Mariel Tishma
Chicago, Illinois, United States
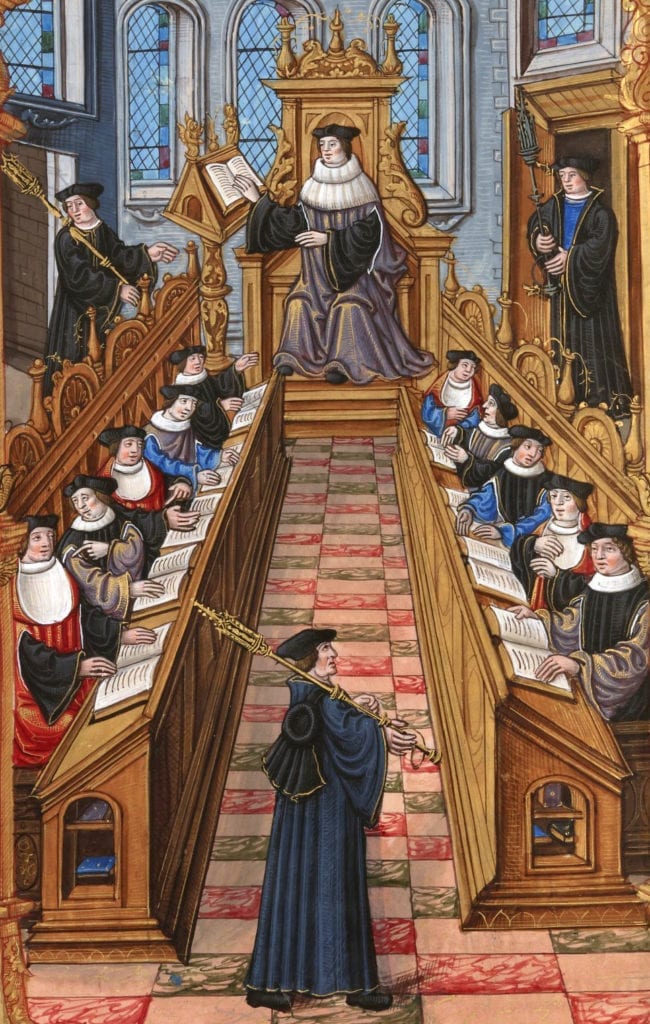 |
| A meeting of doctors at the university of Paris. From the “Chants royaux” manuscript, Bibliothèque Nationale, Paris. BNF, Français 1537, fol. 27v. Source |
In November 1322 a group of folk healers and empirics were put on trial by the Faculty of Medicine from the University of Paris. Their crime was practicing medicine without licenses issued by the university. The punishment was excommunication and a fine of sixty Parisian livres.1
Among the group was a woman, Jacoba (or Jacqueline) Felicie de Almania. To understand what led to her trial, it is essential to unpack the state of medicine and gain insight into the work of women at that particular time.
It was around 1154 that regulating bodies controlled by universities, religious groups, and government officials began issuing licenses, naming who was legally allowed to practice medicine.2 Regulations would become commonplace by the thirteenth and fourteenth centuries.3,4 The education required by licensing bodies was on par with careers in law and theology, and it created a new elite class. But it required separation from the barber surgeons and empirics who practiced with their hands, a feat achieved through strict adherence to theory and disregard for practical education.5
To treat patients successfully was no longer enough to call oneself a physician. Self-trained physicians could apply herbs and cure a condition, but a licensed physician could explain their cures using concepts such as humoral theory, which was growing in importance.6 Only formally educated, licensed physicians had this theoretical knowledge.7 Consequently, the tension between university-educated physicians and self-taught barber surgeons, empirics, and folk healers was high.
The primary forms of education for licensing were medical texts purchased independently and university schooling. This created barriers for many wanting to pursue medicine, but the hurdles were higher for women. Often, women were not taught to read or write in Latin,8 the preferred language of medicine. They were forbidden from attending most universities.9,10 Excluded from education, public perception of female healers became a self-fulfilling spiral. Women were not allowed to be educated, so they must not have been intelligent enough to be educated, and so they must have been incapable of practicing as doctors.
However, at this time there were few official physicians, and so treatment from these persons was hard to access. Schools and testing bodies simply could not produce enough graduates—male or female—to keep up with the needs of the population.11 Most people had to look elsewhere and, in reality, medicine was practiced on a graduated scale, ranging from university-trained physicians to empirics and other healers. Women could be found throughout this graduated scale, but their accomplishments are difficult to find because they were not often recorded. Only the extraordinary—those convicted, published, or praised—were recorded in the documents that have survived today.12
Some claim women had exclusive control over birth and midwifery at this time, and female midwives and birth attendants were fairly ubiquitous. However male midwives or physicians still participated in births, and women did not exclusively seek female attendants. In certain cases, women served as assistants to male physicians, performing manual inspections of female patients and relaying the information to the physician to preserve modesty.13
Outside of birth, small issues like minor cuts and common sicknesses could be handled at home. This treatment was often administered by women in their role as caregivers and may have evolved into more formal practice outside the family unit.14,15 Other patients may have found healing at a hospital where much of the actual work was done by nuns and religious sisters, often led by a formally trained physician.16
It is in this climate that Jacoba Felicie lived and worked, and it is under these conditions that she was put on trial. The treatment of Jacoba’s case is undeniably tied to issues of gender but her accusation was not specifically a gendered issue. The Faculty of Medicine tried Jacoba as part of a group of both men and women. Their goal was to create a more rigorous practice and controlled image of medicine.17
Little is known about the life of Jacoba Felicie. She was a Parisian healer whose story of family and life after her trial has been lost. There is only one document that mentions her, and it is focused exclusively on her practice. That document, including the recounting of witnesses who received her care, is one of the most complete records of a female medical practice from her time.18
We assume that Jacoba was self-trained, or trained by someone else practicing empiric medicine. We know that she took on many patients that formally trained doctors deemed incurable or had treated but not cured. Jacoba only charged for treatment if she was successful at curing her patient, and so she could not be categorized as a quack physician who used medicine to make a profit. One of her patients when called to the witness stand recalled, “When he was asked if he had made a contract with her about curing him, he said that he had not. After he had been made well he paid her as he wished. . . .”19 Her payment system also made her a more attractive option for the common people, elevating her reputation. But charging any sort of fee for healing was considered inappropriate for a woman at that time.
Many of Jacoba’s techniques were the same as theoretical licensed physicians. They included taking the pulse, examining urine, and administering prescriptions.20 As one witness recounted, “[Jacoba] inspected her urine and felt her pulse, and afterwards gave her a certain clear liquid to drink.”21 This suggests that Jacoba knew enough to be regarded as a professional. But it was considered highly improper for anyone other than licensed physicians to use these techniques, furthering the case against her.22
During the trial, Jacoba and her defense argued that though she had been practicing without a license, she had saved many lives, perhaps more than the doctors prosecuting her. Also, as she was a female physician, she had done much to help women who may have felt unable to share their issues with a male physician. She stated:
“It is better and more becoming that a woman clever and expert in the art should visit a sick woman. . . . a woman would allow herself to die before she would reveal the secrets of her illness to a man. . . . Thus it is that the laws say that lesser evils should be permitted, so that greater ones may be avoided.”23
Eight witnesses were called. They were a group of men and women from all layers of society who had sought treatment from Jacoba for symptoms ranging from fever to paralysis and weakness.24 One of her patients, a religious brother named Odo, was treated by sweating over coals and burning herbs. He said, “Jacqueline was wiser in the art of surgery and medicine than any master physician or surgeon of Paris.”25 Another, a woman named Bilbaut, had been so paralyzed by her illness that she was unable to speak and had been left for dead by the licensed physicians.26
Jacoba maintained that the licensure law applied only to individuals who were endangering others by practicing poorly. She had proven her skill, and so should not be punished.27,28 However, she was never tested on her knowledge during her trial.29 The prosecution did not believe she could be as skilled as she appeared to be.
In the end, Jacoba was convicted on the argument that because women could not be lawyers, they could not be doctors. As one male expert consulted by the university suggested:
“It was forbidden by law that a woman practice law or be a witness in a criminal case, so it was of far greater moment that she be likewise barred from the practice of medicine. . . . How much more serious . . . was the danger that she might thus kill a man by these potions and clysters than that she might lose a civil suit through ignorance of the law. For through lack of knowledge in the former she might commit murder, and such a death would be a mortal sin over which the church would have jurisdiction.”30
This ignored the banning of women from universities to attain the knowledge needed, the assertion of the witnesses, Jacoba’s statements of her skill, and her suggestions around the importance of female physicians to mitigate modesty issues. It came down to this: because women were not allowed to be physicians, Jacoba could not have been practicing successfully, no matter the evidence.
After the trial, she and the other accused were excommunicated. Jacoba vanished from history. But court cases continued, suggesting that women (and others) were still practicing, regardless of potential punishment. Jacoba was only one of the women who was caught, after all. Many more unknown women were healing outside of the spotlight.31
There is much to take away from the story of Jacoba Felicie de Almania. First is a reminder of the politics that determine who is allowed to practice medicine and that shape our image of who can be a doctor. Proper education and licensing are undoubtedly important, but the path to those achievements is not equally easy and should be analyzed for barriers we may not realize are there. We can also learn from Jacoba’s hands-on experience. In Jacoba’s day, the theoretical, licensed physicians spent much of their time reading, thinking, and writing. They were no more effective than empirics, and in some cases were less so. It was Jacoba’s practice of medicine that allowed her to succeed where they did not.
Most of all, her story shines a light on the hidden history of women healers before medicine became the profession we know today.
End Notes
- Monica H. Green, “Getting to the Source: The Case of Jacoba Felicie and the Impact of the Portable Medieval Reader on the Canon of Medieval Women’s History,” Medieval Feminist Forum: A Journal of Gender and Sexuality 42, no. 1 (2006): 50, https://doi.org/10.17077/1536-8742.1057.
- Abigail Casey, “Magic and Medicine in a Man’s World: The Medieval Woman as both Healer and Witch,” Proceedings of The National Conference On Undergraduate Research (NCUR) 2016, (April 7-9, 2016): 1517, http://www.ncurproceedings.org/ojs/index.php/NCUR2016/article/view/1937/1039.
- John F. Benton, “Trotula, Women’s Problems, and the Professionalization of Medicine in the Middle Ages,” Bulletin of the History of Medicine 59, no. 1. (Spring1985): 30, https://www.jstor.org/stable/44452036.
- William L. Minkowsli, “Women Healers of the Middle Ages: Selected Aspects of Their History,” American Joumal of Public Health 82, no. 2 (February 1992): 292-293, Vern L. Bullough, “Status and Medieval Medicine,” Journal of Health and Human Behavior 2, no. 3 (Autumn, 1961): https://www.jstor.org/stable/2948986.
- Vern L. Bullough, “Status and Medieval Medicine,” Journal of Health and Human Behavior 2, no. 3 (Autumn, 1961): https://www.jstor.org/stable/2948986.
- Monica H. Green, Making Women’s Medicine Masculine: The Rise of Male Authority in Pre-Modern Gynaecology, (Oxford: Oxford University Press, 2008), 4-5.
- Monica H. Green, “Gendering the History of Women’s Healthcare,” Gender & History, 20 no.3 (November 2008): 495, https://www.academia.edu/4754544/Monica_H._Green_Gendering_the_History_of_Women_s_Healthcare_Gender_and_History_Twentieth_Anniversary_ Special_Issue_20_no._3_November_2008_487-518.
- Ibid.
- Minkowsli, “Women Healers,” 293.
- Casey, “Magic and Medicine in a Man’s World” 1520.
- Benton, “Trotula, Women’s Problems,” 30.
- Monica Green, “Women’s Medical Practice and Health Care in Medieval Europe,” Signs 14, no. 2, Working Together in the Middle Ages: Perspectives on Women’s Communities (Winter, 1989): 444, https://www.jstor.org/stable/3174557.
- Monica Green, “Women’s Medical Practice,” 438-439, 468.
- Montserrat Cabré, “Women or Healers? Household Practices and the Categories of Health Care in Late Medieval Iberia,” Bulletin of the History of Medicine 82, no. 1, Special Issue: Women, Health, and Healing in Early Modern Europe (Spring 2008): https://www.jstor.org/stable/44448505.
- Mary E. Fissell “Introduction: Women, Health, and Healing in Early Modern Europe,” Bulletin of the History of Medicine 82 (February 2008): 14, DOI: 10.1353/bhm.2008.0024.
- Green, “Gendering” 495.
- Pearl Kibre, “The Faculty of Medicine at Paris, Charlatanism, and Unlicensed Medical Practices in the Later Middle Ages,” Bulletin of the History of Medicine, Vol. 27, No. 1 (January-February, 1953): 2, https://www.jstor.org/stable/44443718.
- Green, “Getting to the Source,” 49-53.
- Medieval Medicine: A Reader ed. Faith Wallis, (Toronto: University of Toronto Press, Higher Education Division, 2019), 367.
- Ibid. 366.
- Michèle Le Doeuff, The Sex of Knowing, Trans. Kathryn Hamer and Lorraine Code, (New York: Taylor & Francis, 2003), 76.
- Medieval Medicine: A Reader 368.
- Ibid. 368-369.
- Ibid. 368.
- Penny S. Gold, “A Medieval Tapestry,” review of A Small Sound of the Trumpet: Women in Medieval Life, by Margaret Wade Labarge, The Women’s Review of Books. 4, No. 6 (Mar., 1987), p. 15, https://www.jstor.org/stable/4020079.
- Medieval Medicine: A Reader, 368.
- Green, Making Women’s Medicine Masculine, 15.
- Medieval Medicine: A Reader, 368.
- Minkowsli, “Women Healers,” 293.
- Pearl Kibre, “The Faculty of Medicine at Paris, Charlatanism,” 8.
- Minkowsli, “Women Healers,” 293.
Bibliography
- Benton, John F. “Trotula, Women’s Problems, and the Professionalization of Medicine in the Middle Ages.” Bulletin of the History of Medicine 59, no. 1. (Spring1985): 30-53. https://www.jstor.org/stable/44452036.
- Bullough, Vern L. “Status and Medieval Medicine.” Journal of Health and Human Behavior 2, no. 3 (Autumn, 1961): pp. 204-210. https://www.jstor.org/stable/2948986
- Cabré, Montserrat. “Women or Healers? Household Practices and the Categories of Health Care in Late Medieval Iberia.” Bulletin of the History of Medicine 82, no. 1, Special Issue: Women, Health, and Healing in Early Modern Europe. (Spring 2008): 18-51. https://www.jstor.org/stable/44448505
- Casey, Abigail “Magic and Medicine in a Man’s World: The Medieval Woman as both Healer and Witch.” Proceedings of The National Conference On Undergraduate Research (NCUR) 2016 (April 7-9, 2016): 1515-1524. http://www.ncurproceedings.org/ojs/index.php/NCUR2016/article/view/1937/1039
- “The Faculty of Medicine at Paris, Charlatanism, and Unlicensed Medical Practices in the Later Middle Ages.” Bulletin of the History of Medicine, Vol. 27, No. 1 (January-February, 1953), 1-20. https://www.jstor.org/stable/44443718.
- Fissell, Mary E. “Introduction: Women, Health, and Healing in Early Modern Europe.” Bulletin of the History of Medicine 82 (February 2008): 1–17. DOI: 10.1353/bhm.2008.0024.
- Green, Monica. “Women’s Medical Practice and Health Care in Medieval Europe.” Signs 14, no. 2, Working Together in the Middle Ages: Perspectives on Women’s Communities (Winter, 1989): 434-473. https://www.jstor.org/stable/3174557.
- Green, Monica H. “Gendering the History of Women’s Healthcare.” Gender & History, 20 no.3 (November 2008): 487–518. Pages. https://www.academia.edu/4754544/Monica_H._Green_Gendering_the_History_of_Women_s_Healthcare_Gender_and_History_Twentieth_Anniversary_ Special_Issue_20_no._3_November_2008_487-518.
- Green, Monica H. “Getting to the Source: The Case of Jacoba Felicie and the Impact of the Portable Medieval Reader on the Canon of Medieval Women’s History.” Medieval Feminist Forum: A Journal of Gender and Sexuality 42, no. 1 (2006): 49-62. https://doi.org/10.17077/1536-8742.1057.
- Green, Monica H. Making Women’s Medicine Masculine: The Rise of Male Authority in Pre-Modern Gynaecology. Oxford: Oxford University Press, 2008.
- Gold, Penny S. “A Medieval Tapestry.” Review of A Small Sound of the Trumpet: Women in Medieval Life, by Margaret Wade Labarge. The Women’s Review of Books. 4, No. 6 (Mar., 1987), p. 15. https://www.jstor.org/stable/4020079.
- Le Doeuff, Michèle. The Sex of Knowing. Trans. Kathryn Hamer and Lorraine Code. New York: Taylor & Francis, 2003.
- Livingston, Ryleigh S. “Women in Medicine: Past, Present, & Future.” Honors Thesis, Southern Illinois University Carbondale, 2015. https://opensiuc.lib.siu.edu/cgi/viewcontent.cgi?article=1401&context=uhp_theses.
- Medieval Medicine: A Reader. ed. Faith Wallis, Toronto: University of Toronto Press, Higher Education Division, 2019.
- Minkowsli, William L. “Women Healers of the Middle Ages: Selected Aspects of Their History.” American Journal of Public Health 82, no. 2 (February 1992): 288-295. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1694293/pdf/amjph00539-0138.pdf
- Ross, James Bruce, and Mary Martin McLaughlin The Portable Medieval Reader. New York: Penguin Classics, 1977.
- Schmermund, Elizabeth. Women in Technology. New York: Enslow Pub Inc, 2017.
MARIEL TISHMA is the Executive Editorial Assistant at Hektoen International. She has been published in Hektoen International, Bloodbond, Argot Magazine, Syntax and Salt, The Artifice, and Fickle Muses. She graduated from Columbia College Chicago with a BA in creative writing and a minor in biology. Learn more at marieltishma.com.
Highlighted in Frontispiece Volume 12, Issue 4 – Fall 2020
Spring 2020 | Sections | History Essays

Leave a Reply