Alexandria Szalanczy
Winston-Salem, North Carolina, United States
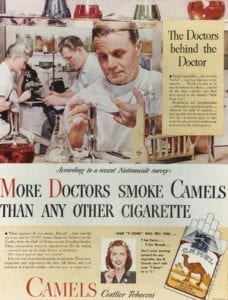 |
| “More Doctors” Advertisment. Camel Cigarettes. 1946. Released and uploaded by the Food and Drug Association, https://www.flickr.com/photos/fdaphotos/7029895715. |
Long before physicians faced a nation crippled by an opioid crisis, their predecessors lived and worked in a nation dominated by cigarettes. By 1953, 47% of Americans smoked cigarettes, including half of all physicians.1 These physician smokers were particularly instrumental to the rise of the cigarette in America. Beginning as early as the 1920s, the tobacco industry began marketing cigarettes based on purported health advantages and relied on physician support in advertising tobacco.2 Physicians were crucial to the growth of the tobacco industry since patients would address smoking-related health concerns with their doctors, and companies would court both individual physicians and their professional organizations in order to promote their products.3 As most of the significant health effects of cigarette smoking had not yet developed, research in the 1930s failed to connect smoking to serious illnesses and had “the perverse effect of exonerating the cigarette.”4 Physicians themselves continued to smoke. Who would believe that cigarettes were dangerous to their health if they saw their doctor smoking the same thing?
As more and more people began to smoke in the first half of the twentieth century, lung cancer rates began to spike and perceptions slowly began to shift.5 Beginning in the 1950s, reports were published linking cigarettes to lung cancer.6,7 In 1953 Wynder, Graham, and Croninger confirmed that condensed cigarette tar was carcinogenic, marking a turning point in the relationship between the tobacco industry and physicians.8 Tobacco executives employed medical doctors and academic scholars to defend cigarettes against mounting concerns by claiming that the evidence was insufficient to reach a scientific conclusion.9,10 But in December 1953 the executives met with a public relations firm that still advised the industry to steer away from health claims regarding cigarettes, which had been the centerpiece of their advertising campaigns for the previous twenty years.11 Other public relations campaigns also sought to attest to the safety of their new filtered cigarettes, whose market increased dramatically in the 1950s—even if the filters did little to actually filter.12 Despite these efforts, by 1954 there were no more advertisements utilizing the image of a physician to market cigarettes, and cigarette advertisements were banned from the Journal of the American Medical Association (JAMA).13 Physicians themselves moved away from smoking cigarettes—a little over half of all physicians smoked in 1954, but by 1959 the percentage had decreased to 39%.14 Today, fewer than 4% of American physicians smoke.15 The tobacco industry, which had for so long relied on physician approval and support, hit the first of its roadblocks.
Professional and public opinion on the negative health effects of cigarettes was validated by the 1964 report of the Surgeon Generals Advisory Committee (SGAC). The Kennedy administration assembled the SGAC after the 1962 Royal College of Physicians report from the United Kingdom concluded cigarettes to be a cause of lung cancer.16 The SGAC considered data from animal, epidemiological, clinical, and autopsy studies. Based on the evidence from these studies, the committee concluded there was a causal relationship between cigarette smoking and lung cancer.17 More importantly, it also concluded that “cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action.” 18 This should have been a fatal blow to the tobacco industry, yet even with this report, change was slow. It was only in 1978, fourteen years after the SGAC report, that the American Medical Association (AMA) publicly acknowledged the harm caused by cigarettes.19 And the tobacco industry, having lost the health appeal of cigarettes, adjusted their message—total per capita consumption of cigarettes still rose from 1964 to 1975 due to a significant increase in the number of young people smoking, as advertisements began pushing cigarettes as a way to look sexy.20,21 This is not to say that progress has not been made at all. In 2011, less than 20% of U.S. adults were smokers, half of what it was in 1965.22,23 This drop has been estimated to have saved eight million lives from smoking-related deaths in the United States from 1965 to 2010.24 The opinion of medical professionals was instrumental in swaying public opinion against cigarettes and averting these losses. Yet during that same time period, twenty million deaths were attributed to smoking.25 How many could have been prevented if physicians had not supported the tobacco industry for so many years?
Now, decades later, a new generation of physicians face their own crisis: a national problem of opioid addiction. In a twist of fate, more people now abuse prescription opioids than use tobacco.26 This new crisis, and the role that physicians have in its making, mirrors the rise and eventual fall of the cigarette in the twentieth century. As the addictive effects of nicotine were being realized and anti-smoking campaigns grew in intensity, the opioid epidemic was in its fledgling stages.27,28 Opioid manufacturers perfected techniques used by the tobacco industry on marketing their drugs—they sought out physicians through advertisements in medical professional publications and purposefully misled consumers about the addictive tendencies of their products.29,30 And the physician stance on prescribing pain pills has changed just as it once did with cigarettes. Twenty years ago, when physicians were frequently castigated for ignoring patient pain, they were encouraged to prescribe more pain pills. Now that the narrative has shifted, there is pressure against prescribing pills.31,32,33
But there are complexities that underlie the opioid crisis that were not present for the tobacco problem. What distinguishes the pain pill epidemic from the tobacco problem of the twentieth century? Not smoking cigarettes does not hurt a patient—but without pain management patients can be left in crippling condition and out of work.34 This traps doctors in a tough situation, since they want to help patients who are demanding relief but current evidence suggests that the narcotics are doing more harm than good.35 No studies have investigated the long-term ability of narcotics to treat chronic, non-cancer pain effectively, but other studies demonstrated that these patients were less likely to recover function.36 Refusing to prescribe narcotics either leaves patients seeking expensive alternative treatments or drives them away from the physician’s office.37,38 But over-prescribing pain pills has led to this current crisis; in 2016 alone, the majority of 60,000 overdose deaths were from opioids.39 This new epidemic promises to be even more pervasive and difficult to overcome than the issue of cigarettes and nicotine addiction.
The industries behind these products cannot be relieved of culpability, given their efforts to promote their products while hiding the negative health impacts. Yet physicians also have a history of failing patients, whether by encouraging patients to smoke cigarettes or by prescribing unnecessary opioids. There is no clear answer on how to balance patient safety with patient happiness, but it is a challenge that every modern physician will face. Perhaps through looking at previous mistakes on how the medical community handled tobacco and cigarettes, we can find ways to navigate today’s mistakes and prevent these blunders from occurring again in the future. We know from the story of the tobacco cigarette that it is possible to overcome mistakes from the past and to mitigate further damage. However, this is new territory that a physician cannot traverse alone. Only if the medical community takes ownership of its part in these sagas can we begin to take steps towards making things right.
End notes
- Michael K. Cummings and Robert N. Proctor, “The Changing Public Image of Smoking in the United States: 1964-2014,” in Cancer Epidemiology, Biomarkers, & Prevention 23 (2014): 33.
- Martha N. Gardner and Allan M. Brandt, “‘The Doctors’ Choice is America’s Choice’: The Physician in US Cigarette Advertisements, 1930-1953,” in American Journal of Public Health 96 (2006): 223-224.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 225.
- Howard Markel, “Tracing the Cigarette’s Path from Sexy to Deadly,” New York Times, March 20, 2007, https://www.nytimes.com/2007/03/20/health/20essay.html.
- Anthony J. Alberg, Donald R. Shopland, and K. Michael Cummings, “The 2014 Surgeon General’s Report: Commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and Updating the Evidence on the Health Consequences of Cigarette Smoking,” American Journal of Epidemiology 179 (2014): 404.
- Cummings and Proctor, “The Changing Public Image of Smoking,” 33.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 405.
- Ernest L. Wynder, Evarts A. Graham, and Adele B. Croninger, “Experimental Production of Carcinoma with Cigarette Tar,” Cancer Research 13 (1953).
- Cummings and Proctor, “The Changing Public Image of Smoking,” 33.
- Ronald Fisher, “Cigarettes, Cancer, and Statistics,” The Centennial Review of Arts & Science 2 (1958): 151-166.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 229.
- Cummings and Proctor, “The Changing Public Image of Smoking,” 33.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 230.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 230.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 222.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 407.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 407.
- US Department of Health, Education, and Welfare, Smoking and Health: Report of the Advisory Committee to the Surgeon General of Public Health Service, US Department of Health, Education, and Welfare, Public Health Service (1964): 33
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 230.
- Cummings and Proctor, “The Changing Public Image of Smoking,” 33.
- Markel, “Tracing the Cigarette’s Path.”
- Cummings and Proctor, “The Changing Public Image of Smoking,” 33.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 409.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 409.
- Alberg, Shopland, and Cummings, “2014 Surgeon General’s Report,” 409.
- Teresa A. Rummans, M. Caroline Burton, and Nancy L. Dawson, “How Good Intentions Contributed to Bad Outcomes: The Opioid Crisis,” Journal of Mayo Clinic Proceedings 93 (2018): 345.
- Cummings and Proctor, “The Changing Public Image of Smoking,” 34.
- Rummans, Burton, and Dawson, “Good Intentions,” 345.
- Gardner and Brandt, “The Physician in US Cigarette Advertisements,” 226.
- Celine Gounder, “Who is Responsible for the Pain-Pill Epidemic?” The New Yorker, November 8, 2013, https://www.newyorker.com/business/currency/who-is-responsible-for-the-pain-pill-epidemic.
- Rummans, Burton, and Dawson, “Good Intentions,” 345-346.
- Gounder, “Pain-Pill Epidemic.”
- Mark Barnes, John Giampa, and Minal Caron, “Opioid Prescribing and Physician Autonomy: A Quality of Care Perspective,” Hospital for Special Surgery Journal 15 (2019): 20.
- Gounder, “Pain-Pill Epidemic.”
- Gounder, “Pain-Pill Epidemic.”
- Gounder, “Pain-Pill Epidemic.”
- Rummans, Burton, and Dawson, “Good Intentions,” 348.
- Gounder, “Pain-Pill Epidemic.”
- Rummans, Burton, and Dawson, “Good Intentions,” 344.
Bibliography
- Alberg, Anthony J., Donald R. Shopland, and K. Michael Cummings. “The 2014 Surgeon General’s Report: Commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and Updating the Evidence on the Health Consequences of Cigarette Smoking.” American Journal of Epidemiology 179, no 4. (2014): 403-412. DOI: 10.1093/aje/kwt335.
- Barnes, Mark, John Giampa, and Minal Caron. “Opioid Prescribing and Physician Autonomy: A Quality of Care Perspective.” Hospital for Special Surgery Journal 15 (2019): 20-26. DOI: 10.1007/s11420-018-09666-8.
- Cummings, K. Michael, and Robert N. Proctor. “The Changing Public Image of Smoking in the United States: 1964-2014.” Cancer Epidemiology, Biomarkers & Prevention 23, no. 1 (2014): 32-36. DOI: 10.1158/1055-9965.EPI-13-0798.
- Fisher, Ronald. “Cigarettes, Cancer, and Statistics.” The Centennial Review of Arts & Science 2 (1958): 151-66. http://www.jstor.org/stable/23737529.
- Gardner, Martha N., and Allan M. Brandt. “‘The Doctors’ Choice is America’s Choice’: The Physician in US Cigarette Advertisements, 1930-1953.” American Journal of Public Health 96, no. 2 (2006): 222-232. DOI: 10.2105/AJPH.2005.066654.
- Gounder, Celine. “Who is Responsible for the Pain-Pill Epidemic?” The New Yorker, November 8, 2013. https://www.newyorker.com/business/currency/who-is-responsible-for-the-pain-pill-epidemic.
- Markel, Howard. “Tracing the Cigarette’s Path from Sexy to Deadly.” New York Times (New York, NY), March 20, 2007. https://www.nytimes.com/2007/03/20/health/20essay.html.
- Rummans, Teresa A., Caroline Burton, and Nancy L. Dawson. “How Good Intentions Contributed to Bad Outcomes: The Opioid Crisis.” Journal of Mayo Clinic Proceedings 93, no. 3 (2018): 344-350. DOI: 10.1016/j.mayocp.2017.12.020.
- US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service (1964).
- Wynder, Ernest L., Evarts A. Graham, and Adele B. Croninger. “Experimental Production of Carcinoma with Cigarette Tar.” Cancer Research 13, no. 12 (1953): 855-864. https://www.ncbi.nlm.nih.gov/pubmed/13116124.
ALEXANDRIA SZALANCZY graduated summa cum laude from Centre College and is currently seeking a Ph.D. at Wake Forest University in Winston-Salem, NC. Born and raised in Michigan, she has been interested in genetics from her early high school days and hopes to better understand how our genes impact our health, and how that information may be translated to improve medical treatment.
Spring 2019 | Sections | Doctors, Patients, & Diseases

Leave a Reply