other physicians subsequently offered courses in other large American cities, and medical schools progressively incorporated obstetric education into their curricula.
As numbers of physicians formally trained in midwifery increased through the 19th century, the wealthy, urban elite—who perceived male physicians as superior in education and training—were progressively more inclined to pay the higher physician fees, presuming that the physician’s modern interventions would result in safer childbirth. Such women chose their physician attendants similarly to how they had chosen their midwife attendants. For instance, at the turn of the century, records showed that midwife birth attendants in both rural and urban Wisconsin primarily attended the labor of local women of similar ethnic backgrounds. For deliveries, city midwives in Milwaukee and Madison rarely traveled beyond wards contiguous to their own, and rural midwives rarely worked outside their township.2 Similarly, physicians tended to be from their immediate communities and of similar ethnic backgrounds. Even with the rise of railroad lines and automobiles in the 20th century, physicians’ practice areas did not significantly expand.2
New medical interventions that physicians employed—such as forceps, anesthesia, and laceration repair—increased the popular perception of the increased safety being provided in childbirth.1,3 In the early 19th century, the physicians’ primary interventions were forceps for difficult deliveries, bloodletting to relieve pain and accelerate labor, ergot to stimulate contractions, and drugs (particularly opium) for pain relief.1 The forceps were invented in the 1590s by Peter Chamberlen the Elder, a French Huguenot “male midwife” whose family had fled to England. Peter was one of the most famous male midwives in England, serving as the queen’s surgeon and delivering the children of multiple kings. He and his family kept the forceps as a family secret for over a century, reportedly performing deliveries under a sheet or blanket to guard their creation.
In the early 18th century, other practitioners developed their own versions of forceps, Dr. William Smellie of Scotland being the most well-known. Smellie taught midwifery and systemically described the proper use of forceps, publishing Treatise on the Theory and Practice of Midwifery in 1752.1,3 With the introduction of forceps, physicians were able to extract fetuses that had previously been undeliverable, which mothers viewed as miraculous. However, as no standards existed for when forceps should be employed, 19th century physicians were generally improperly trained in their use. As a result, individual practices differed substantially, and interventions frequently caused new problems. Some physicians used forceps routinely in every delivery even though their misapplication resulted in increased perineal lacerations, uterine trauma, and fetal defects. There was great debate among American physicians about the proper use and abuse of forceps throughout the 19th century.1
The introduction of anesthesia in the mid-19th century was a key milestone in the history of obstetrics. Based on reading of thousands of diaries and letters from parturient American women from the 18th and 19th centuries, Judith Walzer Leavitt concluded that “next to the fear of death, pain was probably the single part of birth most hated by birthing women.”1 After the first public demonstration of ether in 1846 by dentist William Morton at Massachusetts General Hospital in Boston,4 Fanny Appleton Longfellow was the first woman to use it during childbirth in 1847, writing, “I feel proud to be the pioneer for less suffering for poor, weak womankind. This is certainly the greatest blessing of this age.”1 Subsequently, wealthy women pressed physicians to use ether and chloroform to decrease their suffering. As with forceps, proper use of anesthesia was not standardized, and practice and debate varied tremendously about all aspects of its use, including when and whether to initiate it and appropriate dosing. Consequently, improper anesthetic use caused numerous complications, particularly prolonged labor due to decreased ability of the uterus to contract, newborn breathing difficulty, and hemorrhage.1
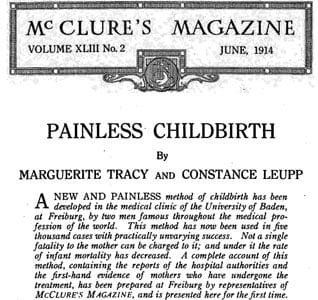
Due to the limitations of ether and chloroform, women and their physicians searched for a superior anesthetic.5 In the early 20th century, Austrian and German physicians—followed by American physicians a few years later—began experimenting with a combination of scopolamine and morphine in childbirth. Alone, scopolamine acts an as amnesic, erasing all later memory of childbirth. Given with an opiate, it also has an anesthetic effect. Scopolamine-morphine, named “twilight sleep,” permitted the patient to be semiconscious with intact contractions during labor, allowing the physician to coach the woman through childbirth without her remembering the experience afterwards. In 1914, McClure’s magazine published “Painless Childbirth,” in which two laywomen raved about German Drs. Karl Gauss and Bernhardt Kronig’s twilight sleep protocol, but lamented the American physician’s inadequate training in the method.

Immediately, a vocal contingent of American women embraced and advocated for twilight sleep for their deliveries, and numerous articles and books were published on the subject.5 From 1914–1915, the National Twilight Sleep Association—organized by wealthy upper- and middle-class women and led by prominent leaders such as Dr. Bertha Van Hoosen in Chicago and Mrs. Francis X. Carmody—advocated relentlessly for physicians and women to adopt twilight sleep, which allowed painless childbirth. In the words of Mrs. Carmody: “the twilight sleep is wonderful but, if you women want it you will have to fight for it, for the mass of doctors are opposed to it.”5 As with other innovations, twilight sleep suffered from widespread controversy over in the medical community and enormous discrepancy in practice. Despite the drug’s amnesic effects, women under scopolamine still experienced intense labor pains, screaming and thrashing so much during labor that they were placed in “crib beds” to avoid accidents.1
By the summer of 1915, twilight sleep sharply declined in popularity. Inappropriate use of the drug by physicians had frequently led to adverse events, including maternal delirium and asphyxiation of newborns. Notably, in August 1915, Mrs. Carmody died in childbirth while under scopolamine’s influence. Her physicians and husband maintained that her death did not result from scopolamine use; however, her neighbor Mrs. Alice J. Olsen initiated a campaign against twilight sleep in response to the event. As the drug’s popularity decreased, doctors limited scopolamine use to the first stage of labor, when it was still considered safe.5
Though the twilight sleep movement was brief, it had long-lasting repercussions. The drug’s promise of a painless childbirth propelled women and their physicians to increasingly seek drugs and other means to ensure that childbirth would be as painless as possible.1 This pursuit, in the context of the twilight sleep movement, brought many women—who otherwise would have chosen home deliveries—to the hospital to avoid numerous problems with home scopolamine administration.
As infection was one of the leading causes of postpartum death, infection control also attracted women to physician-attended labor in hospitals.1 However, while American Dr. Oliver Wendell Holmes and Austrian Dr. Ignnaz Semmelweis recommended careful handwashing to prevent doctor-to-patient transmission of infection in the 1840s, it was Koch, Pasteur, and others’ revolutionary work on bacteria in the late 1860s that propelled the infection control movement in labor and delivery. By the 1880s, increasing numbers of physicians adopted infection control methods, though debates on the matter persisted for decades.
Early methods of antisepsis included vaginal chloral douches (injections of antiseptics into the vagina before and after delivery) and strict scrubbing of the genital area and physician’s hands (with numerous specific recipes and protocols). By the turn of the century, rubber gloves, a rubber “Kelly pad” (a rubber sheet placed under the patient for discharges), and shaving of the genital area were standard recommendations for practicing physicians. Initially, physicians tried to incorporate antisepsis as much as possible in home birthing rooms. However, in the first decades of the 20th century, they began to encourage patients to come to hospitals for truly sterile births, as it was difficult to guarantee the cleanliness of the patient’s home and adherence of other birth attendants to their practices.1
Other non-medical developments led to changes in women’s childbirth practices in the US, including the “mystification of medical knowledge” and the breakdown in women’s social networks for childbirth. With advances in obstetrics, women believed the promise of “science” could alleviate dangers and fears surrounding childbirth. Early 20th century women’s journals and American women advised each other to select a trustworthy physician and follow his guidance, as he knew best. In addition, with increased mobility and urbanization in the 19th and 20th centuries, women no longer had the same expanded social support for pregnancy. The idea of a hospital where nurses and physicians took care of all of their needs was very appealing.1
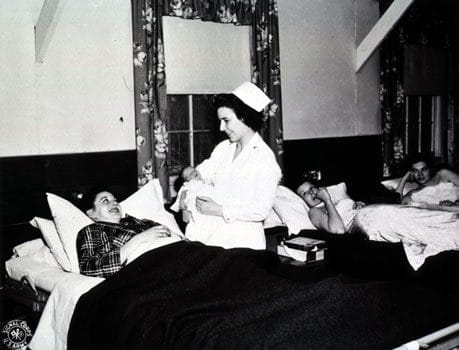
Hospital deliveries through the 1940s were entirely different from home deliveries, however. At home, the parturient exerted control over procedures and anesthesia administered by birthing attendants; in the hospital, women had no input into the drugs and procedures they received. Through the 1940s, hospital births frequently left women disillusioned and terrified, often contributing to psychiatric distress for extended periods after delivery. One woman wrote: “Months later I would scream out loud and wake up remembering that lonely labor room and just feeling no one cared what happened to me, no one kind reassuring word was spoken by nurse or doctor. I was treated as if I was an inanimate object.”1
Interestingly, despite their promise, the numerous advances in obstetric medicine in the 19th and first decades of the 20th centuries did not immediately translate to improved safety during labor and the postpartum period.1,2 Though hospital births were believed to be safer, there was no decrease in maternal mortality between hospital and home births until the 1940s. Despite strides in obstetric knowledge, practical training in medical school remained limited in the first decades of the 20th century. Faculty lectures, student recitations, and practice with a manikin largely comprised the obstetric curriculum at most medical schools. While some schools had courses devoted to pelvic exams and delivery with and without obstetric instruments using a manikin, until 1900, the majority of medical students observed at most one to two deliveries in either the lecture hall or the patient’s home—and many never witnessed one. Famous obstetrician Dr. Joseph DeLee, who graduated from Northwestern, later recalled that he felt lucky to have observed two deliveries as a medical student.
The publications of the 1910 Flexner Report and Dr. J. Whitridge Williams of Johns Hopkins’s 1914 survey of American medical schools’ obstetrics departments both showcased medical schools’ failures in obstetric education. As a result, medical schools labored to increase the number of births witnessed by medical students.1 For decades, this was an uphill battle. Consequently, new physicians continued to be poorly trained to handle deliveries, and practicing physicians still lacked standards of practice to ensure the safety of delivery interventions.2 Lacking such standards, physicians during this period routinely over-utilized forceps, drugs to accelerate delivery, episiotomies, and other interventions—despite ongoing debate in the medical literature—in order to distinguish themselves from low-interventionalist midwives. Through the 1920s, mortality rates for midwife- and physician-assisted births remained similar, with physician assisted delivery possibly faring worse.
In the 1930s and 40s, American physicians—largely wealthy, native-born, white males—increasingly differentiated themselves from traditional midwives—chiefly working-class immigrants and African Americans—through standardized medical school curricula, formal credentials for practice, and professional societies with the authority for self-regulation.1 In addition obstetric specialists also endeavored to establish obstetrics as its own hospital-based specialty, arguing that poorly trained general practitioners, who were “responsible for many obstetrical disasters” needed to cease obstetric work. In addition to establishing obstetrics’ role in the hospital, obstetric specialists redefined the medical philosophy of birth. Contrary to previous depictions of birth as a natural, though painful and dangerous, process, the new obstetricians, such as Dr. Joseph DeLee, deemed birth a “pathologic process” that required close medical supervision. Obstetric specialists formed professional associations, such as the American Congress of Obstetricians and Gynecologists (ACOG) in 1930. By 1936, ACOG was certifying specialists, with the authority to determine who could establish a hospital-based practice.
From the turn of the century on, women increasingly opted to deliver with physicians over midwives—initially with familiar community doctors and then with hospital-based physicians. In 1900, midwives still delivered half of all US births, but by 1930, this number dropped to less than 15% of US births, primarily in the South.2 Similarly, in 1900, less than 10% of American births occurred in a hospital. By 1940, 26.7% of non-white and 55% of white American births took place in a hospital, increasing to 56% (non-white) and 88% (white) by 1950.1 It was at the turn of the century, when births became more prevalent in the hospital, that physician-assisted birth no longer became the purview of the wealthy; very poor and/or single women who lacked other alternatives also utilized physicians as birth attendants.1
During this period, physicians and hospitals learned to standardize obstetric practices to reduce mortality, such as appropriate use of drugs, proper indications and contraindications for obstetric procedures, and improved methods of antisepsis. Later developments of antibiotics, blood transfusions for hemorrhages, and prenatal care for high risk patients significantly contributed to the decline in maternal mortality. As maternal mortality rates fell in the 1940s and 1950s, women sought to regain some control, decision-making power, and humanity in the birth process that they had for millennia prior to the move to the hospital. In this environment, the natural childbirth movement and other philosophies of childbirth as a natural, normal process in which women possess control developed beginning in the 1950s–60s.1
Birth in America changed dramatically from the colonial period to the 20th century. The development of obstetrical “science” and numerous innovations including forceps, anesthesia, and antisepsis transformed childbirth into a standardized process that women no longer feared. Originally occurring at home in a familiar bed supported by female midwives, family, and friends, childbirth moved to a sterile hospital environment accompanied by male and female health professionals and select loved ones. By the middle of the 20th century, these changes coincided with significant reductions in morbidity and mortality as a result of childbirth. By actively seeking safer and less painful childbirth and slowly allowing physicians and their developing technology to attend to them, parturient women changed the natural history and their personal experiences of childbirth.
Notes
- Judith Walzer Leavitt, Brought to Bed: Childbearing in America 1750–1950 (New York: Oxford University Press, 1986).
- Charlotte G. Borst, Catching Babies: The Professionalization of Childbirth (1870–1920) (Cambridge: Harvard University Press, 1995).
- J. Drife, “The Start of Life: A History of Obstetrics,” Postgraduate Medical Journal 78 (2002): 311–315, http://pmj.bmj.com/content/78/919/311.full.
- James F. Crenshaw and Elizabeth A. M. Frost, “The Discovery of Ether Anesthesia: Jumping on the 19th-century Bandwagon,” Archives of Family Medicine 2 (May 1993): 481–484.
- Amy Hairston, “The Debate Over Twilight Sleep: Women Influencing Their Medicine,” Journal of Women’s Health 5, no. 5 (1996), http://www.liebertonline.com/doi/pdf/10.1089/jwh.1996.5.489.
LAURA KAPLAN, MD, studied the history of science, medicine, and technology as an undergraduate at Johns Hopkins University and wrote this paper as a fourth-year medical student in Dr. Mindy Schwartz’s History of Medicine course at the University of Chicago. She is now a Family Medicine resident at Beth Israel Medical Center in New York.
Highlighted in Frontispiece Volume 4, Issue 4 – Fall 2012
